A systematic review and meta-analysis of serum lipid concentrations in people with Down syndrome
Abstract
Background
Down syndrome (DS) is the most prevalent chromosomal disorder, being the leading cause of intellectual disability. The increased life expectancy of individuals with DS has led to a shift in the incidence of non-communicable chronic diseases, resulting in new concerns, particularly cardiovascular disease (CVD) and Alzheimer's disease. This study aimed to analyse the blood lipid profile of a large DS cohort to establish a baseline for evaluating health risk parameters.
Methods
A comprehensive literature search was conducted on PubMed and Virtual Health Library databases to identify original articles published before July 2022. Selected studies were included in the meta-analysis.
Results
Fifteen studies reporting serum lipid levels in individuals with DS were incorporated into the analysis. The meta-analysis used the means and standard deviations extracted from the selected studies. The analysis encompassed 671 participants in the DS group and 898 euploid controls. The results indicated significant differences in total cholesterol [C] (mean difference [MD]: −3.34; CI: 95%: −4.94 to −1.73; P < 0.0001), HDL-C (MD: −3.39; CI: 95%: −6.72 to −0.06; P = 0.05) and triglycerides (MD: 21.48; CI: 95%: 9.32 to 33.65; P = 0.0005) levels between individuals with DS and their control counterparts.
Conclusions
Individuals with DS have less favourable blood lipid concentrations than their controls, particularly HDL-C, triglycerides, and total-C, even when grouped by age. These findings underscore the importance of closer monitoring of lipid profiles in people with DS and the necessity for specific cut-offs for this population, considering the risk for ischemic heart and Alzheimer's diseases.
Introduction
Down syndrome (DS), also referred to as trisomy 21, stands as the most prevalent genetic disorder associated with intellectual disability. Recent data estimates its global prevalence at just over 1 800 000 cases, with an annual incidence of 80 000 cases in 2019, which has displayed relative stability throughout the past decade (Chen et al. 2022). Advancements in medical healthcare over recent decades have notably contributed to an extended life expectancy for individuals with DS. Different studies estimate that the average life expectancy for individuals with DS is 28 years lower than the general population (O'Leary et al. 2018). Nonetheless, the ageing process in individuals with DS has been characterised as premature compared to their euploid counterparts, rendering DS a significant risk factor for developing conditions typically associated with the elderly population, such as Alzheimer's disease, osteoarthritis, and hearing loss (Cilhoroz et al. 2022).
DS encompasses a range of conditions affecting various body systems. While there exists considerable variability in clinical manifestations among individuals with DS, specific health issues, including congenital heart disease, obstructive sleep apnoea, thyroid dysfunction, and immunological anomalies, exhibit higher prevalence in this population than in the general populace (Antonarakis et al. 2020). Moreover, the incidence of non-communicable chronic diseases, such as obesity, diabetes, and dyslipidaemias, has risen alongside increased life expectancy among individuals with DS, necessitating a closer examination of cardiovascular disease (CVD) risk factors (Adelekan et al. 2012; Buonuomo et al. 2016; Cilhoroz et al. 2022).
Many decades ago, DS was considered a model of atherosclerosis-free condition (Murdoch et al. 1977). However, the results of epidemiological studies in the early 21st century did not support this theory, as they found an increased risk of mortality from ischemic heart disease and cerebrovascular diseases (Hill et al. 2003; Day et al. 2005). These findings reinforced previous discoveries of atherosclerotic lesions in coronary arteries obtained from autopsies of young individuals with DS (Moss & Austin 1980). Nevertheless, this topic remains inconclusive, as a recent systematic review identified ischemic heart diseases and cancer as uncommon causes of mortality in people with DS, with congenital heart anomalies, respiratory diseases, leukaemia, dementia, and Alzheimer's disease being the primary causes of mortality (O'Leary et al. 2018). Although the authors acknowledge the need for adjustments for ethnicity, socioeconomic status, and the lack of data in death registries, it is noteworthy that altered lipid profiles appear to be associated with a higher risk of dementia, whether due to comorbidities such as obesity and diabetes or Alzheimer's disease as a cause of death (Zaciragic et al. 2022; Hassen et al. 2023).
Recognising the significance of comprehending the blood lipid profile in individuals with DS is pivotal, given the genetic underpinnings of the condition and its potential ramifications for various aspects of health, particularly cardiovascular health. The blood lipid profile, encompassing measurements of cholesterol and other lipids in the bloodstream, is crucial in assessing and managing the health of individuals with DS. While several studies have investigated serum lipid profiles in people with DS (Zamorano et al. 1991; Pueschel et al. 1992; Adelekan et al. 2012; Real de Asua et al. 2014; Buonuomo et al. 2016; Parra et al. 2017; Garcia-de la Puente et al. 2021), the individual results have yielded mainly inconclusive findings. Considering the ongoing controversy regarding the risk of cardiovascular diseases and the increased risk of Alzheimer's observed in individuals with DS, further research is required to elucidate the standard for lipid parameters in assessing individuals with DS. Therefore, the present study aims to clarify and synthesise the prior 30 years of research by conducting a systematic review and meta-analysis of serum lipid levels in individuals with DS.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al. 2021) and was previously registered on PROSPERO (registration number: CRD42022346666).
Literature search strategy
A literature search was performed in the Medical Literature Analysis and Retrieval System Online (MEDLINE) via PubMed and Virtual Health Library (VHL) databases to identify eligible studies. Observational studies published in English or Spanish that analysed serum lipid levels in individuals with DS, with ages older than 1 year, and a control group comparison were included in the study. The search identified reports published up to the year 2022 using the following strategies: (“Down Syndrome” [Mesh] OR “Trisomy 21*” OR “Syndrome, Down*” OR “Down* Syndrome*” OR Mongolism OR “Trisomy G") AND (“Lipids/blood” [Mesh] OR “Lipids/metabolism” [Mesh] OR Triglyceride* OR “Blood triglyceride*” OR Cholesterol OR “Blood cholesterol” OR Lipoprotein* OR “Total cholesterol” OR “Total blood cholesterol” OR “Serum cholesterol” OR “Serum lipids” OR “Serum lipid profile*” OR “Lipid profile*” OR “Dyslipidemias” [Mesh] OR Dyslipidaemia* OR Hyperlipaemia OR Hyperlipidaemia OR Hyperlipemia OR “High blood cholesterol” OR “High blood triglyceride*” OR “Triglycerides” [Mesh] OR “Lipoproteins” [Mesh] OR “Cholesterol” [Mesh]) for PubMed, an adaptation in Spanish of the same key terms was used for Virtual Health Library. Two authors separately conducted the search. All retrieved articles were compared, and any potential conflicts were discussed and settled by consensus.
Study selection and data extraction
The following criteria were applied to discern among the identified studies: To be included, the study must exhibit an observational design, employ English or Spanish as the publication language, report concentrations of serum lipid fractions in individuals with a verified diagnosis of DS, involve a population aged 1 year or older, and include a control group for result comparison. Studies failing to meet the inclusion criteria, along with those that did not distinguish the presence of comorbidities (e.g. hypothyroidism, diabetes mellitus and congenital heart disease) within their populations, were excluded. Two researchers using Rayyan software independently performed the literature screening and data extraction process (Ouzzani et al. 2016). Citations were imported into the software, and duplicates were systematically identified and eliminated. In the initial screening phase, assessments were based on the titles and abstracts of the studies, with exclusion applied to those that did not align with the predefined inclusion criteria. Any selection disparities between the two reviewers were addressed through discussion and consensus. Following this initial screening, a second screening ensued, during which the full text of the identified references was evaluated. Likewise, studies failing to meet the inclusion criteria or missed data for extraction were excluded from the study. The data extracted from the retained studies included the first author's name, publication year, groups, number of participants, age, sex distribution, and serum levels of total-C, HDL-C, LDL-C and TG (presented as mean ± standard deviation).
Statistical analysis
The mean values and their respective standard deviations of serum lipid levels were analysed with a meta-analysis for each lipid fraction of interest. Studies that reported more than one mean value per lipid fraction were given separate entries for each value reported for their inclusion in the analyses. The meta-analyses were performed using Review Manager version 5.4 software. Heterogeneity was tested using Cochran's Q-statistics and I-statistics, utilising a random-effects model. Mean difference (MD) was used to measure the effect size, and a P value of less than 0.05 was considered statistically significant.
Results
Literature search
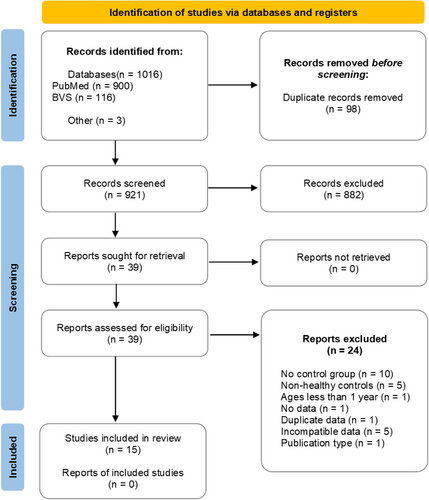
Figure 1 shows the PRISMA 2020 flow diagram depicting the study selection process. Initially, 921 articles were identified, with duplicates removed, resulting in 882 exclusions during the first screening due to non-compliance with inclusion criteria. Subsequently, 39 articles underwent full-text screening, of which 24 reports were excluded. These exclusions comprised 10 studies lacking a control group, five studies devoid of healthy controls, one study included subjects below 1 year of age, one study containing unextractable data, one study featuring duplicate data from the same author, five studies with incompatible data, and one study with an unsought publication type. Ultimately, 15 studies were included in the final review, summarising their respective characteristics in Table 1.
| First author (year) | DS participants (n) | Control participants (n) | Age (years ± SD) | Lipid profile | |||
|---|---|---|---|---|---|---|---|
| Total-C | LDL-C | HDL-C | TG | ||||
| Adelekan et al. (2012) | 27 | 31 | 6.6 ± 2.1 | ● | ● | ● | ● |
| Corsi et al. (2005) | 19 | 23 | 55 | ● | ● | ● | ● |
| Draheim et al. (2010) | 52 | 52 | 35–60 | ● | ● | ● | ● |
| Lacko et al. (1983) | 21 | 9 | 16–46 | ● | ● | ● | ● |
| Nagyová et al. (2000) | 25 | 25 | 18 ± 5, 17 ± 7 | ● | ● | ● | ● |
| Nishida et al. (1977) | 20 | 16 | 23.1 ± 9.2 | ● | ● | ||
| Parra et al. (2017) | 51 | 51 | 35.8 ± 10.6 | ● | ● | ● | ● |
| Pueschel et al. (1992) | 27 | 23 | 8–32 | ● | ● | ● | ● |
| Real de Asua et al. (2014) | 48 | 33 | 36 ± 11 | ● | ● | ● | ● |
| Rubello et al. (1995) | 227 | 257 | 1–53 | ● | ● | ● | |
| Sánches et al. (1986) M | 15 | 67 | 9–13 | ● | ● | ● | |
| Sánches et al. (1986) F | 21 | 88 | 9–13 | ● | ● | ● | |
| Sánchez-Lamar et al. (1985) | 38 | 141 | 9–13 | ● | |||
| Tansley et al. (2012) | 20 | 22 | 29–61 | ● | ● | ||
| Taşdemir et al. (2004) | 21 | 22 | 5.52 ± 2.26 | ● | ● | ||
| Tenneti et al. (2017) | 39 | 38 | 2–12 | ● | ● | ● | ● |
| TOTAL | 671 | 898 | |||||
- ●, data available for analysis; DS, Down syndrome; F, female; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; M, male; SD, standard deviation; TG, triglyceride; total-C, total cholesterol.
Meta-analysis findings
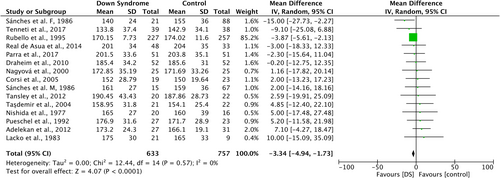
Fourteen studies compared serum total-C levels between individuals with DS (n = 633) and euploid controls (n = 757) (Figure 2). The studies exhibited low heterogeneity (I2 = 0%; P = 0.57). The results highlighted statistically significant differences between the groups, revealing lower serum total-C levels within the DS group (Mean difference (MD): −3.34; 95% CI: −4.94 to −1.73; P < 0.0001).
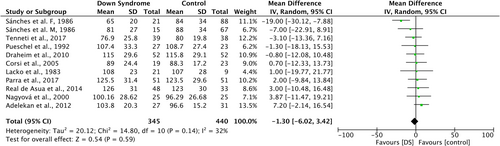
Ten studies compared serum LDL-C concentrations between the DS cohort (n = 345) and euploid controls (n = 440) (Figure 3). Heterogeneity among the studies was low (I2 = 32%; P = 0.14). However, no statistically significant differences were found between the groups (MD: −1.30; 95% CI: −6.02 to 3.42; P = 0.59).
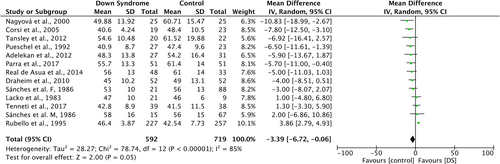
Twelve studies compared serum or plasma HDL-C concentrations between the DS group (n = 592) and euploid controls (n = 719) (Figure 4). These studies displayed significant heterogeneity (I2 = 85%; P < 0.00001). Moreover, statistically significant differences between the groups were obtained, with lower serum HDL-C concentrations in the DS group (MD: −3.39; 95% CI: −6.72 to −0.06; P = 0.05).
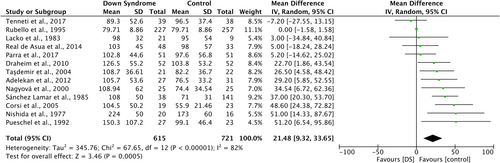
Finally, a comparison of serum or plasma TG concentrations was executed across 13 studies involving individuals with DS (n = 615) and euploid controls (n = 721) (Figure 5). Heterogeneity among the studies was significant (I2 = 82%; P < 0.00001). The analysis demonstrated statistically significant differences between the groups, indicating higher serum TG levels within the DS group (MD: 21.48; 95% CI: 9.32 to 33.65; P = 0.0005).
Subgroup analysis findings
Considering the presence and variability of heterogeneity observed during the analysis of the included studies, an additional subgroup analysis was conducted based on participants' age, categorised into groups aged below 21 and those aged 21 or older.
The outcomes resulting from the implementation of the subgroup analysis are summarised in Table 2. In the cases of total-C (I2 = 50% for <21 subgroup; I2 = 0% for >21 subgroup) and LDL-C (I2 = 76% for <21 subgroup; I2 = 0% for >21 subgroup), participants aged below 21 exhibited higher levels of heterogeneity. This diverges from the heterogeneity obtained in the previously presented meta-analysis with all ages included (I2 = 32% for total-C; I2 = 0% for LDL-C). Conversely, regarding HDL-C (I2 = 0% for <21 subgroup; I2 = 23% for >21 subgroup) and TG (I2 = 74% for <21 subgroup; I2 = 58.8% for >21 subgroup), heterogeneity was lower in comparison to the previous results (I2 = 85% for HDL; I2 = 82% for TG). However, it is important to note that the observed statistical significance in heterogeneity between subgroups only applied to the HDL-C parameter (P = 0.02). Despite the variations obtained in the subgroup analysis, the tendency of effect sizes observed in the original meta-analysis remained consistent.
| Lipid parameters | Subgroup by age (years) | No. of studies included | Mean difference (95% CI) | Heterogeneity within subgroup (I2) | Heterogeneity between subgroups (P) |
|---|---|---|---|---|---|
| Total-C | <21 | 4 | −2.12 (−11.28, 7.05) | 50% | 0.63 |
| >21 | 8 | 0.55 (−5.34, 6.43) | 0% | ||
| LDL-C | <21 | 3 | −3.89 (−9.39, 1.62) | 76% | 0.18 |
| >21 | 6 | 1.44 (−4.07, 6.95) | 0% | ||
| HDL-C | <21 | 3 | −0.3 (−3.48, 2.88) | 0% | 0.02 |
| >21 | 7 | −5.2 (−7.72, −2.67) | 23% | ||
| TG | <21 | 4 | 21.54 (1.55, 41.53) | 74% | 0.89 |
| >21 | 7 | 23.29 (8.55, 38.04) | 58.8% |
- Random effects model was used.
- CI, confidence interval; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TG, triglyceride; total-C, total cholesterol.
Sensitivity analysis
Two types of sensitivity analyses were performed. First, each study included in the meta-analysis was individually removed to assess its impact. Additionally, the Newcastle-Ottawa scale was used to evaluate the methodological quality of the studies; those with the lowest scores were removed from the analysis to verify the consistency of the previously obtained results. Following the removal of studies in the meta-analysis for all the examined lipid parameters, no qualitative alterations were observed in the overall effect sizes. This suggests a robust and reliable nature of the outcomes derived from this meta-analysis.
Publication bias
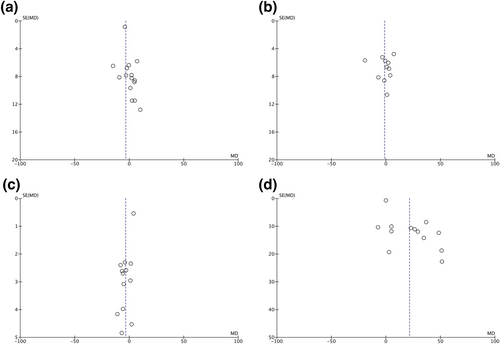
Funnel plots were used to assess potential publication bias across each lipid parameter examined within the study. In all cases, no noticeable asymmetry was observed in the plots, indicating the absence of significant evidence supporting publication bias in the meta-analysis (Figure 6).
Discussion
This meta-analysis examined the association between serum lipid levels and the presence of DS. A total of 671 participants with a confirmed DS diagnosis, as well as 898 euploid controls, were included in the study. The findings revealed distinct alterations in the lipid profile of DS individuals, with significant differences observed in total-C, HDL-C, and TG levels. Notably, the DS group exhibited less favourable lipid profiles compared to those of the control group, except for total-C levels, which, although lower and seemingly favourable in the DS group, did not cross the 200 mg/dL threshold (NCEP & ATP 2002) in either group, yielding similar interpretations regarding both groups' outcomes.
The underlying mechanisms driving the propensity of DS individuals towards unfavourable lipid profiles remain unclear. Possible explanations for this outcome may include a higher prevalence of overweight and obesity, diabetes mellitus, interaction with other health condition, and dietary and lifestyle habits. Nevertheless, some controversy remains regarding the association of higher body mass index (BMI) as well as nutritional status as risk factors for dyslipidaemia in DS. Some studies find an association between excess body weight and an affected lipid profile (Valentini et al. 2017; Garcia-de la Puente et al. 2021; Oreskovic et al. 2023), while others do not (Real de Asua et al. 2014; Bertapelli et al. 2016; de la Piedra et al. 2017; Magge et al. 2019). Contributing to resolving this knowledge gap is part of the objective of the present meta-analysis. Furthermore, within the studies included in the present meta-analysis, segregating participants by BMI or evaluating their dietary and lifestyle habits was uncommon.
In the case of hyperglycaemia and insulin resistance, which can induce oxidative stress, glycation of lipoproteins such as LDL-C and higher levels of coagulation leading to endothelial damage and increased atherogenesis (Aronson & Rayfield 2002; Adelekan et al. 2012), only two of the included studies reported glucose levels, and no significant variance was found between the study groups.
Given that the DS phenotype is linked to dosage imbalances of genes on chromosome 21 and subsequent overexpression of these genes (Asim et al. 2015; Perez-Villarreal et al. 2022), it is plausible that abnormal lipid profiles in DS individuals are influenced by genetic factors affecting lipid metabolism. Prior research identified a susceptibility locus on chromosome 21 associated with elevated Apo B levels, a primary constituent of very low-density lipoproteins (VLDL) and LDL (Pajukanta et al. 1999). More recently, it was found that chromosome 21, specifically in the 21q11 region, contains a gene locus responsible for encoding a VLDL receptor, likely playing a pivotal role in lipid metabolism regulation (de la Piedra et al. 2017; Garcia-de la Puente et al. 2021). Additionally, increased cholesterol levels have been observed in foetuses with trisomy 21 during intrauterine development, suggesting lipid metabolism abnormalities before other factors could influence lipid levels (Bocconi et al. 1997). While lifestyle habits may influence lipid profiles during later life stages, their role as an established causal factor in DS remains unverified, strengthening the hypothesis of an underlying genetic mechanism driving lipid profile alterations in DS individuals.
There is a lack of conclusive evidence regarding the influence of cardiovascular risk factors on the incidence of cardiovascular events in DS individuals. Current health guidelines for DS mainly emphasise BMI monitoring and obesity prevention through educational efforts; however, the recommendation for periodic monitoring of the lipid profile is not indicated (Lizama et al. 2013; Flores et al. 2021; Michael & Marder 2021; Bull et al. 2022; Dalrymple et al. 2022). Furthermore, despite the recently development of guidelines aimed to the adult DS population (Tsou et al., 2020), which had been previously focused to a greater extent on paediatric population, strong recommendations for the assessment and monitoring of serum lipid levels remain unclear given the scarcity of robust evidence needed to support them. Addressing this knowledge gap necessitates further research to inform the development of appropriate tools for lipid profile management.
Conclusions
Individuals with DS exhibit alterations in their lipid profiles, characterised by low levels of HDL-C and elevated TG concentrations. Routine monitoring of lipid profiles in this population is recommended, commencing from an early age. Long-term monitoring of serum lipid levels will be of great utility to determine if the differences between lipid profiles translate into heightened morbidity and mortality from cardiovascular and Alzheimer's diseases among individuals with DS. Further research is also encouraged beyond the limits of the DS population, diversifying through a wide scope of syndromes that could ultimately benefit from the advancements generated.
Limitations
This review has some limitations. First, there is heterogeneity between the studies included in the review. This includes differences regarding age groups; most authors provided mean values for this parameter, complicating classification for further subgroup analysis. Additionally, most studies did not provide separate mean values for different-sex participants, potentially impacting the interpretation of parameters with sex-specific references, such as HDL-C. We also consider that it is necessary to establish a control group comprising individuals with DS who fall within the normal weight range according to the growth charts specific to this population. This additional control group aims to mitigate potential confounding factors related to adipose tissue or metabolic anomalies that may impact the lipid profile. Lastly, there is no clarification of usage of lipid lowering medication within either group of participants of the studies included, a crucial element for the optimal analysis of the data presented.
Acknowledgements
We acknowledge the Programa de Fomento y Apoyo a Proyectos de Investigación (Profapi) from the Universidad Autónoma de Sinaloa, for the academic grant PRO_A3_020 provided.
Source of funding
This work was funded by Universidad Autónoma de Sinaloa.
Conflict of interest
The authors declare no conflict of interest.
Open Research
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.




