Hepatobiliary and Pancreatic: Follicular cholangitis mimicking perihilar cholangiocarcinoma
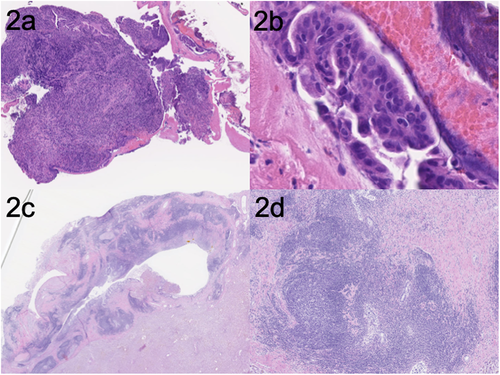
A 73-year-old woman who presented with gradual worsening of liver function was referred to our hospital. She was asymptomatic. Her blood examination showed elevated hepatobiliary enzyme levels. Autoimmune antibodies were all negative, and serum IgG and IgG4 levels remained within normal limits. Contrast-enhanced computed tomography showed wall thickness of the bile duct from the proximal bile duct to the right hepatic duct and dilatation of the right intrahepatic bile duct (Fig. 1a). Endoscopic ultrasonography revealed irregular and low-echoic wall thickness of the bile duct (Fig. 1b). Endoscopic retrograde cholangiopancreatography showed irregular stenosis of the perihilar bile duct. Intraductal ultrasonography showed low-echoic wall thickening with an irregular outer layer (Fig. 1c). Peroral cholangioscopy (POC) revealed polypoid lesion with irregular and tortuous vessels (Fig. 1d). Biopsy from the lesion was performed.
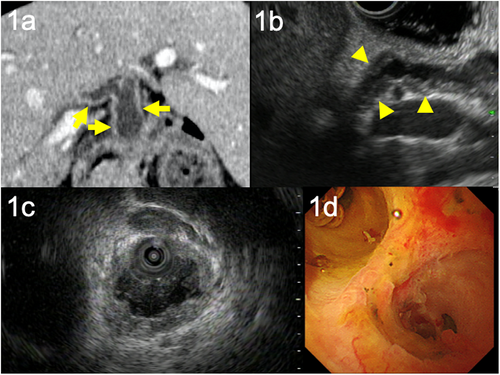
Biopsy from the lesion showed atypical glands, which was suggestive of adenocarcinoma (Fig. 2a,b). Perihilar cholangiocarcinoma IIIB (UICC 8th edition) was diagnosed, and right lobectomy was conducted. The pathology results showed the bile duct wall thickening with dense fibrosis and a marked formation of lymph follicles (Fig. 2c,d) and finally diagnosed with follicular cholangitis.
It is difficult to differentiate follicular cholangitis from perihilar cholangiocarcinoma. There has been no useful imaging modality for diagnosing follicular cholangitis, and POC is expected to be a better diagnostic device; however, it did not enable us to acquire the accurate diagnosis in our case. To our knowledge, this is the first report of follicular cholangitis that has appearance that mimics cholangiocarcinoma on POC. Further study about features of POC in follicular cholangitis should be conducted.