Efficacy of interventions aimed at reducing explicit and implicit weight bias in healthcare students: A systematic review and meta-analysis
Funding information: RSJ was supported by the Research Training Program (RTP) Scholarship, Australian Government, Department of Education. BH was supported by an Australian Research Council Discovery Early Career Researcher Award (DE230100704). Funding sources had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Summary
We conducted a systematic review and meta-analysis to determine the efficacy of interventions aimed at reducing weight bias in healthcare students, and to explore factors that may impact intervention success. A systematic review and random-effects meta-analyses were conducted by including studies that examined the efficacy of weight bias reduction interventions for healthcare students. Of the 3463 journal articles and dissertations screened, 67 studies (within 64 records) met inclusion criteria, with 35 studies included in the meta-analyses (explicit = 35, implicit [and explicit] = 10) and 32 studies included in the narrative synthesis (explicit = 34, implicit [and explicit] = 3). Weight bias interventions had a small but positive impact, g = −0.31 (95% CI = −0.43 to −0.19, p < 0.001), in reducing students' explicit weight bias but there was no intervention effect on implicit weight bias, g = −0.12 (95% CI = −0.26 to 0.02, p = 0.105). There was considerable heterogeneity in the pooled effect for explicit bias (I2 = 74.28, Q = 132.21, df = 34, p < 0.001). All subgroup comparisons were not significant (p > 0.05) and were unable to explain the observed heterogeneity. Narrative synthesis supported meta-analytic findings. The small but significant reduction of explicit weight bias encourages the continued testing of interventions, irrespective of variation in individual intervention components. Contrarily, reductions in implicit weight bias may only be possible from a large societal shift in negative beliefs and attitudes held towards people living in larger bodies.
1 INTRODUCTION
The World Obesity Federation predicts that approximately 51% of people aged ≥ 5 five years will be living with overweight or obesity by 2035.1 An implication of this increase is that most patients of future healthcare professionals will be living with overweight or obesity. Interdisciplinary healthcare teams comprised of, but not limited to doctors, nurses, and psychologists will play a crucial role in addressing not only obesity comorbidities but also psychosocial factors that may be associated with those comorbidities. However, previous research2, 3 highlights that healthcare students hold negative weight-biased beliefs and attitudes towards people living with overweight or obesity that may impede the provision of optimal care to people living in larger bodies.
Weight bias is defined as holding negative beliefs, attitudes, judgments, and assumptions about people living with overweight or obesity.4 Weight bias can be explicit (overt and controllable) or implicit (covert and consciously uncontrollable) and may lead to stigmatizing behaviors (enactment of weight bias) such as making negative verbal remarks towards people living with overweight or obesity and attitudes such as viewing this population as lazy, unintelligent, and unmotivated to improve their health.5, 6 Several studies from across the world have reported weight bias among healthcare students. In a cross-sectional study, Jayawickrama et al found that students from 22 healthcare disciplines across 39 Australian universities held explicit weight biases. Students were fearful of gaining weight, exhibited dislike towards people living with overweight or obesity, held the beliefs that obesity was personally controllable and that people living in larger bodies lacked willpower. Students who identified as male (vs. female) displayed higher of both explicit and implicit weight bias.2 Similarly, Phelan et al reported implicit weight bias among US medical students, similar to their implicit racial bias. Students' explicit weight attitudes were also more negative compared to attitudes towards people from diverse ethnicities and lower socioeconomic statuses.7 Puhl and colleagues found that physician associate, clinical psychology, and psychiatric residency students expressed frustration and pessimism about treating patients living with overweight or obesity. Students who believed obesity to be caused by behavioral (vs. psychological or physiological) factors exhibited more explicit weight bias.8 Finally, in a study of nursing students, 65% incorrectly estimated their absence of implicit weight bias, indicating that a large proportion of healthcare students may be unaware of how their weight-biased attitudes and beliefs may be influencing patient care and outcomes.9
Practicing healthcare professionals have been shown to spend less time with and provide limited health education to patients living with overweight or obesity.10 Health providers have also been shown to blame people living with overweight or obesity for their weight, and excessively attribute presenting concerns to weight gain.11 Evidence from a recent systematic review found that patients living with overweight or obesity may be provided with fewer cancer screenings and less frequent escalation of diabetes treatment, indicating that weight bias exhibited by healthcare professionals may impact their clinical decision-making.12 Experiencing weight stigma from healthcare professionals may lead people living with overweight or obesity to reduce their participation in the healthcare system, whereby they avoid or delay seeking treatment, engage in ‘doctor shopping’, adopt maladaptive coping mechanisms, decrease physical activity, and reduce adherence to recommended treatments.13-15 Sutin and colleagues found that experiencing weight stigma was associated with a 60% increased risk of mortality, independent of common physical and psychosocial contributors, including BMI.16 It is also important to note that even the perception of weight stigma, rather than the direct experience, has also been associated with having increased circulating levels of C-reactive protein, a marker of inflammation linked to the development of cardiovascular disease, diabetes, and depression.17 The consequences of weight stigma could exacerbate overweight, obesity, and other associated conditions, contributing to worse health and quality of life. There is therefore an urgent need to reduce weight bias among healthcare students to ensure that future generations of healthcare professionals are prepared and able to provide impartial support to people living with overweight or obesity.
Recent studies have attempted to ameliorate healthcare students' explicit and implicit weight bias. Several interventions have utilized strategies including education, empathy evoking, and size acceptance to target students' weight bias.18-20 However, existing interventions appear to only reduce explicit biases short-term21-23 and are not efficacious in reducing implicit weight bias.24, 25 Several systematic reviews and meta-analyses have attempted to quantify the efficacy of weight bias reduction interventions for healthcare professionals and trainees. Alberga and colleagues (k = 17) conducted a systematic review to assess the impact of weight bias reduction interventions on healthcare students' and professionals' weight bias and found that interventions were mostly unsuccessful in reducing weight bias among the investigated populations.26 Talumaa et al (k = 25) systematically reviewed the extant evidence to identify strategies to reduce weight bias among healthcare students and professionals and found that studies have mostly used five strategies including increased education, providing information on the causes and controllability of obesity, empathy evoking, weight inclusivity, and mixed methodology.15 Further evidence on the efficacy of weight bias reduction interventions on healthcare students' and professionals' explicit and implicit weight bias combined (k = 9) was extrapolated into a meta-analysis by Moore et al Findings showed that the interventions had a small but positive reduction of weight bias.27 Overall findings from the aforementioned studies indicate partial reductions in negative attitudes and beliefs; however, several methodological limitations must be considered.
Examining the impact of weight bias reduction interventions for healthcare students combined with other populations such as healthcare professionals renders it difficult to establish the efficacy of interventions for healthcare students exclusively, as interventions may have differing impacts for various populations. A decline in empathy has been evidenced among medical students as they progress through medical school, attributable to a demanding workload, greater complexity in patients and their health concerns, and a focus on theoretical understanding.28 A decline in general attitudes towards social issues in medicine was also noted,29 illustrating that healthcare training may be a period of increased openness to changes in attitudes, compared to practicing healthcare professionals who may have strong and established beliefs and attitudes that may be more difficult to change. Consequently, implementing interventions during the formative phase of students' attitudes becomes increasingly vital to foster durable and positive professional behaviors.
However, prior to developing novel weight bias reduction interventions to target students' developing attitudes and beliefs, a rigorous review and analysis of the evidence focused exclusively on healthcare students is needed. Additionally, it is also important to emphasize that while there is an association between explicit and implicit biases, they are separate constructs that need to be independently examined and meta-analyzed.30, 31 Further, the mixed results found within the current literature on intervention efficacy suggest that an in-depth investigation of moderators including delivery method (in-person, online), learning type (active vs. passive), intervention type (unidimensional vs. multifaceted), theoretical framework, and duration (single vs. multiple time points) is needed to determine critical intervention components that may assist in future intervention development.
Recent literature reports the continued existence of explicit and implicit weight bias among healthcare students32, 33 and studies that have attempted to reduce healthcare students' explicit and implicit weight bias have found mixed results, making their combined efficacy unclear. Therefore, this systematic review and meta-analysis aims to address this gap in the literature and will answer the following question: to what extent have previous weight bias interventions been efficacious in reducing healthcare students' explicit and implicit weight biases? This systematic review and meta-analysis will also explore factors that may impact intervention success.
2 METHODS
This systematic review and meta-analysis were conducted according to the Preferred Reporting Items of Systematic Reviews and Meta-Analyses 2020 Statement (PRISMA)34 and the study protocol was prospectively registered with PROSPERO (ID: CRD42020209407).
2.1 Search strategy
The Patient/Population/Problem, Intervention, Comparison and Outcome Framework (PICO)35 was utilized to develop the review question and search strategy (see Section 1 of the supplementary materials). Electronic databases including MEDLINE, PsycINFO, CINAHL, ProQuest, and Web of Science were searched using a combination of search terms (e.g., weight or obesity or overweight or body mass index AND stigm* or discriminat* or phobi* or teas* AND reduc* or interventio* or chang* AND studen* or traine* or medic* or nurs*; see Section 2 of the supplementary materials for the full search strategies applied to the databases). Randomized control trials, quasi-experimental, pilot, cohort, and qualitative studies, dissertations, and feasibility trials that reported pre-post changes of tests of explicit and implicit weight bias reduction interventions were included. Gray literature and pre-print databases (OpenGrey, medRxiv, PsyArXiv, Trove, EThOS, ProQuest Dissertations & Theses Global) were also searched using adaptations of the search terms to identify unpublished manuscripts and dissertations relevant to the inclusion criteria. All searches were limited to English and human participants aged ≥ 17 years. Editorials, comment articles, and case studies were excluded. Reference lists of previous systematic reviews and meta-analyses were also screened to identify additional relevant records. Studies were included from database inception to August 2023, with the initial search conducted on the 5th of February 2022, and updated on the 2nd of August 2023.
2.2 Study selection
Database searches were uploaded to Rayyan, an online study screening tool.36 Authors RSJ and AD independently screened article titles and abstracts according to the inclusion criteria and identified studies for inclusion. Disagreements or uncertainties were resolved by discussion. RSJ then screened the full texts of all articles to be included., while LRE screened the full texts of 10% of the articles. Uncertainties were resolved by discussion and reasons for exclusion and inclusion were validated between the authors.
2.3 Data extraction
Healthcare student population, sample size, objective, design, intervention details, weight bias outcome measures, findings, and future recommendations were extracted from each included study. Means and standard deviations (pre-test and post-test) for explicit outcomes and Cohen's d (d-scores) for implicit outcomes were also extracted for each weight bias outcome, from the intervention group and control/comparison groups. Means and standard deviations were computed from available data when required (e.g., conversion from standard error to standard deviation), and respective authors of studies were contacted when insufficient data were reported. One author (RSJ) conducted the initial data extraction, subsequently confirmed by a co-author (LRE). Additional categorical study characteristics including intervention type (unidimensional vs. multifaceted), theoretical framework, intervention delivery method (in-person vs. online), intervention category (e.g., empathy evoking), intervention duration (single time point vs. multiple time points), and contact with an individual living with overweight or obesity (active vs. passive vs. no contact) were also extracted for subgroup analyses. Additional study characteristics including the percentage of female and male participants were extracted to conduct meta-regressions. Other gender identifications including non-binary were not extracted as they were either not included or represented only a minority of the sample. The primary aims of six studies37-41 were to develop or test the feasibility of interventions in lieu of examining their efficacy. Nonetheless, these were included in the narrative synthesis (and excluded from the meta-analyses due to insufficient data) as they provided applicable information to further the understanding of weight bias interventions.
2.4 Statistical analysis
Comprehensive Meta-Analysis (CMA, version 4.0)42 was used to conduct all statistical analyses. A random-effects model was applied due to the anticipated heterogeneity between studies. Extracted means, standard deviations, and d-scores were used to calculate individual effect sizes (Hedge's g). Effect sizes of studies that administered multiple outcome measures (to assess explicit bias) were pooled, so that each experiment within each study contributed once to the meta-analysis. Similarly, for studies that tested the efficacy of multiple equally weighted weight bias reduction strategies (e.g., social consensus, cognitive dissonance conditions), the sample sizes of control or comparison groups were divided by the respective number of conditions, so that each study contributed one effect size. All individual effect sizes were then pooled together to obtain an average effect size (Hedge's g with 95% Confidence Intervals [95% CI]).43
Studies that reported post-test-only results were excluded from the meta-analyses as it was not possible to quantify intervention effects in the absence of baseline data. Additionally, nine studies reported data for follow-up periods (see Section 3 of the supplementary materials); however, these data points were excluded to maintain the uniformity of the remaining data (pre-test and post-test). Hedge's g, 95% CIs (lower and upper), z, and p-values were used to represent effect size estimates, and Q (with degrees of freedom) and p-values (for Q-value) along with I2 and prediction intervals (PI) were used to examine heterogeneity.43 Outcome measures were classified as beliefs or attitudes (for explicit bias) according to the methodology described by Lee et al (examining the articles that detail the development of the measures and the specific items they contain) who conducted a meta-analysis of weight bias interventions aimed at various populations.44 Sensitivity analyses were carried out by removing studies with CIs that did not overlap with the CI of the pooled effect size, in addition to studies that contained large sample sizes. Publication bias was assessed by visually examining the funnel plot, conducting Egger's regression test, Rosenthal's fail-safe N, Orwin's fail-safe N, and the trim-and-fill method.43 Finally, sub-group analyses and meta-regressions were conducted for explicit and implicit weight bias using study characteristics outlined in the ‘Data extraction’ section.
2.5 Narrative synthesis
Studies excluded from the meta-analyses including those that utilized post-test only and qualitative designs and studies that did not provide the required data to be meta-analyzed were included in the narrative synthesis. Descriptions of studies including their objective, intervention, application, and findings were systematically organized (i.e., in the summary of findings table). Patterns within and between studies including direction and size of intervention impact, and study characteristics were explored and synthesized.
2.6 Study quality assessment
The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE)45 tool was used to individually assess the quality of evidence of the meta-analyzed explicit and implicit bias outcomes. Authors RSJ and LRE applied the GRADE to each outcome independently. Uncertainties or disagreements were resolved by discussion, and consensus was reached to finalize the GRADE for each outcome. The Revised Cochrane Risk of Bias tool for Randomized Trials (RoB 2),46 The RoB 2 for cluster-randomized trials,47 the Risk of Bias in Non-randomized Studies – of Interventions (ROBINS-1)48 and The Joanna Briggs Institute Checklist for Qualitative Research49 were used to assess the risk of bias each study (for studies that used randomization, non-randomization, and qualitative designs, respectively) included in the narrative synthesis. Author RSJ applied the tools to all included studies, while co-author LRE applied the relevant tools to 10% of the included studies. There was 100% agreement between LRE and RJ on ratings of overall risk of bias of the shared studies.
3 RESULTS
3.1 Search results
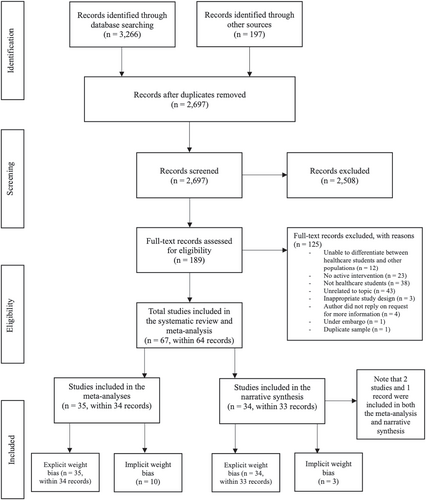
Titles and abstracts of 3463 articles and dissertations were systematically screened (see Figure 1). Sixty-seven studies (contained in 64 records) met the inclusion criteria. Thirty-five studies (within 34 records) provided the required data to be meta-analyzed, while 34 (in 33 records) were included in the narrative synthesis. Two studies24, 25 were included in both the meta-analysis and narrative synthesis. They provided sufficient data for inclusion in the explicit weight bias meta-analysis but not the implicit weight bias meta-analysis. Thus, they were also included in the implicit weight bias narrative synthesis. To facilitate readability, the majority of references to studies described in ‘study characteristics’ are not included in the main text but can be found in Section 3 of the supplementary materials.
3.2 Study characteristics
Sample sizes ranged from 450 to 71851 with a total of 7528 participants. Based on the available demographic details, most participants were women (62%) with a mean age of 22.75 (SD = 3.59) years. Twenty-four studies included psychology students, 17 included medical students, 12 included nursing students, four included students from multiple disciplines (i.e., dietetics, health promotion, medical nursing, and occupational therapy, three included kinesiology students, two from each of the following disciplines: dietetics/nutrition, public health/health promotion, and one from each of the following disciplines: exercise science, marriage and family therapy, and counseling. Sixty-four studies were quantitative with between-subjects (k = 41) and within-subjects (k = 23) designs, and three were qualitative. Among the quantitative studies, 64 examined the efficacy of weight bias interventions on explicit weight biases (i.e., attitudes and beliefs) and 13 examined both explicit and implicit weight biases.
Among the measures used to assess explicit weight bias, 32 used miscellaneous measures, including study-constructed measures, 14 used the Beliefs About Obese Persons Scale (BAOP),52 13 used the Antifat Attitudes Test (AFAT),53 10 used the Fat Phobia Scale (FPS),54 8 studies used the Antifat Attitudes Questionnaire (AFA),55 another eight used the Attitudes Towards Obese Persons Scale (ATOP),52 seven used the Obese Persons Trait Survey (OPTS),56 three used the Universal Measure of Bias-Fat (UMB-FAT),57 two used the Nutrition, Exercise, and Weight Management Attitudes Scale (NEW),38 another two used the Explicit Rating Test (ERT),58, 59 and one used the Nurses' Attitudes Towards Obesity and Obese Patients Scale (NATOOPS).60 Most studies used a combination of measures to assess explicit bias, with only nine33, 38, 50, 51, 61-65 studies having used a single (composite) measure. Among the measures used to assess implicit weight bias, 1218, 19, 22, 24, 25, 66-72 used the Implicit Association Test (IAT)73 and one used a visual probe task.74 A summary of the intervention findings and future recommendations of each study can be found in Section 4 of the supplementary materials.
3.3 Meta-analyses
3.3.1 Explicit weight bias
Thirty-five studies (within 34 records) provided 157 individual effect size estimates for weight-biased attitudes and beliefs. Individual effect sizes were then pooled to obtain a composite effect size of g = −0.31 (95% CI = −0.43 to −0.19, z = −4.98, p < 0.001), indicating that weight bias reduction interventions had a small, but positive effect in reducing students' explicit bias. Results were similar for both beliefs (g = −0.38, z = −3.29, p = 0.001) and attitudes (g = −0.29, z = −5.13, p < 0.001). However, there was significant heterogeneity in the pooled effect, indicating that 74% (I2) of the variance in observed effects was due to variance in true effects rather than sampling error (Q = 132.21, df = 34, p < 0.001). The prediction interval was −0.93 to 0.31; that is, assuming a normal distribution of true effects, the true effect size (in 95% of all comparable populations) could fall between these values. The forest plot can be seen below in Figure 2.

A sensitivity analysis was conducted by independently removing two studies with large sample sizes and seven studies with CIs that did not overlap the CI of the pooled effect size (See Section 5 of the supplementary materials). There were trivial changes in the pooled effect estimates, g = −0.31 and −0.28, indicating that the original pooled effect was not substantially influenced by these factors.
The generated funnel plot was symmetrical (see Section 6 of the supplementary materials) and did not reveal noticeable patterns, and Egger's regression test was not significant (p = 0.798). Rosenthal's Failsafe-N revealed that 815 studies with non-significant results were needed to render the average effect non-significant. Similarly, Orwin's Failsafe-N using −0.10 as the criterion for a trivial Hedge's g revealed that 71 studies were needed to render the average effect trivial. As the funnel plot was symmetric, the trim-and-fill method indicated that zero hypothetical studies were missing from the meta-analysis. Hence, overall, publication bias was not present in this pooled effect. Based on the GRADE45 criteria, the quality of evidence was graded as ‘very low’ (see Section 7 of the supplementary materials).
3.3.2 Implicit weight bias
Eighteen individual effect sizes from 10 studies were pooled to obtain a composite effect size of g = −0.12 (CI = −0.26 to 0.02, z = −1.62, p = 0.105), which indicated that weight bias reduction interventions were not efficacious in reducing students' implicit weight bias. Indicators of heterogeneity (Q = 6.62, df = 9, p = 0.676, I2 = 0.00, PI = N/A) assumed that all studies shared a common effect size, and therefore dispersion of true effects was not observed. See Figure 3 below for the forest plot.
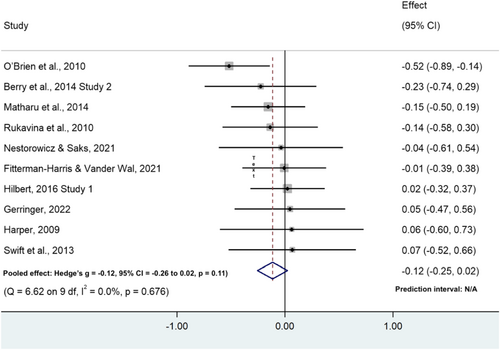
Outliers were not found in the implicit pooled effect, with the CIs of included studies overlapping with the CI of the pooled effect, and all studies included similar sample sizes (mean N = 92.60, SD = 42.36). Sensitivity analyses were therefore not conducted. The generated funnel plot was relatively symmetrical (see Section 6 of the supplementary materials) and Egger's regression test was not significant (p = 0.388). Rosenthal's Failsafe-N indicated that zero studies with non-significant results were needed to render the average effect non-significant. Further, Orwin's Failsafe-N with −0.10 as the criterion value for a trivial Hedge's g indicated that two studies were needed to render the average effect trivial. As the funnel plot was symmetrical, the trim-and-fill method indicated that zero hypothetical studies were missing from the meta-analysis. The results of Rosenthal and Orwin's failsafe-N tests were indicative of publication bias, suggesting that smaller studies with non-significant results were less likely to be published. However, given the symmetrical funnel plot and non-significant Egger's regression test, publication bias was considered impertinent. In accordance with the GRADE45 criteria, the overall quality of evidence was graded as ‘very low’ (see Section 7 of the supplementary materials).
3.3.3 Subgroup analyses
Eight subgroup analyses were conducted for both the explicit and implicit weight bias meta-analyses using the categorical study characteristics of healthcare discipline, intervention type (unidimensional vs. multifaceted), theoretical framework (e.g., Attribution Theory75), delivery method (e.g., in-person), learning type (active vs. passive), intervention category (e.g., education, empathy evoking, education and empathy evoking), intervention duration (single vs. multiple time points), contact with a person living with overweight or obesity during the intervention (active, passive, or no contact), and outcome measure. Between-groups Q tests of variance for each category were non-significant (p > 0.05), suggesting that the investigated subgroups did not account for systematic differences in the size of the effects of both explicit and implicit weight bias. See Section 8 of the supplementary materials for a detailed overview of the subgroup analyses.
3.3.4 Meta-regressions
Two meta-regression analyses using the percentage of participants who identified as men were conducted for the explicit and implicit weight bias meta-analyses. Findings showed that there was a non-significant (p > 0.05) association between participants who identified as men and the pooled effect sizes of both explicit and implicit weight bias. See Section 9 of the supplementary materials for a detailed overview of the meta-regressions.
3.4 Narrative synthesis
3.4.1 Explicit weight bias
Within the 34 studies (in 33 records) that investigated the efficacy of weight bias reduction interventions on explicit bias, the majority (k = 23)35, 37, 39-41, 50, 53, 55, 62, 71, 76-88 reported a partial reduction (a decrease in explicit weight bias on some, but not all outcome measures [including subscales] used in each study) in students' explicit weight bias. Seven studies37, 38, 51, 56, 61, 89, 90 reported a successful reduction in explicit weight bias; however, in two of these studies, when participants' relationship with people living with overweight or obesity37 or positive affect90 was controlled for, the reduction in negative attitudes and less desire to social distance (respectively) was no longer significant, suggesting that the effect was not due to the intervention but due to participant characteristics or exposure. Two studies91, 92 did not find significant reductions in students' explicit weight bias.
Considerable differences in methodology between studies were also noted. Studies differed in their use of outcome measures, intervention type, theory, intervention delivery method, learning type, learning strategy, intervention duration, and contact with people living with overweight or obesity during the intervention (See section 3 of the supplementary materials). Given that most aforementioned studies reported partial reductions in explicit weight bias, it appears that the interventions were only marginally successful in reducing students' explicit weight bias, with notable heterogeneity between studies. Despite the observed small reduction in explicit weight bias, it is important to note that many of the quantitative studies (k = 18 out of 29 studies)37, 40, 41, 53, 55, 56, 62, 71, 76-79, 82, 84-86, 90 employed a post-test-only study design, introducing the risk of bias in terms of study quality, as this prevents comparison between pre and post-intervention explicit weight bias. Indeed, the overall risk of bias for the majority of the included studies was ‘high’ (see Section 7 of the supplementary materials for the risk of bias assessment).
3.4.2 Implicit weight bias
Three studies24, 25, 71 investigated the efficacy of weight bias reduction interventions on implicit weight bias. However, no studies reported a significant reduction. There were considerable differences between the studies including intervention type, theory, intervention delivery method, learning type, learning strategy, intervention duration, and contact with people living with overweight or obesity during the intervention (see Section 3 of the supplementary materials); however, all studies utilized the IAT73 to assess implicit weight bias. Taking these findings together, it can be concluded that study interventions were not efficacious in reducing students' implicit weight bias, with considerable heterogeneity observed between studies on most (but not all) methodologies. Additionally, the overall risk of bias was ‘high’ for the majority of the included studies (see Section 7 of the supplementary materials for the risk of bias assessment).
4 DISCUSSION
This systematic review and meta-analysis aimed to examine the extent to which interventions have been efficacious in reducing healthcare students' explicit and implicit weight biases and explore factors that may impact intervention success. The meta-analyses indicated that interventions reduce healthcare students' explicit weight bias but not their implicit weight bias; findings which were supported by the narrative synthesis. Our findings regarding explicit biases are supported by previous systematic reviews and meta-analyses that also found small reductions in healthcare students' (including other populations) explicit weight-biased beliefs and attitudes.27, 44, 93 The included studies in the current systematic review and meta-analysis examined the efficacy of explicit and implicit weight bias reduction interventions for healthcare students since 1991. However, these interventions have not produced large reductions in weight bias. Recent studies have found that weight-biased attitudes and beliefs remain persistent among healthcare students, with Jayawickrama et al having found the presence of both explicit and implicit weight bias among Australian healthcare students (N = 900) within 22 disciplines,2 and Kerbyson having found that a sample of nursing students and recent nursing graduates (N = 67) engage in ‘fatphobic’ behaviors themselves and observe such behaviors from instructors.94 Nonetheless, the small reduction seen in explicit bias indicates that attempts to reduce students' explicit weight bias are highly relevant and meaningful.
Subgroup analyses and a meta-regression were conducted to examine factors that may impact intervention efficacy; however, analyses did not identify any characteristics that influenced the efficacy of the interventions. Additionally, there was no difference in intervention effects for male and female participants. Subgroup analyses also could not explain the heterogeneity within the explicit bias pooled effect, suggesting that different methodological characteristics between studies may not contribute to variability in the efficacy of weight bias interventions. Unknown factors including individual participant characteristics, confounding variables such as exposure to weight-stigmatizing advertisements, or social desirability may explain the observed heterogeneity. Thomas and colleagues found that the willingness of participants to take part in clinical studies was influenced by feelings of anxiousness or depression, altruism, age, aspects of quality of life, and previous treatment experience.95 Comparatively, participant characteristics of healthcare students such as time commitment, learning ability, personality traits, eagerness to contribute to research, and investment to correctly complete intervention components may have impacted students' willingness to take part in the interventions and thus, influence intervention results. Additionally, several interventions from the included studies in the current review were delivered as classroom curriculums.24, 65, 96-98 It is possible, that participant characteristics such as academic performance may have also influenced intervention results. Further, while all subgroup analyses were nonsignificant, and therefore do not show that one intervention factor may have a greater beneficial effect on reducing weight bias over the others, visual inspection of the effect estimates suggest that multifaceted interventions (intervention type), interventions delivered at multiple time points (intervention duration), and those using active learning methods (learning type; see Section 8 of the supplementary materials for all comparisons) may produce greater reductions in explicit weight bias. However, caution must be exercised when interpreting the effect estimates given the differences in k within each category.
The deeply ingrained nature of weight bias at a societal and cultural level means that healthcare students are continually exposed to weight-biased beliefs, attitudes, and behaviors in many domains of life outside of formal education.99 Evidence has even shown that medical students may observe their instructors engaging in discriminatory behaviors toward people living with overweight or obesity.3 Thus, previous exposure to displays of weight-biased behaviors may confound intervention efficacy. It is appreciated that measuring or controlling for confounding variables may not always be feasible; however, we encourage the use of such procedures where possible. Moreover, as weight bias is a sensitive topic, social desirability (the tendency for participants to respond to measures in a manner that conforms with societal expectations)100 may have impacted students' responses to the outcome measures. Only four out of 35 studies56, 66, 70, 101 included in the meta-analysis assessed social desirability within participant responses, with mixed findings. For example, Puhl et al found that socially desirability responses were unrelated to participants' trait ratings of people living with overweight or obesity at both pre-test and post-test.56 However, Fitterman-Harris and Wander-Val found that after controlling for socially desirability responses, no significant difference in weight bias reduction was observed between the intervention and control group.70 A recent study102 also found mixed results, where the BAOP was not associated with socially desirability responses, but, as AFA scores increased, participants were less likely to respond in a socially desirable manner.
The preceding findings may suggest that students presumed that negative attitudes towards people living with overweight or obesity were the norm, prompting them to report negative attitudes that may not reflect the attitudes they may hold. Given that socially desirable responding was investigated in a few studies with mixed findings, conclusions about the impact of social desirability on intervention efficacy cannot be drawn. Therefore, it is recommended that future studies include measures of social desirability where possible. Overall findings indicate that irrespective of individual intervention components (e.g., theory, duration, learning type), weight bias interventions were efficacious in producing a small reduction of explicit bias.
Contrarily, findings from this systematic review and meta-analysis showed that interventions do not reduce healthcare students' implicit bias; a finding confirmed by the narrative synthesis. Additionally, no variance in true effects was observed. Subgroup analyses and meta-regression were conducted to examine intervention factors that may impact intervention efficacy. However, analyses did not identify any factors that impacted the efficacy of the interventions. There was also no difference in intervention effects for male and female participants. Implicit weight bias is more robust to change compared to explicit weight bias. Reinforcement of social stereotypes is thought to affect the development of implicit bias.103 Shah and Bohlen state that implicit biases may be formed due to past influences and imprints throughout life, and that individuals are unaware of their decision-making being guided by subconscious impressions rather than by factual information and observations.104 Given that these beliefs and attitudes are outside of conscious awareness, they are difficult to access and are therefore harder (if not impossible) to change.72, 73, 105, 106 To note, the majority of studies included in this systematic review and meta-analysis that evaluated implicit weight bias used the IAT. While the measure demonstrates psychometric soundness, several researchers underscore its limitations. These include the strong methodological (vs. theoretical) mechanisms behind the development of the IAT, and the possible association of negativity to the target category (e.g., people living with overweight or obesity) arising from the mere societal awareness of beliefs and attitudes rather than from personal endorsement of those views.107 Schimmack argues that structural equation modeling of multimethod data to examine the construct validity of the IAT found no evidence supporting the claim that IATs measure implicit biases.108 Yet the IAT remains the most common measure to examine implicit weight biases. Future researchers are encouraged to compare IAT results with other measures of implicit bias, such as the Implicit Relational Assessment Procedure (IRAP),109 and the Large Language Model Implicit Bias (LLM)110. However, caution must be exercised when using such tests, as they may also be based on the IAT.109, 110 Further, in their meta-narrative review, Sukhera and Colleagues found that several studies utilized the IAT scores in health professions education to raise awareness and prompt reflection of unconscious biases, a technique used by Geller and Watkins, a practice that future studies should consider adopting.39, 111
Despite the difficulty seen in attempts to reduce implicit bias, research alludes to the importance of both implicit and explicit attitudes on behavior. While explicit attitudes are more strongly associated with intentional behavior, implicit attitudes are more strongly associated with unintentional behavior. Explicit and implicit attitudes may also have a combined effect on certain types of behavior (e.g., voting).112 Hofmann et al suggest that repeated exposure to counter-attitudinal information may be required to ‘rewire’ automatic associations.113 Yet, current findings may indicate the need for more research targeting healthcare students' implicit weight bias, as only 13 out of 67 studies examined the topic. However, it is possible that true reductions in implicit weight bias may only originate from a societal change in beliefs and attitudes. Nevertheless, it may require years, if not decades for a notable shift in societal norms.
At present, weight bias interventions may attempt to teach healthcare students how to suppress their explicit attitudes (and behavior) when interacting with people living with overweight or obesity, as explicit attitudes are more strongly associated with deliberate behavior.112 Such strategies may include training students to use patient-centred communication with person-first language, using non-weight-focused or weight-inclusive approaches rather than focusing solely on weight, and ensuring that medical equipment suitable for those living in larger bodies is readily accessible. It is also necessary for future professionals to include patients in all stages of clinical decision-making, recognize the difficulty of diet and physical activity changes, avoid engaging in stereotypic communication with others about people living with overweight or obesity, and acknowledge that individuals may have had negative experiences in healthcare.91, 114 Awareness must also be raised about the multi-factorial nature of obesity including the wider determinants that demonstrate factors evidenced as causing overweight and obesity including those completely or partially outside of individual control.115 Training students to repress deliberate behaviors may reduce stigmatizing behaviors experienced by people living with overweight or obesity, enabling the provision of fair treatment of, and interaction with, these individuals.
Considering that weight-biased attitudes and beliefs continue to be reported among healthcare students,2, 32, 33 researchers are encouraged to continue the development and testing of weight bias reduction interventions for healthcare students. However, the overall quality of evidence of the meta-analyzed explicit and implicit weight bias outcomes was classified as very low, and the risk of bias of the studies included in the narrative synthesis was high, indicating the presence of many methodological shortcomings, potentially affecting the precision of the reported results. Future studies may consider applying sound methodology (e.g., double-blinding and prospective registration of data-analysis plans) and incorporating the recommendations discussed below. The included weight bias reduction interventions were targeted at healthcare students from 10 disciplines, with psychology being the most common discipline. Although psychology (particularly first-year) students are a readily available population, future interventions are recommended to include students from all relevant healthcare disciplines. It is most likely that care for people living with overweight or obesity will be provided by interdisciplinary teams of healthcare professionals. Therefore, developing and testing the efficacy of weight bias reduction interventions among students from diverse disciplines including physiotherapy, optometry, paramedicine, audiology, dentistry, and medical imaging is crucial. Perhaps delivering weight bias reduction interventions to final-year healthcare students may yield more significant outcomes, considering that many students enrolled in undergraduate healthcare degrees may not pursue future practice.
Additionally, only 1021, 22, 25, 72, 74, 92, 116-118 out of 67 studies included follow-up testing. Several of the studies that demonstrated reductions in explicit weight bias at post-intervention did not sustain these reductions at follow-up. For example, Kushner et al found that medical students' (N = 127) negative obesity stereotypes, empathy towards, and confidence in clinical interaction with people living with obesity improved following an educational intervention. Improvements in empathy and confidence were sustained at follow-up (1 year); however, negative obesity stereotypes reverted to baseline scores.23 Current literature suggests that weight bias reduction interventions may not be efficacious in the long-term. However, it may also suggest that re-exposure to intervention elements is needed between post-test and follow-up periods. Additionally, as students learn many curricula at university, decreases in intervention learning may occur. To further understand the impact of interventions in the longer term, future studies are recommended to include various follow-up periods (e.g., 1 month – 1 year) and determine whether re-exposure to interventions is required to maintain long-term reductions in weight bias. Perhaps integrating weight-bias education in all health-related curricula throughout training (e.g., undergraduate and postgraduate) may invoke positive beliefs and attitudes within students and enable them to perceive those beliefs and attitudes as the norm, consequently reducing their weight-bias long-term. These effects can then be integrated into policies and clinical guidelines to target a broader population. For instance, under the Equal Opportunity Act, discrimination against physical features including weight is prohibited in work, education, sporting or social organization, retail, aged care, and accommodation settings in the state of Victoria in Australia.119 This legislation could be applied to healthcare settings nationally, and potentially globally over time. Based on the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework used to inform the development and evaluation of programs, Holtrop and Colleagues state that long-term maintenance of programs (i.e., interventions) at both the individual and institutional levels may include providing ongoing feedback to participants, referral to community resources, and peer support, as well as incorporating programs into organizational practices and policies.120 Individual-level interventions combined with broader societal-level actions may offer considerable potential to reduce weight bias, particularly in the long-term.
Although the studies included in this review demonstrated a small reduction in students' explicit bias, it is unclear whether this reduction translates to actual behavior towards people living with overweight or obesity. According to the Theory of Planned Behavior,121 both beliefs and attitudes influence behavior.122 Therefore, future studies are recommended to assess the impact of interventions on healthcare students' stigmatizing behavior. Assessing students' actual behavior may be crucial to gauging their anticipated interactions with those living in larger bodies in future practice. However, it is appreciated that including objective measures of behavioral assessment may not be consistently feasible, particularly in online interventions. Moreover, the majority of the included studies utilized explicit measures of weight-biased beliefs and attitudes targeted toward the general population of individuals living with overweight or obesity. Few studies employed measures designed to examine students' beliefs and attitudes towards caring for patients living with chronic conditions (e.g., NATOOPS,118 and empathy for and confidence in clinical interaction with patients living with overweight or obesity23). Perhaps it may be necessary to develop a comprehensive measure that evaluates students' beliefs and attitudes towards providing care (or their intention to care) for these patients before examining whether changes in weight bias translate into practice.
The primary strengths of this systematic review and meta-analysis are the inclusion of weight bias reduction interventions targeted at all relevant (and available) healthcare student disciplines, the inclusion of both a meta-analysis and narrative synthesis, and the exploration of the possible factors that may impact intervention success. However, limitations must also be considered. Despite the application of a thorough search strategy, it is possible we did not find and include all eligible studies, including studies not published in English. Incorporating studies written in other languages (and culturally diverse samples) may strengthen the evidence of future systematic reviews and meta-analyses.
4.1 Conclusion
Interventions to reduce weight bias aimed specifically at healthcare students had a significant lowering effect on explicit weight bias, whereas implicit weight bias was unchanged. There was no effect of variations in intervention delivery method, intervention type, and theoretical framework utilized. Overall findings signify the need for more robust weight bias reduction interventions for healthcare students, including recruiting students from all available healthcare disciplines when testing interventions and assessing intervention effects at various follow-up periods. However, substantial shifts in societal attitudes may be required to produce notable changes (and maintenance of those changes) in implicit weight bias.
ACKNOWLEDGMENTS
We thank Ms Vanessa Varis, the Faculty of Health Sciences and Vice-Chancellory Librarian at Curtin University for her guidance in the development of the literature search strategy and navigation of electronic databases. We also thank Dr Michael Borenstein, lead author of the text Introduction to Meta-Analysis and the developer of Comprehensive Meta-Analysis (CMA) software for his guidance with CMA and the meta-analysis procedure. Open access publishing facilitated by Curtin University, as part of the Wiley - Curtin University agreement via the Council of Australian University Librarians.
CONFLICT OF INTEREST STATEMENT
SWF reports research grants and support for attending meetings from UK National Institute for Health Research, UK Office of Health Improvement & Disparities, UK Doncaster Council, Novo Nordisk, Johnson & Johnson, University of Leeds UK, UK Parliament, UK Safefood, Novo Nordisk Foundation, and Diabetes Ireland Congress and Exhibition. EH reports receiving royalty fees for a book published on the topic of weight stigma. All declared interests relate outside the submitted manuscript. RSJ, BH, MO, LRE, XD, and BJL declare no competing interests.
Open Research
DATA AVAILABILITY STATEMENT
Data will be made available upon request to author RSJ for non-commercial purposes to individuals associated with academic or public research and health institutions.




