Biliary protozoa in a dog with acute cholangiohepatitis fed a raw food diet
Abstract
A 1-year 11-month intact female Alaskan Malamute fed a raw food diet was referred to the Queen Mother Hospital for Animals for further investigation of hyporexia and increased hepatobiliary enzyme activities. Clinicopathological and imaging findings were consistent with cholangiohepatitis, with coccidial zoites identified on bile cytology. Polymerase chain reaction and amplicon sequencing from the bile identified Hammondia heydorni, a Sarcocytid coccidial protozoa with an obligate 2-host life cycle. The dog was treated with clindamycin, marbofloxacin, ursodeoxycholic acid (UDCA) and S-adenosylmethionine/silybin with complete clinical and biochemical resolution documented after 6 weeks. Infection with Hammondia spp. should be considered in patients receiving raw food diets in which coccidial zoites are identified in the bile, but the pathogenic potential of this organism is unknown and the possibility of its presence as a commensal cannot be discounted.
1 INTRODUCTION
Hammondia heydorni is a cyst-forming coccidian parasite with a 2-host life cycle. Definitive host infection occurs by ingestion of an intermediate host.1, 2 Little is known about the pathogenicity of the Sarcocystid coccidian protozoa H. heydorni in dogs, but diarrhea is the most frequently reported clinical sign in clinical cases.3, 4 Other Sarcocystid coccidian protozoa have been associated with hepatitis in dogs,5, 6 with the presence of Hammondia species identified in bile from a dog with acute hepatitis7 and Isospora spp. also documented in canine bile,8 but the clinical relevance of these biliary protozoa is unclear.
We report the first case in which coccidial zoites of H. heydorni have been documented in the bile of a dog that was fed raw food with clinical, clinicopathological and imaging findings consistent with cholangiohepatitis.
2 CASE DESCRIPTION
A 1-year 11-month, intact female Alaskan Malamute presented for further investigation of hyporexia, pigmenturia and increased hepatobiliary enzyme activities identified before referral. The dog had no history of travel outside of the United Kingdom and was fed a commercial raw food diet. On presentation, physical examination disclosed icteric sclera, mild cranial abdominal discomfort, and an increased body condition score of 8/9, but was otherwise unremarkable. Initial investigations included a CBC, serum biochemistry profile and abdominal ultrasonography. The CBC identified a mild neutrophilia (14.22 × 109/L; reference interval, 3.5-11.5 × 109/L) with reactive lymphocytes. Serum biochemistry documented markedly increased alkaline phosphatase (ALP) activity (6232 U/L; reference interval, 0-130 U/L), alanine aminotransferase (ALT) activity (2481.6 U/L; reference interval, 19.8-124 U/L), total bilirubin concentration (59.9 μmol/L; reference interval, 0.1-4.2 μmol/L) and C-reactive protein (CRP) concentration (121.3 mg/L; reference interval, 0-10 mg/L) along with mild increases in cholesterol concentration (11.95 μmol/L; reference interval, 3.2-6.2 μmol/L) and creatine kinase (CK) activity (677 U/L; reference interval, 67-446 U/L), and a mild decrease in urea concentration (2.4 mmol/L; reference interval, 3.1-10.1 mmol/L). Leptospira microscopic agglutination testing (MAT) was not consistent with active leptospirosis and urine PCR was negative for leptospires.
Abdominal ultrasonography identified mildly heterogenous liver parenchyma with mild rounding of the right liver margins, moderate dilatation of the common bile duct with hyperechoic mildly thickened walls, mild hepatic lymphadenopathy and a scant amount of peritoneal fluid adjacent to the gallbladder. Fine needle aspirates (FNA) of the liver and cholecystocentesis were performed without complication.
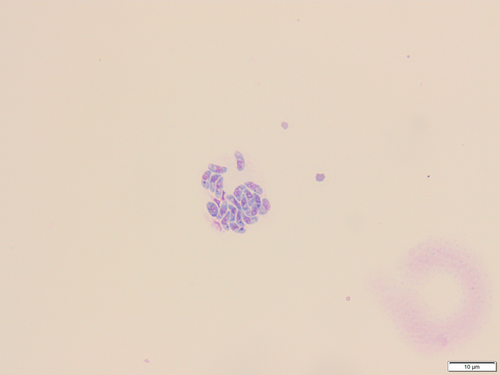
Liver FNA identified moderate numbers of segmented neutrophils seen focally throughout hepatocyte clusters, high numbers of hepatocytes containing lipid vacuoles, and moderate numbers of bile casts, findings consistent with neutrophilic inflammation, vacuolar degeneration (lipid type) and cholestasis. Bile cytology on both direct and cytocentrifuged preparations documented low to moderate numbers of crescent-shaped zoites with light to moderate blue cytoplasm and central to pericentral nuclei, both individually and in clumps (Figure 1). Bile culture failed to identify any bacterial isolates. After cytological identification of coccidial zoites, serology for Toxoplasma and Neospora was performed. Toxoplasma Immunoglobulin M (160; reference interval, <20) and Immunoglobulin G (>800; reference interval, <50) titers were strongly indicative of exposure, as was Neospora serology (Immunoglobulin G immunofluorescence >1600; reference interval, <100). The PCR of the patient's bile however was negative for Toxoplasma and Neospora (Langford Veterinary Services, Bristol, UK). The dog was treated with a 4-week course of marbofloxacin (3.89 mg/kg q24h PO [Marbocyl, Vetoquinol, UK]), a 4-week course of clindamycin (31.2 mg/kg q12h PO [Antirobe, Zoetis, USA]), a 4-week course of ursodeoxycholic acid (UDCA; 11.7 mg/kg q24h PO [Destolit, Norgine, UK]), a 4-week course of S-Adenosylmethionine/Silybin (16.6 mg/kg q24h PO [Denamarin, Protexin, UK]) and it was recommended to transition the dog onto a commercial cooked hydrolyzed protein diet and to reassess the dog in 4 weeks. One week after presentation, repeat CBC was normal and serum biochemistry indicated marked improvement in ALP (3045 U/L; reference interval, 0-130 U/L) and ALT (818.3 U/L; reference interval, 19.8-124 U/L) activities, and total bilirubin (7.5 μmol/L; reference interval 0.1-4.2 μmol/L) and CRP (18.4 mg/L; reference interval 0-10) concentrations, but these results had not normalized. The patient's hyporexia and pigmenturia had resolved. At 6 weeks, repeat CBC and serum biochemistry documented complete resolution of the patient's previously increased ALP (109 U/L; reference interval, 0-130 U/L) and ALT (52 U/L; reference interval, 19.8-124 U/L) activities and total bilirubin (2.9 μmol/L; reference interval, 0.1-4.2 μmol/L) and CRP (0.6 mg/L; reference interval, 0-10 mg/L) concentrations and the owner reported no clinical concerns.
3 MOLECULAR IDENTIFICATION OF H. HEYDORNI
Total genomic DNA was extracted from bile using a Qiagen DNeasy Blood & Tissue kit as recommended by the manufacturer (Qiagen, Hilden, Germany). Polymerase chain reaction followed by amplicon sequencing targeting coccidial 28S ribosomal DNA (rDNA) was performed using the primers KL-P1Fa (5′-TACCCGCTGAACTTAAGCAT-3′) and KL-P2Rb (5′-TGCTACTACCACCAAGATCTGC-3′) as described previously.9 Sequences were manually curated using CLC Main Workbench (version 8.0.1) and annotated following comparison using BLASTn (https://blast.ncbi.nlm.nih.gov/Blast.cgi), identifying H. heydorni by comparison with GenBank reference sequence AF159240 (100% query coverage, 99.79% identity).10 The consensus sequence is available under GenBank accession number ON738675.
4 DISCUSSION
This case is the first report of H. heydorni identified in the bile of a dog presenting with clinical signs, clinicopathological features and imaging findings consistent with acute cholangiohepatitis. A single report exists describing biliary Hammondia spp. in a dog with acute hepatitis,7 but the previous study could not differentiate between H. heydorni or Hammondia triffittae.
Sarcocystidae species have been described as a causative factor in hepatitis affecting companion animals, namely Toxoplasma in cats, and Sarcocystis and Neospora in dogs. Hammondia was historically not believed to be associated with disease in dogs, but recent literature suggests this organism may be an emerging pathogen.1, 3, 4 Hammondiasis has been reported infrequently, often is associated with diarrhea,4, 11 and has been identified in dogs fed raw meat.11 Infection secondary to feeding a raw meat diet in the dog described here would be compatible with the obligate 2-host life cycle of Hammondia,2 with small rodents and ruminants usually acting as intermediate hosts, and dogs and other canids as definitive hosts in natural infection. Further evidence supporting the fact that consumption of a raw meat diet could have led to infection in the dog described here is that H. heydorni-like oocysts have been documented in the feces of dogs fed musculature of infected cattle, sheep, goats, roe deer, and other herbivores.2
Feeding of raw diets is a rapidly growing trend with substantial concern regarding both the development of food-borne disease in pets and the risk to humans handling raw food products and in contact with animals fed such diets and their environment.12 Several dangerous pathogens with zoonotic capacity have been identified in commercial raw food diets and raw meat, including extended-spectrum β-lactamase producing Enterobacterales, Salmonella species, Clostridium perfringens and several other bacterial and protozoal pathogens.12-15 Biliary H. heydorni in the dog described here may represent a novel unusual infectious disease related to feeding of raw meat, but both the source of infection and the pathogenicity of H. heydorni in our case cannot be definitively proven.
A previous report in which Hammondia species were identified in the bile of a dog with acute hepatitis is similar to the case presented here,7 in which marked increases in ALP and ALT activities were evident along with cytologic evidence of hepatic neutrophilic inflammation and biliary coccidial zoites. However, a limitation of the former report was the inability to distinguish H. heydorni from H. triffittae. Both the aforementioned case and our case had biochemical and clinical resolution after treatment, having both received clindamycin, S-Adenosylmethionine/Silybin and a fluoroquinolone. Ursodeoxycholic acid was utilized in our dog for its cholerectic action,16 given the ultrasonographic and biochemical evidence of cholestasis.
Interestingly, serology for Toxoplasma and Neospora were positive in both our dog and in another report7 despite negative PCR, and subsequent identification of Hammondia. This finding suggests a likely degree of cross-reactivity in canine assays between Sarcocystidiae species, similar to what has been observed in ruminants and rodents.17-19
It is not possible to conclude that hammondiasis was a definitive contributing factor to the cholangiohepatitis in our case, and clinical improvement could be attributed to treatment with marbofloxacin, ursodeoxycholic acid or S-Adenosylmethionine/Silybin or to spontaneous resolution, rather than resolution of hammondiasis secondary to treatment with clindamycin. A limitation of our report is that repeat cholecystocentesis to document persistence or resolution of Hammondia was not performed. It is possible Hammondia may have been incidentally detected as a commensal organism that refluxed into the bile from the intestine, was present as an opportunistic pathogen secondary to concurrent disease, or could indeed have acted as a primary causative pathogen. Despite this uncertainty, identification of biliary protozoa is a rarely reported and interesting finding, and ours is the first report of definitively identified H. heydorni in canine bile.
Clinical and clinicopathological resolution was achieved in this dog with normalization of bilirubin concentration and hepatobiliary enzyme activities 44 days postdiagnosis. Repeat cholecystocentesis was not performed to confirm absence or persistence of H. heydorni because of lack of benefit in a clinically healthy patient.
To conclude, we describe the first report of confirmed H. heydorni in bile of a dog fed a raw food diet with suspected cholangiohepatitis. This case adds to the body of evidence surrounding H. heydorni as an emerging organism of interest, although the clinical relevance of identification of this Sarcocystid organism in this case is unknown.
ACKNOWLEDGMENT
No funding was received for this study.
CONFLICT OF INTEREST DECLARATION
Authors declare no conflict of interest.
OFF-LABEL ANTIMICROBIAL DECLARATION
Authors declare no off-label use of antimicrobials.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Authors declare no IACUC or other approval was needed.
HUMAN ETHICS APPROVAL DECLARATION
Authors declare human ethics approval was not needed for this study.