Hepatobiliary and Pancreatic: Kasabach-Merritt syndrome in adult
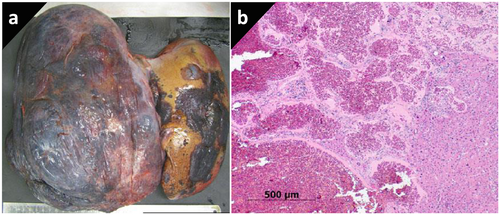
A 57-year-old female with a history of progressively enlarging hepatic hemangiomas presented with blood parameters consistent with a consumptive coagulopathy and microangiopathic hemolysis with pancytopenia, in the absence of liver synthetic failure or portal hypertension. Abdominal computed tomography scan showed a massive liver almost completely replaced by hemangiomas (Fig. 1). The patient was diagnosed with Kasabach–Merritt syndrome and proceeded to liver transplantation. Following transplantation, her cytopenias and coagulopathy resolved, and she remains well at 6-month follow-up.
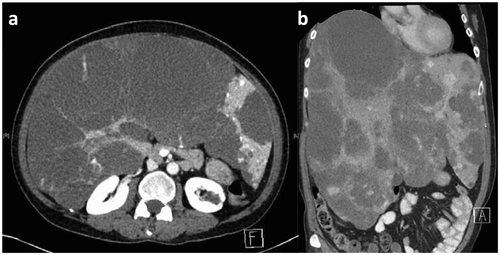
Kasabach–Merritt syndrome, first described in an infant, is a rare association between the consumptive coagulopathy and the presence of giant hemangiomas. While the exact pathophysiology remains unclear, it is theorized that interactions between the clotting factors and the pro-coagulant endothelium of highly vascular and convoluted hemangiomas result in activation of the clotting cascade. Several large pediatric case series have argued that the Kasabach–Merritt syndrome only occurs in patients with kaposiform hemangioendotheliomas or tufted angiomas. However, several case reports in adult literature describe a “Kasabach–Merritt-like” phenomenon occurring in the setting of giant hepatic hemangiomas, which resolves with either resection or liver transplantation. In this case, explant histology demonstrated giant cavernous hemangiomas (Fig. 2).