Child sleep problems, maternal sleep and self-efficacy: Sleep's complicated role in maternal depression
Summary
Depression, poor sleep duration and low self-efficacy are common in mothers of children with sleep problems. However, research rarely extends beyond the postpartum period. This study investigated the multifaceted relationship between child sleep and maternal depression in early motherhood. A confidential survey assessed child sleep problems, maternal sleep duration, parental self-efficacy and depressive symptoms in 477 Australian mothers of children aged 3 months to 5 years. We found no relationship between child age and maternal depression, supporting our decision to look beyond postpartum depression. Robust bootstrapped mediation modelling tested the hypothesis that both maternal sleep duration and parental self-efficacy would mediate child sleep problems as predictors of maternal depression. After controlling for child age, results showed a significant parallel mediation effect, demonstrating that maternal sleep duration and parental self-efficacy both mediate the relationship between child sleep problems on maternal depression. While the total effect of child sleep problems on maternal depression was statistically significant, after partialling out the effects of other variables, child sleep problems no longer predicted maternal depression. Akaike information criterion analyses supported the full model, with both mediators explaining meaningful variance in maternal depression. This study expands our knowledge beyond the postpartum period, and divulges the disparate effects of sleep deprivation and parental self-efficacy on the relationship between child sleep and depression in early motherhood. Maternal sleep duration and self-efficacy are modifiable risk factors of maternal depression, indicating possible efficacious treatments. Parental self-efficacy stands out as a direction for clinical practice and further psychobiological study.
1 INTRODUCTION
Child-rearing stressors, such as child sleep problems, may predispose mothers to depressive symptomology in early motherhood (Hiscock & Wake, 2001; Karraker & Young, 2007). An Australian cross-sectional study (N = 10,090) estimated about 17% of infants and 14% of preschool-aged children experience sleep problems (Martin et al., 2007). Poor child sleep is positively correlated with poor maternal sleep (Kalmbach et al., 2021). In a cross-cultural study of mothers with children under 6 years of age (n = 10,085), 26% of mothers reported sleep duration ≤ 6 hr (Mindell et al., 2013). Price et al.'s (2012) Australian study found that 40% of mothers of children with a sleep problem during the first year of life exhibited clinical levels of depression. However, maternal depression and sleep duration may impact the mother's impression of her child's sleep (Halal et al., 2020). Thus, the pathway from child sleep problems to parental depression is not straightforward. Here, we examined a more complicated set of child and maternal variables, and their impact on maternal depression.
Parental self-efficacy is the subjective belief a parent holds regarding their ability to successfully perform their role as a parent (Bandura, 2006). In mothers of children with sleep problems, repeated unsuccessful settling attempts can reduce parental self-efficacy (Leahy-Warren & McCarthy, 2011; Wolfson et al., 1992). Low parental self-efficacy has been identified as a risk factor for maternal depression in Australian mothers (Giallo et al., 2013; Howell et al., 2009; Kohlhoff & Barnett, 2013; Leahy-Warren & McCarthy, 2011). Werner et al. (2022) found that higher parental self-efficacy was related to fewer child sleep problems. Poor parental self-efficacy is related to depressiogenic schema through negative self-evaluation and feelings of worthlessness (Jones & Prinz, 2005), which may be exacerbated by poor sleep duration. Previous studies found that the association between child sleep and maternal depression was mediated by maternal sleep duration in postpartum populations (Hairston et al., 2016; Meltzer & Mindell, 2007).
Child sleep problems that endure throughout early childhood may have exacerbated effects. Tikotzky and Shaashua's (2012) study of 71 mother–child dyads found that more frequent night-waking at 12 months predicted higher problematic sleep by age 4 years. Lam et al.'s (2003) longitudinal study of 114 children aged 8–10 months and again aged 3–4 years revealed that night-waking remained common and depression severity remained significantly higher in mothers of children with sleep problems in infancy.
Behavioural sleep intervention studies aimed at improving child sleep outcomes have also enhanced maternal sleep duration (Lewis et al., 2018), parental self-efficacy (Heerman et al., 2017; Kohlhoff & Barnett, 2013), and reduced maternal depressive symptomology (Goldberg et al., 2013; Kohlhoff & Barnett, 2013). While these intervention studies have narrow age inclusions, they cumulatively accentuate the multifaceted relationship between child sleep and maternal depression.
Previous studies provided support for child-driven (Ystrom et al., 2017), maternal-driven (Teti & Crosby, 2012) and bidirectional models (Dias & Figueiredo, 2021). However, research was limited by narrow age ranges and variables. Ystrom et al.'s (2017) longitudinal study of 959 children up to age 4 years found a significantly larger effect for child-driven processes than mother-driven processes, while Dias and Figueiredo's (2021) study of 312 mother–infant dyads up to 6-months postpartum found support for a bidirectional relationship between infant unsettled sleep and postpartum depression symptoms. They hypothesized that this relationship may be explained by the effects of maternal sleep, fatigue and self-efficacy.
In this study, we investigated a unidirectional child-driven model (Ystrom et al., 2017) hypothesizing that child sleep problems impact maternal sleep duration, and decrease maternal self-efficacy, thus leading to the emergence of depressive symptoms. However, ordering variables in cross-sectional, or even longitudinal, studies always includes a degree of subjectivity (Agler & De Boeck, 2017). As we predict both maternal sleep problems and paternal self-efficacy will mediate the relationship between child sleep problems and maternal depression, we chose a parallel model. Evidence suggests that child sleep problems should predict lower maternal nocturnal sleep duration (Kalmbach et al., 2021) and lower self-efficacy (Werner et al., 2022). Mothers' sleep duration and parental self-efficacy are hypothesized to negatively predict depressive symptoms. Further, we tested this model on mothers of children up to 5 years old.
2 METHODS
2.1 Design
The current study is a secondary analysis of data collected to develop a screening questionnaire for an mHealth sleep program for parents with sleep and settling difficulties. Ethics approval was obtained from Sydney Local Health District (X19-0069), and Charles Sturt University (H21115). Analyses were conducted with R, 4.2.2 (R Core Team, 2022), robmed package for robust bootstrapped mediations (Alfons et al., 2022), the coefficientalpha package for bootstrapped omegas (Zhang & Yuan, 2016), and AICcmodavg for AIC model comparisons. Analyses were bootstrapped (5000 iterations) to allow better generalization of results (Bland & Altman, 2015). R code and full results are available at: https://osf.io/wsn4r/.
2.2 Procedure
The study recruited parents of infants and children who experienced difficulties with sleep. This recruitment was based on parents’ perceived experience of infant and child sleep; however, their infant or child may or may not have actually had an objective sleep problem (as defined by the frequency and duration of any nocturnal sleep-related behaviours that are commonly used as criteria for the presence of a childhood “sleep problem”; Sadeh, 2004). The survey was publicly advertised on social media networks (e.g. Facebook and LinkedIn). Participants received an information statement detailing anonymity, and participants provided consent by commencing the survey. The survey took approximately 30 min to complete. Participants were then directed to an exit page that contained a supporting statement with helpline contacts (e.g. Tresillian parent advice helpline). Participants were invited to enter a prize draw for a $100 gift voucher drawn at random. Identifiable information was collected separately to protect participants' privacy and were excluded from the present dataset.
3 MEASURES
3.1 Maternal depression
Participants completed the Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987). The 10-item self-report measure assesses the past 7 days symptoms of depression. The EPDS is scored on a four-point scale, with sum scores ranging from 0 to 30. The current study performed principal axis factor analysis, revealing a single factor nine-item scale explaining 53.0% of common variance. Item 10, “the thought of harming myself has occurred to me”, was removed due to low correlations, communalities and factor loading. The EPDS-9 demonstrated good internal consistency in the present study (ω = 0.89, 95% confidence interval [CI] [0.87, 0.90]). Sum scores ranged from 0 to 26 out of a possible 0–27 (M = 7.96, SD = 4.78). To apply popular cut-off scores for mild depression, we used the full EPDS-10; however, for all other analyses we used continuous scores of the EPDS-9.
3.2 Parental self-efficacy
The four-item self-efficacy subscale from the Me as a Parent scale (MaaP-SE; Hamilton et al., 2015) measured mothers' perceptions of their parenting self-efficacy (e.g. “I know I am doing a good job as a parent”) on a five-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate higher parental self-efficacy, with a possible range of 4–20. The current study found moderate internal consistency (ω = 0.86, 95% CI [0.84, 0.89]). Sample scores ranged from 8 to 20 (M = 15.68, SD = 2.34).
3.3 Maternal sleep duration
Mothers reported their average sleep duration over the past month via a single question: “how much sleep do you have most nights?”. Higher maternal sleep duration (MSD) scores indicated higher nocturnal sleep duration. Scores in this study ranged from 2 to 9 hr. Scores were interpreted in accordance with the US National Sleep Foundation's recommendations of 7–9 hr for adult sleep duration (Hirshkowitz et al., 2015). As there were no indications of excessive sleep in the sample, higher MSD scores indicate better sleep quality.
3.4 Child sleep problems
The Brief Infant Sleep Questionnaire (BISQ; Sadeh, 2004) is a 13-item parent-report questionnaire of sleep difficulties and demographics pertaining to the child. Individual items measure sleep-onset (minutes), nocturnal and diurnal sleep duration (hours), child waking (frequency), nocturnal wakefulness (duration), and the mother's perceived severity of the sleep problem. The current study created total scores based on recommended cut-offs that have been validated against objective sleep actigraphy and sleep diaries: waking frequency > 3, nocturnal wakefulness > 1 hr, total sleep duration < 9 hr (Sadeh, 2004). While the BISQ was not validated in children above 36 months, it provides descriptive information and, according to normative data (Paavonen et al., 2020), the cut-off scores would apply to children above 36 months as waking and wakefulness should decrease with age, whilst sleep duration increases. Binary categories were created for each variable. A score of 1 was provided if participants exceeded these thresholds. The three items were then summed, with scores ranging from no problem (0), a minor problem (1), a major problem (2), and a severe problem (3).
4 RESULTS
4.1 Participants
Participant inclusion criteria were restricted to Australian mothers of healthy children aged 3 months to 5 years, with English language proficiency, internet access, and willingness to complete at least one questionnaire on child–parental factors. The sample included 477 mother–child dyads with a 78.8% completion rate. Child's age ranged from 3.00 to 59.73 months (M = 17.54, SD = 13.99). There were 213 under 12 months old, 128 aged 1–2 years, and 136 aged between 2 and 5 years. Mother's age ranged from 19 to 49 years (M = 33.22, SD = 4.27). The majority of women in this sample were from one Australian state, New South Wales (87.4%), married (82.8%), primiparous (70.4%) and well-educated (68.2% completed a university degree or higher), while 47.2% reported currently working. However, 8.5% of participants had children born prematurely, and 7.7% stated their child was off track with their developmental milestones. Those cases were retained as they were not deemed influential in multivariate outlier checks.
4.2 Preliminary analyses and descriptive statistics
For this study, we measured indicators of maternal depression (i.e. EPDS scores). However, we reference various criteria for comparison purposes. For this sample, 38.4% of mothers reported EPDS-10 scores ≥ 9, a level that Cox et al. (1996) suggested indicates significant depressive symptoms. Using a more conservative cut-off score of ≥ 13 to avoid false negatives, as recommended by Levis et al. (2020), 17.6% of mothers likely meet the diagnostic criteria of major depressive disorder. In this study, 52.6% of mothers had < 7 hr sleep per night on average. In line with recommended interpretations of sleep problems (Sadeh, 2004), 18.8% of children had < 9 hr sleep, 22.4% woke more than 3 times per night, and 57.9% had a nocturnal waking duration < 1 hr. Based on normative data (Paavonen et al., 2020), Sadeh's (2004) criteria apply to children across the 0–5-year-old age range used in this study. In line with these cut-off criteria (Sadeh, 2004), 66.0% of children in this study, regardless of age, had a sleep problem (minor = 31.2%; moderate = 24.1%; major = 10.7%).
4.3 Correlation analysis of study variables
Pearson's correlations tested predictions of positive associations between child sleep problems and maternal depression, and identified confounds (Table 1). Analyses revealed a statistically significant, small positive correlation between child sleep problem severity and maternal depression (r = 0.14, p = 0.002, 95% CI [0.05, 0.22]). However, child age showed no association with EPDS scores (r = −0.01, 95% CI [−0.09, 0.09]), supporting our decision to examine maternal depression beyond the typical postpartum period. Child age showed statistically significant correlations with other key study variables and was therefore controlled for as a potential confound.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. PA | ||||||||||
| 2. CA | 0.23*** | |||||||||
| 3. FC | −0.15*** | −0.03 | ||||||||
| 4. PM | 0.13** | 0.05 | 0.08 | |||||||
| 5. SP | 0.17*** | 0.12** | 0.07 | 0.16*** | ||||||
| 6. ES | 0.14** | 0.42*** | −0.07 | 0.00 | −0.01 | |||||
| 7. PR | 0.03 | −0.10* | 0.04 | −0.01 | 0.08 | −0.07 | ||||
| 8. SD | −0.06 | 0.26*** | 0.16*** | −0.05 | 0.02 | 0.16*** | −0.19*** | |||
| 9. PSE | −0.07 | 0.06 | −0.09 | −0.10* | −0.00 | 0.07 | 0.01 | 0.26** | ||
| 10. MD | 0.06 | −0.01 | −0.01 | 0.10* | 0.04 | 0.05 | −0.02 | −0.20*** | −0.47*** | |
| 11. CSP | −0.06 | −0.32*** | −0.10* | −0.01 | 0.01 | −0.23*** | 0.14** | −0.52*** | −0.24*** | 0.14** |
- Abbreviations: CA, child age; CSP, child sleep problem; ES, employment status; FC, first child; MD, maternal depression; PA, parental age; PM, premature; PR, parental responsibility; PSE, parental self-efficacy; SD, parents' sleep duration; SP, sole parent.
- * p < 0.05.
- ** p < 0.01.
- *** p < 0.001, two-tailed.
4.4 Mediation model predicting maternal depressive symptoms
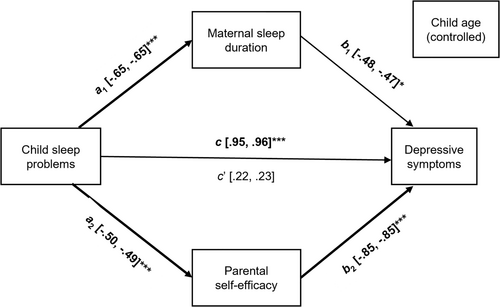
Mediation modeling was conducted after satisfying test assumptions (Hayes, 2017). Controlling for child age, we conducted a robust bootstrapped parallel mediation to test the hypothesized model, that maternal sleep and self-efficacy would mediate child sleep problems as a predictor of maternal depression. Both indirect pathways were supported, from child sleep problems to maternal sleep duration and to parental self-efficacy, to depressive symptoms. However, level of statistical significance varied. For the maternal sleep-depression pathway, p = 0.017, for parental self-efficacy-depression, p < 0.001. We found the total effect of child sleep problems on maternal depression was statistically significant, but the direct effect of child sleep problems on maternal depression was not. In other words, after partialling out the effects of other variables, child sleep problems no longer predicted maternal depression. These results support the hypothesis that both maternal sleep and maternal self-efficacy mediate the relationships between child sleep problems and maternal depression. Figure 1 presents the details of the parallel mediation model.
We next calculated AICc values (corrected Akaike information criterion) to test whether the data support a specific model. The lowest AICc value indicates the best fit. The full model AICc was 2.43 lower than the next best, the self-efficacy model. The AICc weights tell us the full model has about a 77% chance of being the best model, and the self-efficacy model about 23%. Table 2 also shows the maternal sleep model has much less support but does contribute beyond the child sleep problem model.
| Regression comparisons | AICc comparisons | |||||
|---|---|---|---|---|---|---|
| Model | RSE | Adj. R2 | p | K | ΔAICc | AICc wt |
| Full | 4.28 | 0.20 | < 0.001 | 6 | 0.00 | 0.77 |
| Efficacy | 4.30 | 0.19 | < 0.001 | 5 | 2.43 | 0.23 |
| Sleep | 4.69 | 0.04 | < 0.001 | 5 | 87.34 | 0.00 |
| CSP | 4.74 | 0.02 | 0.008 | 4 | 97.00 | 0.00 |
- Abbreviations: AICc, corrected Akaike information criterion; RSE, residual standard error; Full, child sleep problems, child age, maternal sleep, self-efficacy; Efficacy does not include maternal sleep; Sleep does not include self-efficacy; CSP only includes child sleep problems and child age; wt, weight.
5 DISCUSSION
The objective of this study was to contribute to our understanding of the relationship between child sleep problems and depression in early motherhood by examining the possible mediating effects of maternal sleep duration and parental self-efficacy. We also addressed the child age gap in the literature by including children aged 3 months to 5 years, as most previous study was limited to children up to 12 months old. We tested a unidirectional infant-driven model predicting the relationship between child sleep problems and maternal depression would be mediated by both maternal sleep duration and parental self-efficacy. Robust bootstrapped results supported that model. Maternal sleep duration and self-efficacy accounted for most of the variance between child sleep problems and maternal depression. Self-efficacy, in particular, showed evidence as a strong mediating factor.
The literature on maternal depression is dominated by studies of mothers during the first 12 months postpartum. Here, we included mothers of children aged up to 5 years old. When we examined maternal depression by age of child, we saw a correlation of approximately zero (95% CIs = −0.10, 0.09), and a plot of the data revealed a nearly straight line. That is, there were no differences in maternal depression by age of child. This finding indicates that studies on maternal depression may be expanded to examine more variables, such as self-efficacy, but also longer periods of motherhood. However, we also note that child age did show associations with other variables and was statistically controlled for to provide more generalizable results.
The parallel mediation model showed total effect of child sleep problems on maternal depression was statistically significant; however, the direct effect was not. This indicates that the relationship between child sleep problems and maternal depression is complex, involving mediating phenomena. Previous literature has identified maternal sleep as a mediator between child sleep and maternal depression (Hairston et al., 2016; Meltzer & Mindell, 2007). The current study adds to the understanding of the relationship between child sleep problems and maternal depression by including self-efficacy in the model and controlling for child age as a potential confound. An additional bivariate finding showed that more severe child sleep problems predicted lower maternal sleep duration, consistent with Kalmbach et al. (2021). The current study also found that higher parental self-efficacy negatively predicted maternal depression, which is consistent with previous research (Giallo et al., 2013; Werner et al., 2022).
Our findings showed that having a child with a sleep problem alone does not predict depression, but the effects of a child's sleep problem on maternal sleep duration and self-efficacy indirectly predict depression. Maternal sleep duration and self-efficacy are modifiable risk factors of maternal depression. These findings have clinical implications for early intervention and routine screening for sleep disturbances in mothers and their children as risk factors for maternal depression. Interventions should focus on building self-efficacy in parents of children with sleep problems especially when maternal sleep duration is also low. Evidenced-based practices like cognitive behavioural therapy (CBT) for maternal depression (Huang et al., 2018) and CBT for insomnia (Çıvgın & Dirik, 2020) may be revised to incorporate the unique challenges of early motherhood and a focus on parental self-efficacy through cognitive restructuring.
5.1 Strengths and limitations
The current study recruited parents of infants and children who they believed experienced sleep difficulties. As such, it is difficult to compare with other samples as 34% of this sample had no sleep problem, based on Sadeh's (2004) criteria. These results suggest that a discrepancy exists between mother's perception of problematic sleep and quantified sleep problems using Sadeh's criteria, which should be investigated in future research. In the current sample, over half of mothers had inadequate sleep duration (< 7 hr; Hirshkowitz et al., 2015), which is lower than Yang et al.'s (2020) estimation of two-thirds of postpartum women experiencing sleep problems. This discrepancy may be attributable to the current child's age inclusion criteria beyond the postpartum period. Price et al.'s (2012) Australian study found that 40% of mothers of children with a sleep problem during the first year of life reported depressive symptoms, which is comparable to the current study's prevalence of 38% from 3 months to 5 years postpartum. However, Levis et al. (2020) suggest using a more conservative cut-off score of ≥ 13 to avoid false negatives. The current study found that 17.6% of mothers had clinical levels of depression (EPDS ≥ 13).
These results should be considered in light of limitations. We used robust bootstrapped parallel mediations to test expanding existing theory and evidence. However, this cross-sectional study does not provide evidence on causation. The methods used here are compatible, however, with continuing longitudinal assessment of mother and child factors, which would provide more definitive evidence of development and buffering of sleep and depressive factors. Mothers with low education, sole parents and those residing outside of New South Wales were underrepresented. Variable availability is an inherent disadvantage of secondary analyses. The current study did not include detailed health or household information, measures of sleep quality, anxiety, mental health history, depression onset or duration, which may impair generalizability. Single item self-reported variables, such as mother's sleep duration and child developmental milestones, limited the accuracy and objectivity of information. Imminent research should consider additional variables, diagnostic approaches, longitudinal research, and the development of standardized norms and measurements for child sleep behaviours. Maternal-driven and bidirectional models should be considered with additional variables and age ranges. Future research on the continuity of sleep problems in children and mothers is necessary to further delineate the effects of sleep on child development and maternal wellbeing.
Our findings demonstrate that a simple approach to understanding the relationship between child sleep problems and maternal mental health could lead to inaccurate conclusions. A more complex model, including maternal sleep and self-efficacy, provided an improved understanding of this important human dilemma – caring for children with sleep problems without imperilling one's own mental health. Another notable finding was that there was no relationship between the child's age and maternal depression. This may help open the door to more studies with broader ages of children to better understand relationships between sleep and depression in early motherhood.
AUTHOR CONTRIBUTIONS
Alyssa J. Carroll: Conceptualization; data curation; formal analysis; methodology; project administration; validation; visualization; writing – original draft; writing – review and editing. Jessica Appleton: Conceptualization; data curation; investigation; methodology; project administration; resources; supervision; writing – review and editing. Keith M. Harris: Formal analysis; methodology; project administration; software; supervision; validation; writing – review and editing.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENT
The original research and data this analysis is based on were developed by a research team from the University of Technology Sydney, Tresillian, and Sleepfit. The original research was funded by a grant to Sleepfit and Tresillian from private health insurer HCF (Hospitals Combined Fund) for a partnership to develop and validate a digital parenting program. Open access publishing facilitated by Charles Sturt University, as part of the Wiley - Charles Sturt University agreement via the Council of Australian University Librarians.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from Tresillian, email [email protected]. The data are not publicly available due to privacy or ethical restrictions.




