Cardioembolic stroke in the cardiac variant of Fabry disease
Abstract
We describe herein the case of a 71-year-old man with the cardiac variant of Fabry disease presenting with cardioembolic stroke. Stroke is one of the most well-known manifestations of Fabry disease, and lacunar stroke is a widely recognized etiology. However, little is known about stroke in patients with the cardiac variant of Fabry disease. The cardiac variant of Fabry disease should be considered as a potential cardiac source of embolic stroke.
Introduction
Fabry disease is an X-linked lysosomal storage disorder resulting from deficiency of α-galacctosidase A (α-GLA) activity that predominantly affects the peripheral nervous system, skin, heart, kidneys, eyes and vascular endothelium. Two variants of Fabry disease with manifestations selectively involving the heart (cardiac variant of Fabry disease [CVFD]) or kidney (renal variant of Fabry disease) have been reported. CVFD typically presents as a late-onset disorder primarily limited to the heart, leading to hypertrophic cardiomyopathy (HCM) and arrhythmias, including non-sustained ventricular tachycardia (NSVT) and atrial fibrillation (AF). No involvement of the vascular endothelium or other organs is seen.1 Although the incidence of Fabry disease has been estimated as approximately one in 30 000–40 000, that of CVFD has been reported as one in 1600 based on recent epidemiological data.2 We could thus encounter stroke events more frequently in CVFD patients than in patients with Fabry disease. However, little is known about stroke in patients with CVFD. We describe herein the case of a patient with CVFD who presented with HCM and cardioembolic stroke.
Case report
A 71-year-old man presenting with aphasia was admitted to the National Cerebral and Cardiovascular Center, Suita, Japan. He had a history of HCM at 52 years-of-age. Fabry disease was diagnosed based on the very low level of α-GLA activity in lymphocytes at 70 years-of-age. He did not receive enzyme replacement therapy (ERT). There was no family history of cardiac disease, renal disease, stroke or Fabry disease.
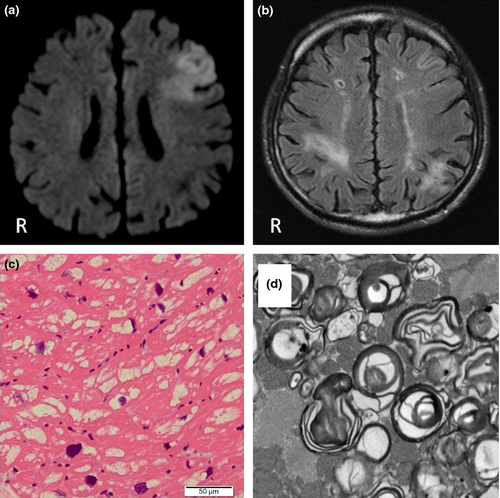
On admission, neurological examination showed mutism without paralysis. No skin or corneal symptoms were evident. An acute infarct in the left frontal lobe was identified on diffusion-weighted imaging (Fig. 1a). Fluid-attenuated inversion recovery imaging showed old infarcts in bilateral parietal lobes and the right centrum semiovale (Fig. 1b). Findings on intracranial magnetic resonance angiography and carotid ultrasonography were normal. Electrocardiography showed sinus rhythm, and NSVT was the only arrhythmia detected on Holter electrocardiography. Echocardiography showed global reduction in left ventricular systolic function with an ejection fraction of 15%. Severe stenosis of the proximal left coronary artery was found on coronary angiography. Right ventricular endomyocardial biopsy showed extensive vacuolar degeneration in histology and lamellar bodies in an electron micrograph compatible with Fabry disease (Fig. 1c,d). The level of the N-terminal of prohormone brain natriuretic peptide was 1443 pg/mL on blood testing. Estimated glomerular filtration ratio was 64 mL/min/1.73 m2, and urinalysis showed no proteinuria. GLA activity in lymphocytes was 1.2 nmol/mg/protein/h (normal 49.8–116.4 nmol/mg/protein/h). We detected, in this patient, the mutation c.758 T > C in the exon 5 of the GLA gene, which caused the amino acid substitution I253T in the protein.
Cardioembolic stroke was diagnosed. Anticoagulation therapy with warfarin was indicated, but not ERT. Cardiac resynchronization therapy defibrillators were implanted 1 month after stroke onset. Sensory aphasia remained at discharge, 2 months after stroke onset.
Discussion
Fabry disease is an important cause of stroke in young adults. Lacunar stroke is a well-known etiology among patients with Fabry disease, because deposition of glycosphingolipids occurs in the vascular endothelium and smooth muscle cells.3 In contrast, patients with CVFD are likely to develop cardioembolic stroke resulting from arrhythmias, valvular heart disease and HCM. Ooka et al.4 reported ventricular hypertrophy, AF and subsequent cardioembolic stroke in a 57-year-old woman with a family history of Fabry disease. Cardioembolic stroke can be a common event in elderly patients with Fabry disease, including CVFD.
We thought that our patient might be at high risk of stroke recurrence because of the presence of multiple old cortical infarcts. We therefore initiated anticoagulant therapy with warfarin for secondary prevention of cardioembolic stroke. Nakamura et al.5 reported three patients with Fabry disease who developed hemorrhagic stroke, concluding that degeneration of the cerebral small arteries secondary to deposition of glycosphingolipids and aging, in addition to hypertension and antithrombotic/anticoagulant agents, was contributing to the risk of hemorrhagic stroke in these patients. More attention should therefore be paid to prevention of not only ischemic stroke, but also hemorrhagic stroke in patients with Fabry disease receiving anticoagulant therapy.
Patients with Fabry disease occasionally suffer from sudden cardiac death.6 Although reports describing implantation of cardiac resynchronization therapy defibrillators for Fabry disease have been limited, our patient with NSVT received cardiac resynchronization therapy defibrillators to prevent sudden cardiac death.6-8
ERT in addition to ordinary secondary prevention is recommended in patients with ischemic stroke and Fabry disease.9 However, the effectiveness of ERT in preventing stroke recurrence has not been confirmed, particularly for patients with CVFD and stroke. Pieroni et al. reported that patients with Fabry disease and myocardial fibrosis from HCM, as in the present case, receive only limited benefit from ERT, and that treatment should be started before myocardial fibrosis has developed, to achieve at least a stabilization of cardiac involvement.10
In conclusion, Fabry disease, particularly CVFD, should be considered as a cardiac source of embolic stroke in elderly patients.
Acknowledgments
We are grateful to Dr Hitoshi Sakuraba, Department of Clinical Genetics, Meiji Pharmaceutical University, Tokyo, Japan. This study was supported in part by JSPS KAKENHI Grant Number 24591309. The authors declare no conflict of interest.