Hepatobiliary and Pancreatic: Symptomatic hepatic splenosis
A 68-year-old man was referred to our hospital with a 6-month history of epigastric and right hypochondrium discomfort with an abdominal computed tomography from the exterior showing a 3.5-cm liver lesion on the right lobule suggestive of hepatocellular carcinoma (HCC). His medical co-morbidities includes hypertension, dyslipidemia, and asthma. In 1975, he had an abdominal trauma required blood transfusion and splenectomy, with no documented liver injury. His laboratory evaluation was notable for normal full blood count, liver enzymes, albumin, coagulation studies, serologies of hepatitis virus, and alpha fetal protein (3 μg/L). Contrast magnetic resonance imaging (MRI) outlined a 3cm lesion in segment 6 that was hypointense on T1 and hyperintense on T2 images, with increased vascularity on contrast administration and washed out during late venous phase (Fig. 1). The rest of the liver was normal. A clinical–radiological diagnosis of HCC/adenoma was made. After multidisciplinary discussion and with refusal of liver biopsy by the patient, he underwent a laparoscopic segmentectomy. The resected liver showed multiple encapsulated nodules of ectopic splenic tissue characterized by white and red pulp (Fig. 2). There was no evidence of malignancy and the rest of the liver parenchyma was normal. The diagnosis of hepatic splenosis was made.
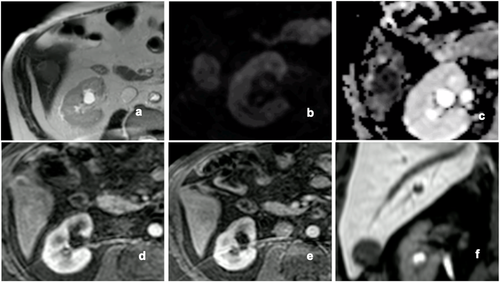
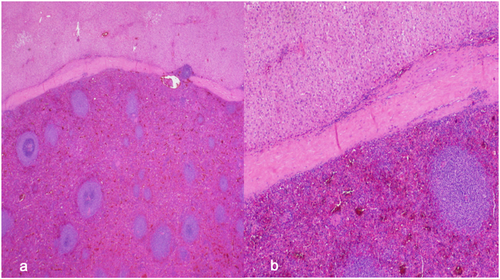
Splenosis is an acquired condition characterized by the presence of heterotopic viable splenic tissue in other organs due to direct seeding or intravascular cell migration after splenic trauma or surgery. This phenomenon is normally diagnosed accidentally during physical or imaging examination due to the associated paucity of symptoms and various possible sites of presentation such as abdominopelvic cavity, pleural cavity, and even brain. Splenic tissue ectopically planted in the liver has been rarely observed and represents an important differential diagnosis of liver masses because it can be misdiagnosed as hepatic cancer. The distinction from liver neoplasia can be made with ultrasound-guided fine needle aspiration cytology and technetium-99 m-labeled heat-denatured RBC scintigraphy when there is a high index of suspicion.
We present a case where due to the biopsy refusal from the patient, a surgical pathology diagnosis of hepatic splenosis was made instead of the HCC/adenoma diagnosis proposed by imaging. Bearing in mind the differences in the prognosis and management of these entities, we highlight the need for a high index of suspicion with the inclusion of abdominal splenosis as a differential diagnosis in patients with an abdominal mass under investigation and prior history of splenic trauma and/or splenectomy.