System level interventions to reduce utilization of general anesthesia to treat dental caries: a practice brief
Abstract
Dental caries are the most common chronic disease of childhood. Untreated caries can result in severe pain and infection; and in some cases, difficulties in eating, speech, and education. Hospitalization and general anesthesia are often necessary for treating extensive disease in young children, which adds significant risk and expense. Interventions, such as community-based preventative care, utilization of pre-authorizations for treatment, and at-risk contracts, have been deployed as innovative strategies to reduce the incidence of caries and the cost of treatment. Value-based payment structures give payors flexibility to design a multipronged system to impact the health of consumers. This practice brief will identify interventions at a systems level that reduced the utilization of general anesthesia treating dental caries in children under the age of six. Dental claims data from the period of Q1 2011 to Q2 2020 were utilized to analyze the trends in utilization of the operating room (OR) to treat dental conditions among children under 6 years. Fixed effects analysis was utilized to identify key over time changes in the reduction of children's OR utilization. A reduction in utilization of general anesthesia and hospitalization for treating dental caries in young children was seen. The expansion of the community care team, metrics to reinforce the systems of provider education and training, and the use of incentive payments were all associated with reductions in the rate of OR utilization. Between 2012 and 2017, multiple initiatives were implemented without a systematic approach to quality improvement to evaluate.
Program
Advantage Dental from DentaQuest is a Dental Service Organization based in Oregon. Advantage Dental was founded in 1994 by a group of dentists wanting to address the dental needs of rural Oregonians. The design of Advantage Dental's care delivery model evolved over several years, with a commitment to develop a system where no one had to suffer the ravages of tooth decay.1 The organization is a vertically integrated dental accountable care organization where providers are responsible for an assigned population of patients. The care delivery system includes a mix of contracted network providers, staff model practices, and community care hygienists with a shared focus to control costs and improve outcomes. This risk-based model encourages innovative strategies and incentives to develop and meet quality metrics, where quality is defined as the “degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”2
During 2012–2017, changes occurred at a state level to promote integration across physical, oral, and behavioral health. The aim of these changes was to move payment models from output to outcomes. Riley et al. explain in their framework for value-based care “When the focus turns to results rather than services (value rather than volume), the oral health care delivery model can change to proactively preventing oral disease rather than one primarily designed around the restorative measures needed to treat disease.”3 Advantage Dental was compelled to look at initiatives that would result in better health outcomes for the membership at a reduced cost, such as ongoing provider trainings around disease prevention and management, expanding disease management services to community care sites, and providing encounter credit for use of caries risk codes. Use of hospital facilities and general anesthesia to provide dental care for young children is widely recognized as an expensive4 and risky5-8 alternative to manage a preventable disease.
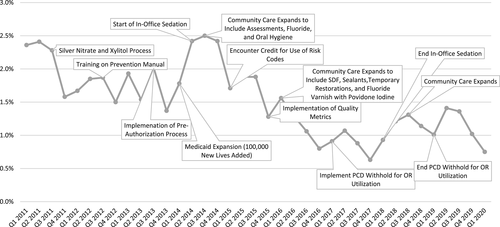
The caries process has been defined as a preventable bacterial infection passed from primary caregiver to child in the first year of life9, 10 that is costly to the overall system. With this in mind, various strategies were implemented to influence early disease intervention and discourage hospital referral for caries management in children under 6 years. A retrospective review of system changes employed during this time period determined those that had the greatest impact on cost and general anesthesia utilization for children under 6 years were: community-based care, preauthorization for general anesthesia/hospital referral, and utilization and quality metrics (Figure 1).
Implementation of a detailed preauthorization system occurred in third quarter of 2013 to review non-emergent hospital and general anesthesia referrals. The intent of preauthorizing was to encourage non-invasive caries management interventions when medically appropriate and to ensure a comprehensive risk-based preventive treatment plan was in place. Advantage Dental endorsed use of any recognized forms of caries risk assessment. Development of a caries risk assessment that considered the International Caries Detection and Assessment System, Association of State and Territorial Dental Directors Basic Screening Survey, and the American Dental Association's Caries Risk Assessment occurred over time. These assessments were adapted to work in the unique care delivery model deployed by Advantage Dental. Calibration of contracted providers would have been ideal, though given the number of providers was not feasible. The primary use of a risk assessment was to increase awareness of a members risk and to increase follow through for patients at risk of disease. An evaluation of internal claims data prior to implementation of the caries risk assessment tool identified an increase of repeat general anesthesia GA cases and lack of disease management by providers.
Approval of hospital facility and general anesthesia referrals occurred when medically necessary, due to multiple existing infected teeth and when other appropriate treatment options had been attempted as well as taking into account age, behavior, and ASA physical classification status. The preauthorization system also allowed better visibility and quality of care monitoring for repeat hospital referrals of individual members for follow-up to engage case management services or follow-up with primary care dentist (PCD) offices on caries disease management protocols.
Community-based dental services, beyond screening and fluoride varnish, were implemented in third quarter of 2014 to address inequities in utilization of care through disease management and prevention by Expanded Practice Dental Hygienists. The goal of community care was to increase utilization and bridge the gaps between members and dental care by taking expanded practice permit dental hygienists into community-based settings. Dental services utilized expanded from assessments and fluoride varnish to a broader menu of services like fluoride varnish in conjunction with povidone iodine, silver diamine fluoride, sealants, and temporary restoration without excavation. Another unique piece as expansion occurred was the electronic connectivity between PCD and the community care team. This allowed the opportunity to work in collaboration to support the patient in their care to reduce disease.
Advantage Dental had always had some level of utilization management and review and employed a variety of quality incentive metrics to influence best practices. Examples of quality incentive metrics used at various times by Advantage have included value-based payment for meeting performance goals for caries risk assessment, utilization by pregnant members and young children, emergency department utilization, and patient satisfaction. Additional targeted quality measures were developed and implemented in fourth quarter of 2015, which took into consideration medically appropriate in-office sedation and minimally invasive caries management techniques to include services, such as fluoride therapies and glass ionomers and later, silver diamine fluoride. By training providers on evidence-based options to reduce the risk and expense associated with oral or intra-venous sedation hospitalization and general anesthesia and tying quality incentive funds to this, it helped with acceptance from providers across the network.
Objective/goal
Identify interventions at a systems level that reduced the utilization of general anesthesia and hospitalization for treating dental caries in children under the age of 6.
Methodology
Dental claims data from the period of Q1 2011 to Q2 2020 were utilized to analyze the trends in utilization of the operating room (OR) to treat dental conditions among children between the ages of 1 and 6. OR utilization was identified in the claims data using the CDT code D9420, a billing code for referral to a hospital or ambulatory surgical center. The proportion of total patients seen by Advantage Dental providers who were treated in the OR is the outcome of interest. A timeline of key events in community-based care, preauthorization for general anesthesia/hospital referral, and utilization and quality metrics is mapped against trends in this proportion to understand drivers of general anesthesia/hospital referrals.
In addition, fixed effects analysis was utilized to identify key over time changes in the reduction of children's OR utilization for dental conditions (Table 1). Fixed effects models control for time-invariant unobserved characteristics that may influence whether children are referred to the OR. Therefore, the results presented here are not biased by the specific characteristics of the children that make up the population at each time period and, thus, focuses on the systems-level changes. However, caution should be taken when interpreting these results, as they may still be biased by the presence of over time changes of children in the population. Moreover, as processes were constantly being improved during this period, it is difficult to separate the effects of individual initiatives definitively.
| 95% CI | |||
|---|---|---|---|
| Intervention or period | Coefficent | Lower Limit | Upper Limit |
| Medicaid expansion | 0.49* | 0.03 | 0.27 |
| Pre-authorization | −0.21 | −0.68 | 0.27 |
| Community care expansion | −0.65* | −0.88 | −0.38 |
| Utilization and quality metrics | −0.68* | −1.36 | −0.01 |
| Incentive payments and PCD withholds | −0.71* | −1.49 | −0.07 |
| Intercept | 1.90* | 1.71 | 2.09 |
| Number of time periods | 37 | ||
| Number of patients | 105,409 | ||
- * Indicates P < 0.05.
- CI, confidence interval; PCD, primary care dentist.
Outcomes
The referral of children during the period fell from 2.4% of in Q1 of 2011 to 0.8% in Q1 of 2020, with the period from the first quarter of 2015 onward having consistent declines (Figure 1). The pre-authorization system and provider education appeared to reduce the referral of children to the OR, but that decline was interrupted by Medicaid expansion, which added 100,000 new covered lives to Advantage Dental. The regular expansion of community care team, in both size and practice scope, along with the implementation of encounter credits and withholds for PCDs were associated with a declining proportion of children being referred to the OR. The cumulative effect of these processes appears to make the reduction relatively “sticky,” that patterns are relatively robust to the ending of initiatives that influence behavior, such as in-office sedation and the withhold payments.
The fixed effects regression bears out the descriptive findings. Controlling for time-invariant unobserved factors, we see that Medicaid expansion increased the proportion of children referred to the OR by approximately 0.5% points On the other hand, the expansion of the community care team, the addition of utilization and quality metrics to reinforce the systems of provider education and training, and the use of incentive payments and PCD withholds to incentivize provider behavior were associated with reductions in the rate of referral to OR by 0.65 percent, 0.68 percent, and 0.71 percent, respectively. These results also demonstrate that cumulative effect of each of these interventions in facilitating reductions.
Lessons learned
- During the time period of 2012–2017, multiple initiatives were implemented without a systematic approach to quality improvement. This made it challenging to determine the effectiveness of particular interventions.
- The preauthorization system provided data to identify knowledge gaps among the providers. Training to increase alternative approaches to care for minimally invasive procedures were provided.
- External policy changes through dental licensure regarding anesthesia and FDA guidance around use of general anesthesia supported organizational initiatives in regard to treating caries under general anesthesia.
- Providing community-based dental services increased utilization of preventive services reducing the gap in care.
- Development and implementation of metrics coupled with incentive payments was marginally effective in influencing provider behavior to reduce hospital referrals. The reason being that one provider could have a larger pool of children who did need to go to the OR and they would be negatively impacted due to the random assignment of members.
- Education and training on evidence-based alternative interventions are helpful to support behavior change.
Strategies for implementation
- Ensuring that there is an equal distribution of members to all providers to improve equal provider impact could improve overall buy-in to the metric.
- A traditional structured quality improvement project approach is recommended when possible to accurately measure and evaluate the effectiveness of interventions to influence provider behavior and achieve desired clinical outcomes.
- Multiple overlapping interventions may occasionally be necessary in a provider group due to external and internal pressures to reduce costs and improve clinical outcomes on an accelerated schedule. A rapid cycle improvement process can be a useful and necessary approach but may limit accurate measurement of the effectiveness of different strategies. Identification of rapid cycle performance improvement as the primary objective is important to allow a systematic approach to planning, implementing, and measuring the effectiveness of multiple overlapping strategies.
Acknowledgment
The authors would like to thank Yara Halasa-Rappel for her analytical support on this manuscript.