Resin composite cements: Current status and a novel classification proposal
Abstract
Objectives
Currently, a classification of resin cements that includes relatively recently formulated (“universal”) cements is lacking. Furthermore, the terminology used to define different resin cements in the scientific reports is inconsistent. Accordingly, this work aims to: (i) propose a novel classification of resin composite cements; (ii) disambiguate the term “universal cements” and (iii) present an overview of the properties of these cements.
Methods
An analysis of peer-reviewed literature (PubMed search), as well as market research on definitive resin composite cements were performed.
Results
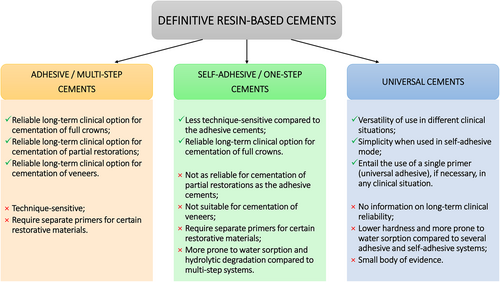
A tendency toward simplified and versatile luting materials was observed both in the scientific literature and on the dental market with the advent of self-adhesive/one-step resin cements. However, additional priming procedures were necessary to improve their bonding performance in certain clinical situations. Hence, several cements that can be applied both in adhesive and self-adhesive mode were introduced. These cements are associated with a universal adhesive resin, that can be used as a tooth and/or restorative material primer, without the need for other priming systems, regardless of the substrate. These systems should be considered truly universal. Therefore, we hereby suggested a new classification of resin-based cements: (1) adhesive/multi-step; (2) self-adhesive/one-step; (3) universal cements (one- or multi-step). Despite promising in vitro results, clinical trials and long-track laboratory studies are necessary to confirm the reliability of the universal cements.
Conclusions
This review presented the current advances in the field of resin-based cements, which are reflected in the proposed classification. The term “universal cement” was disambiguated, which will help standardize the terminology used in published research.
Clinical Significance
The classification of resin-based cements and a better understanding of the proper terminology will help standardize the terminology in published research, as well as improve the understanding of the clinical practitioners of the different indications and possible modalities of use of the available cements.
1 INTRODUCTION
Adhesive dentistry has been making immense steps forward in the previous decades, enabled by the sophistication and innovation of each product used as a part of the adhesive procedures. A clear trend has been noted in the dental market toward simplifying and creating less technique-sensitive materials while maintaining their efficacy.1, 2 Furthermore, versatility of the new adhesive materials enables their employment in a vast array of clinical situations, with the one-bottle/syringe systems also contributing to lower expenditures for the dental office, and less confusion during the adhesive procedures. This trend was particularly reflected in resin-based adhesives and cements.3 Universal adhesives have become sophisticated enough to provide durable bonds between dental substrates and direct restorative materials, with excellent medium-term clinical success.2, 4
The introduction of dual-cure self-adhesive resin cements for indirect restorations reflected the trend of simplification established in the direct adhesive procedures. Although these materials performed rather well in full crowns and enabled adequate bond strength to dentin, their bond strength to enamel demonstrated certain shortcomings, leading to less predictable performance in partial restorations.5 Hence, in clinically challenging situations, such as in the case of short abutments, or bonding to enamel in partial restorations, the use of an additional adhesive layer was deemed necessary. However, there were hurdles regarding chemical incompatibility between the universal adhesives and dual-cured resin cements to be crossed.6, 7 After compositional “fine-tuning”, several manufacturers proposed novel systems, introducing adhesive resin/self-adhesive cement coupled systems, that can be used or individually or together, to “universally” respond to each clinical situation. “Universal” has been a term used rather often in the previous years when it comes to resin-based cements, both in the scientific literature, and on the websites of dental materials' manufacturers. This is not surprising, since it was only natural to call self-adhesive resin-based cements universal due to their ability to bond to various substrates, including dental tissues and different restorative materials. However, with the launch of materials that retain many of the properties of self-adhesive cements, while entailing the possibility of being used both in a multi-step and one-step mode, the authors of this manuscript consider that these systems should be the only ones referred to as truly Universal.
Accordingly, this work aims to suggest a novel classification of resin-based cements and disambiguate the term “universal cement,” as well as attempt to disentangle the advances made in the chemical composition of the universal cement systems and their repercussions on the mechanical properties and the bonding performance of these materials.
2 CLASSIFICATION OF RESIN-BASED CEMENTS
Market research on currently available definitive resin-based cements (Table 1) demonstrated that all the manufacturers developed an adhesive cement, used with the recommended adhesive resin. Adhesive resin cements were developed to meet the necessity for more esthetic and mechanically resistant all-ceramic restorations, that would provide a strong and predictable long-term bonding to tooth tissues.8 These multi-step cements have shown excellent long-term clinical performance.9 However, the adhesive luting procedure is complex and technique sensitive. In everyday clinical practice the performance of technique-sensitive adhesive materials that entail a multi-step adhesive workflow likely does not reach that accomplished in well-controlled randomized clinical trials performed by expert operators.10 Therefore, self-adhesive resin cements have been developed, simplifying the luting procedures considerably. Data from Table 1 clearly confirm the tendency of the dental industry toward simplification, since nearly all manufacturers offer this type of cement alongside adhesive ones. Self-adhesive resin cements are intended for use in a one-step protocol or combined with primers/coupling agents to enhance adhesion on different substrates.11 Self-adhesive cements seem to perform well clinically in association with full metal-ceramic and all-ceramic crowns for up to 6 and 10 years, respectively.12, 13 However, a recent systematic review of laboratory studies reported that multi-step resin cements provide higher bond-strength values to coronal dentin at baseline as well as after artificial aging when compared to self-adhesive resin cements.14 Also, the latter demonstrated similar or slightly lower mechanical properties, higher wear and increased hydrophilicity, making them more prone to water sorption than the adhesive cements.1, 15, 16 These properties were reflected in the clinical performances of partial restorations cemented with self-adhesive or adhesive cements.5, 17, 18
| Manufacturer | Cement name | Adhesion modality | Curing option | Functional Monomer | Suggested adhesive | Pretreatment tooth | Pretreatment restoration |
|---|---|---|---|---|---|---|---|
| Bisco | Duo-link Universal | Adhesive | Dual-cure | // | // | // | Ceramic primer or zprimer |
| Choice 2 | Adhesive | Light-cure | // | // | // | Ceramic primer or zprimer | |
| eCement | Adhesive | Light-cure version or Dual-cure version | // | All bond Universal | // | Porcelain primer | |
| BisCem | Self-adhesive | Dual-cure | // | // | // | Ceramic primer or zprimer | |
| TheraCem | Self-adhesive | Dual-cure | 10-MDP | // | // | Silane for ceramic | |
| Coltene/Whaledent | Paracore | Adhesive and Core cement | Dual-cure | // | ParaBond chemical cured | // | // |
| Duocem | Adhesive | Dual-cure | // | // | // | // | |
| Solocem | Adhesive or Self-adhesive | Dual-cure | 10-MDP 4-META |
One coat 7 universal | // | // | |
| Dentsply Sirona | Calibra Ceram | Adhesive | Dual-cure | PENTA | Prime&Bond® active | // | // |
| Calibra veneer | Adhesive | Light-cure | // | Prime&Bond® active | // | // | |
| Calibra Universal | Self-adhesive | Dual-cure | PENTA | // | // | // | |
| DMG | PermaCem Universal | Adhesive | Dual-cure | // | LuxaBond Universal | // | // |
| PermaCem | Adhesive | Dual-cure | // | LuxaBond | // | // | |
| Vitique | Adhesive | Light-cure | // | // | // | // | |
| PermaCem 2.0 | Self-adhesive | Dual-cure | 10-MDP | // | // | // | |
| GC | G-Cem Linkforce | Adhesive | Dual-cure | // | G-Premio Bond | // | G-Multiprimer |
| G-Cem Veneer | Adhesive | Light-cure | Silane | G-Premio Bond | // | // | |
| G-Cem Capsule | Self-adhesive | Dual-cure | 4-META | // | // | // | |
| G-Cem ONE | Self-adhesive | Dual-cure | 10-MDP | // | Adhesive enhancing primer (optional) (Contains 10-MDP) | G-multi Primer | |
| Hareaus Kultzer | iCEM | Self-adhesive | Dual-cure | // | // | // | // |
| Ivoclar | Variolink Esthetic | Adhesive | Light-cure or Dual-cure version | // | Adhese universal | // | Monobond plus |
| Multilink automix | Adhesive | Dual-cure | // | // | Multilink Primer | Monobond plus | |
| SpeedCEM Plus | Self-adhesive | Dual-cure | 10-MDP | // | // | // | |
| Kerr | Nexus Universal | Adhesive | Dual-cure | // | Optibond Universal | // | // |
| Maxcem Elite | Self-adhesive | Dual-cure | GPDMA | // | // | // | |
| Maxcem Elite chroma | Self-adhesive | Dual-cure | // | // | // | // | |
| Kuraray Noritake | Panavia V5 | Adhesive | Dual-cure | // | // | Tooth primer (contains 10-MDP) | Clearfil Ceramic Primer Plus |
| Panavia Veener LC | Adhesive | Light-cure | // | // | Tooth primer (contains 10-MDP) | Clearfil Ceramic Primer Plus (contains 10-MDP) | |
| Panavia F 2.0 | Adhesive | Dual-cure | 10-MDP | // | ED primer II A + B (contains 10-MDP) | Alloy primer, ceramic primer (contain 10-MDP) | |
| Panavia 21 | Adhesive | Dual-cure | // | // | ED primer A + B (contains 10-MDP) | Alloy primer, ceramic primer (contain 10-MDP) | |
| Panavia SA Universal | Adhesive or Self-adhesive | Dual-cure | 10-MDP LCSi | Clearfil Universal Bond Quick | // | // | |
| Shofu | ResiCem | Adhesive | Dual-cure | // | // | Primer A and B | AZ primer; HC Primer; Porcelain Primer; SHOFU Universal Primer. |
| BeautyCem SA | Self-adhesive | Dual-cure | phosphonic acid monomers | // | // | Ceramic primer | |
| Tokuyama | Estecem II Plus | Adhesive | Self-cure | // | Universal Bond II A and B | // | // |
| Ultradent | PermaFlo DC | Adhesive | Dual-cure | // | Peak Universal Bond | // | // |
| PermaShade LC | Adhesive | Light-cure | // | Peak Universal Bond | // | // | |
| 3 M ESPE | RelyX Ultimate | Adhesive | Dual-cure | // | Scotchbond Universal (contains 10-MDP and Silane) | // | // |
| RelyX Veneer Cement | Adhesive | Light-cure | // | Adper Single Bond Plus | // | RelyX Ceramic Primer | |
| Relyx Universal | Adhesive or Self-adhesive | Dual-cure | Mixture of GPDMA, bisGPDMA and trisGPDMA | Scotchbond Universal Plus (optional) (Contain 10-MDP and Silane) | // | // | |
| Relyx Unicem 2 | Self-adhesive | Dual-cure | Mixture of GPDMA, bisGPDMA and trisGPDMA | // | // |
- Note: The present list is not exhaustive and is based predominantly on the European market. Any omission of a product is unintentional. Product information was retrieved from the currently available SDS sheets and manufacturers' websites.
- Abbreviations: 10-MDP, 10-Methacryloyloxydecyl dihydrogen phosphate; 4-META, 4-methacryloxyethyl trimellitic anhydride; bisGPDMA, bis(gliceryldimethacrylate) phosphate; GPDMA, glycerol phosphate dimethacrylate; LCSi, long carbon-chain silane coupling agent; PENTA, dipentaerythritol penta-acrylate phosphate; trisGPDMA, tris(glyceryldimethacrylate) phosphate.
The choice of resin cement seems less important in case of zirconia or lithium-disilicate full-crowns, given that they show good clinical performance both with multi- and one-step luting procedures.19 Similarly, partial glass-ceramic indirect restorations can be successfully luted with both self-adhesive and adhesive resin cements with no major differences in clinical outcome in short-term period (up to 1-year of follow-up).20 However, it is important to mention that adhesive cements are more performant after 18 months,17 39 months5 and over 6 years.18, 21 As for fiber posts, laboratory studies report that self-adhesive cements can provide higher push-out bond-strength values compared to adhesive ones, possibly providing better retention.22 However, a multi-centered randomized clinical trial reported that both self-adhesive and adhesive resin cements are valid options for adhesive luting of glass fiber posts, with a mean observation time of 3 years.23
As it can be seen from the above-mentioned, certain discrepancies may exist between laboratory and clinical trials, and the right choice of cement depends on the substrate and clinical situation. Overall, self-adhesive cements seem to perform well in retentive restorations – full crowns and intraradicular fiber posts,13, 23, 24 but could present certain shortcomings (reduced life-span and esthetic-related problems) when faced with less retentive types of preparations, such as partial crowns5 or short abutments. For partial indirect restorations and in the presence of enamel as substrate, the use of self-adhesive resin cements alone is not indicated, as they cannot guarantee optimal clinical outcome and durable retention.25, 26 Therefore, adhesive cements are more adequate in this case, although they may show a higher risk for the development of post-operative sensitivity when used with an E&R adhesive system. This post-operative sensitivity is usually resolved spontaneously, within days or weeks after the luting procedure, as commonly reported in clinical trials.27 To avoid intense initial post-operative sensitivity, it is advisable to limit the etching to enamel only and avoid dentin contamination with phosphoric acid.26
Although developed to simplify clinical procedures without jeopardizing the longevity of restorations, self-adhesive cements have failed to provide predictable clinical behavior of esthetic partial restorations and (in the majority of cases) require pre-treatment of composite and ceramic surfaces with a silane coupling agent, or 10-MDP primer in case of zirconia. Aiming to meet diverse clinical needs and resolve the conundrum of the materials available on the market and stocked in dental offices, several manufacturers developed cements that are indicated for use both in self-adhesive, and, when coupled with their recommended universal adhesives, in the adhesive mode. Moreover, these cement-adhesive resin systems are recommended for luting of metallic, composite, ceramic, and zirconia-based restorations, without the need for additional primers, and could therefore be considered truly “universal”.
- be indicated for application in self-adhesive, and adhesive (self-etch, selective enamel etch, or etch-and-rinse mode) luting protocols, depending on the clinical requirements and clinicians' preference;
- be indicated for luting to tooth tissues, as well as metallic, silica-based and zirconia-based restorative materials;
- be associated with a recommended universal adhesive resin, that can be used as a tooth and/or restorative material primer, without the need for other priming systems;
- at least one of the universal cement/adhesive resin system components should contain functional acidic monomers and preferably silane-coupling molecules, to ensure chemical bridging between the cementation substrates (tooth tissues and restorative materials)
- be a dual-cure material.
An important distinguishing between resin cements (independent of the luting mode) should also be made according to their curing mode (light-cure, chemical-cure or dual-cure), as shown in Table 2. According to this classification, it was interestingly noted that the majority of the currently available cements are dual-cure, while only one product has been purported as chemical-cure. Also, a line of light-cure cements is present, usually named “esthetic” or “veneer” and intended for use, as their name indicates, in the esthetic zone, accounting for the low thickness and sufficient translucency of dental veneers which enables adequate light-curing. These cements are always adhesive, due to the fact that the main cementation substrate in these cases is enamel, which undoubtedly benefits from etching and adhesive resin placement to ensure the longevity of the resin-dentin bonds.25, 28, 29
| Light-cure | Chemical-cure | Dual-cure |
|---|---|---|
| Choice 2 (Bisco) | Estecem II (Tokuyama) | Duo-link Universal (Bisco) |
| aeCement (Bisco) | aeCement (Bisco) | |
| Calibra Veneer (Dentsply Sirona) | TheraCem (Bisco) | |
| Vitique (DMG) | BisCem (Bisco) | |
| G-Cem Veneer (GC) | Paracore (Coltene/Whaledent) | |
| Panavia Veener LC (Kuraray Noritake) | Solocem (Coltene/Whaledent) | |
| PermaShade LC (Ultradent) | Duocem (Coltene/Whaledent) | |
| RelyX Veneer Cement (3M ESPE) | Calibra Ceram (Dentsply Sirona) | |
| Calibra Universal (Dentsply Sirona) | ||
| PermaCem Universal (DMG) | ||
| PermaCem 2.0 (DMG) | ||
| PermaCem (DMG) | ||
| G-Cem LinkAce (GC) | ||
| G-Cem Linkforce (GC) | ||
| G-Cem Capsule (GC) | ||
| G-Cem ONE (GC) | ||
| iCEM (Hareaus Kultzer) | ||
| aVariolink Esthetic (Hareaus Kultzer) | aVariolink Esthetic (Hareaus Kultzer) | |
| Multilink automix (Ivoclar) | ||
| SpeedCEM Plus (Ivoclar) | ||
| Nexus Universal (Kerr) | ||
| Maxcem Elite (Kerr) | ||
| Maxcem Elite chroma (Kerr) | ||
| Panavia V-5 (Kuraray Noritake) | ||
| Panavia SA Universal (Kuraray Noritake) | ||
| Panavia F 2.0 (Kuraray Noritake) | ||
| Panavia 21 (Kuraray Noritake) | ||
| BeautyCem SA (Shofu) | ||
| ResiCem (Shofu) | ||
| PermaFlo DC (Ultradent) | ||
| Relyx Universal (3M ESPE) | ||
| Relyx Unicem 2 (3M ESPE) | ||
| RelyX Ultimate (3M ESPE) |
- a Cements available in 2 versions – light-cure and dual-cure.
Several cements are produced in two versions, a light-cure and a dual-cure option (Table 2). While light-cure cements are one-syringe materials, the dual- and chemical-cure materials are necessarily present in two bottles to separate the components of the chemical curing reaction and prevent premature polymerization. The chemical curing initiators, aromatic amine and benzoyl peroxide are more prone to color changes compared to the photo-initiating components – camphorquinone and aliphatic amine.30 Furthermore, certain light-cure cements demonstrated higher degree of conversion (DC) and microhardness compared to dual-cure cements,31 possibly due to differences in the polymerization kinetics and differences in the compositions and filler load and type.32 However, it is important to emphasize that the mechanical and curing properties of resin cements are highly material-dependent,33 and it is therefore difficult to draw generalized conclusions on a certain group of cements.
3 UNIVERSAL CEMENTS
Universal cements are essentially next-generation self-adhesive cements, although the concept behind the two remains similar. Universal cements are furnished in a two-paste system intended to separate parts of the redox system, the acidic and near neutral, as well as hydrophilic and hydrophobic counterparts. The modification of the compositions of the new generation of cements intended to enable them to work in synergy with their recommended universal adhesives, avoid possible curing incompatibilities, and ensure optimal interaction with both dental substrates and restorative materials.
Among the cements present on the market at the moment of this research process, it seems that only three products meet all the criteria to be classified as “universal cements”: RelyX Universal (RXU, 3M Oral Care, St Paul, MN, USA) coupled with Scotchbond Universal Plus, Panavia SA Universal (PSAU, Kuraray Noritake Dental Inc, Okoyama, Japan), recommended with Clearfil Universal Bond Quick, and SoloCem (SOC, Coltène/Whaledent, Altstätten, Switzerland) and OneCoat 7 Universal adhesive. Their detailed compositions and the compositions of the universal adhesive resins they are coupled with are presented in Table 3. The available data on the mechanical properties and bonding performance of universal cements will be presented in the next sections.
| Manufacturer | Universal cement | Universal adhesive resin |
|---|---|---|
| 3M ESPE | 3M RelyX Universal Resin Cement | 3M Scotchbond Universal Plus Adhesive |
| Base paste: | Brominated dimethacrylate | |
| γMPTES, reaction products with vitreous silica | HEMA | |
| DUDMA | 10-MDP | |
| TEGDMA | 2-Propenoic acid, 2-methyl-, 3-(triethoxysilyl)propylester, reaction products with silica and 3-(triethoxysilyl)-1-propanamine | |
| Mixture of GPDMA, bisGPDMA and trisGPDMA | Ethanol | |
| Silane treated silica | Water | |
| t-Amyl Hydroperoxide | Synthetic amorphous silica, fumed, crystalline-free | |
| 2,6-Di-tert-butyl-p-cresol | γMPTES | |
| HEMA | Camphorquinone | |
| Methyl Methacrylate | Copolymer of acrylic and itaconic acid | |
| Acetic acid, copper(2+) salt, monohydrate | N,n-dimethylbenzocaine | |
| APTES | ||
| Catalyst paste: | DEGDMA | |
| DUDMA | Acetic acid, copper(2+) salt, monohydrate | |
| Ytterbium (III) fluoride | ||
| Silane-treated glass powder, | ||
| TEGDMA | ||
| L-Ascorbic acid, 6-hexadecanoate, hydrate (1:2) | ||
| Silane treated silica | ||
| HEMA | ||
| Titanium Dioxide | ||
| Triphenyl Phosphite | ||
| Kuraray Noritake | PANAVIA SA Cement Universal | CLEARFIL Universal Bond Quick |
| Paste A | Bis-GMA | |
| 10-MDP | ethanol | |
| Bis-GMA | HEMA | |
| TEGDMA | 10-MDP | |
| Hydrophobic aromatic dimethacrylate | Hydrophilic amide monomers | |
| HEMA | Colloidal silica | |
| Silanated barium glass filler | Silane coupling agent | |
| Silanated colloidal silica | Sodium fluoride | |
| Camphorquinone | Camphorquinone | |
| Peroxide | Water | |
| Catalysts | ||
| Pigments | ||
| Paste B | ||
| Hydrophobic aromatic dimethacrylate | ||
| Silane coupling agent (LCSi proprietary monomer) | ||
| Silanated barium glass filler | ||
| Aluminum oxide filler | ||
| Surface treated sodium fluoride (Less than 1%) | ||
| Camphorquinone | ||
| Accelerators | ||
| Pigments | ||
| Coltène/Whaledent | SoloCem | OneCoat 7 Universal |
| TEGDMA | DUDMA | |
| DUDMA | HEMA | |
| Bis-GMA | 10-MDP | |
| HEMA | Ethanol | |
| Zinc oxide; | Diphenyliodonium chloride | |
| ytterbium(III) fluoride | Diphenyl(2,4,6-trimethylbenzoyl)phosphinoxid | |
| 2,6-di-tert-butyl- 4-methylphenol | ||
| 10-MDP | ||
| dibenzoyl peroxide (BPO initiator) | ||
| 4-META |
- Note: The information on the composition of the materials was obtained from the manufacturers' websites and SDS documents.
- Abbreviations: 10-MDP, 10-Methacryloyloxydecyl dihydrogen phosphate; 4-META, 4-methacryloxyethyl trimellitic anhydride; APTES, (3-aminopropyl)triethoxysilane; Bis-GMA, Bisphenol A diglycidylmethacrylate; bisGPDMA, bis(gliceryldimethacrylate) phosphate; DEGDMA, Diethylene glycol dimethacrylate; DUDMA, diurethane dimethacrylate; GPDMA, glycerol phosphate dimethacrylate; HEMA, 2-Hydroxymethacrylate; LCSi, long carbon-chain silane coupling agent; TEGDMA, Triethyleneglycol dimethacrylate; trisGPDMA, tris(glyceryldimethacrylate) phosphate; γMPTES, 2-Propenoic acid, 2-methyl-, 3-(trimethoxysilyl)propyl ester.
3.1 Physical properties of universal cements
Given that the majority of the universal cements have been marketed relatively recently, the reports on their laboratory and clinical performances are scarce.
Recently, a series of 3 papers has been published on the physical properties of RXU compared to several self-adhesive cements (including the direct predecessor of RXU – RelyX Unicem2, 3M ESPE), and several multi-step cement systems.34, 35 Higher shrinkage of RXU compared to other investigated cements was reported, possibly due to lower inorganic filler content.34 In terms of hardness, RXU demonstrated lower values compared to other investigated cements, with the values always being higher in the dual-cure mode for all the cements.35 The total elution of monomers from RXU cement was lower or comparable to the investigated self-adhesive and multi-step cements.36 This was supposedly related to the absence of bisphenol A glycidyl methacrylate (Bis-GMA) in both RXU and Scotchbond Universal Plus adhesive. In particular, bis-GMA is manufactured from bisphenol A (BPA), that was shown to activate estrogen receptors and act as a risk factor for fertility, and even induce deterioration of psychological health in children.37 It is important though to mention that all the cements eluted monomers well below the half-maximal-effect concentration levels. The water sorption of RXU was found to be comparable or lower than several self-adhesive cements, but higher than the investigated adhesive multi-step cements.36 The same study demonstrated that the solubility of RXU was comparable to, or lower, than the other investigated cements. Since water sorption is related to color stability of resin-based materials,38 these findings are in accordance with the results of another recent study on the color stability of resin cements.39 This group of authors found that the color stability of RXU was comparable to Panavia SA and lower than Panavia V5 (tested also in the previously mentioned study). However, RXU demonstrated higher color change compared to other investigated self-adhesive cements. This could be due to differences in the composition of the resin matrix and filler content and size.38
Polymerization stress to feldspathic ceramics of SOC compared to 8 different self-adhesive cements (all employed after a silane pretreatment) was demonstrated to be comparable or lower when the universal cement was used.40 This cement also demonstrated higher water sorption compared to 7 self-adhesive cements.41 The same study affirmed, however, that this material is more stable than the majority of the other investigated cements color-wise after 1 year of storage in different dying solutions,41 which could be contradictory. Another study investigated the color stability of adhesive and self-adhesive cements after an accelerated aging protocol (2 weeks of consecutive UV light at 60°C for 4 h and vapor condensation at 50°C for 4 h).42 All the investigated cements exhibited significant color changes after accelerated aging, apart from Panavia F 2 (Kuraray Noritake), which performed significantly better. In terms of mechanical properties, SOC showed similar hardness and indentation modulus to the majority of other investigated cements (7 self-adhesive cements).43 After 180 days of storage in a NaCl solution, the mechanical properties of SOC did not decrease, while there was a significant decrease in the properties of the cement stored in physiological saliva, artificial saliva and distilled water. In general, the materials with a higher filler content showed higher hardness.43
To the best of our knowledge, there is currently no available data in the literature on the physical properties of PSAU.
3.2 Interaction of universal cements with dental tissues
Universal cements are required to bond predictably to tooth substrates. Therefore, functional acidic monomers are incorporated into their composition. These monomers are intended to etch and infiltrate the dental substrate, forming chemical bonds with Ca2+ ions from hydroxyapatite, as well as with methacrylate monomers, performing somewhat a “silanization” of the tooth surface. Although several functional acidic monomers are currently used in dental cements, such as 4-methacryloxyethyl trimellitic acid (4-MET), 4-methacryloxyethyl trimellitic anhydride (4-META), and dipentaerythritol penta-acrylate phosphate (PENTA), the gold standard functional monomer at present is surely 10-methacryloyloxydecyl dihydrogen thiophosphate (10-MDP). This phosphoric acid-spacer-methacrylate group molecule forms very strong and stable bonds with hydroxyapatite,44 forming 10-MDP-Ca salts, as well as hydrogen bonds with collagen molecules.45 On the other end, this molecule bonds with the carbon chain of the resin monomers.45 Additionally, 10-MDP and 10-MDP-Ca salts inhibit endogenous dentinal matrix-metalloproteinases shown to degrade the hybrid layer and diminish the longevity of resin-dentin bonds.46, 47
All three universal resin cements, or the universal adhesives they are associated with, contain 10-MDP, and/or other functional monomers. This surely impacts their bonding performance to tooth tissues and restorative materials. RXU combined with the pertinent adhesive demonstrated bond strength to dentin and enamel comparable to Panavia V5 (Kuraray Noritake)48 and G-Cem One self-adhesive cement (GC, Tokyo, Japan)49 placed with the G-Cem One Adhesive Enhancing Primer (GC), while in enamel, the universal system yielded lower results or at baseline (compared to G-Cem One, GC), or after thermocycling (compared to Panavia V5, Kuraray Noritake).48 Bond strength of RXU comparable or better than several self-etch and multi-step cements was also demonstrated in root dentin.50
PSAU, on the other hand, demonstrated comparable shear bond strength to dentin as its predecessor Panavia SA Plus (Kuraray Noritake), both employed in self-adhesive mode.51 Another group of authors partially confirmed these results, as microtensile bond strength to dentin was comparable when these two cements were applied directly on dentin in dual-cure mode, while in the self-cure mode and in the groups where prior resin coating was applied on dentin, Panavia SA Plus demonstrated better bonding performance.52 Bond strength on tooth tissues using PSAU with Universal Bond Quick has still not been tested but might further improve bond strength values, as indicated in patent literature. A proprietary amide monomer was introduced into the formulation of this adhesive resin, which supposedly lowers the surface tension of the bonding substrate and allows for an immediate impregnation with the adhesive resin, without the need to wait or active application. Our internal research confirmed that the shear bond strength to dentin of both RXU and PSAU benefits from the application of the pertinent universal adhesive (unpublished results). These results need to be further pursued and replicated.
Although SOC is the first marketed universal cement, to the best of our knowledge there are no reports in the literature on bonding performances of this cement to tooth tissues, or restorative materials.
3.3 Interaction of universal cements with the restorative materials
It is naturally equally important for universal cements to bond predictably to restorative materials. Bond strength of RXU cement system on composite, polymer-infiltrated ceramic, lithium disilicate, feldspar ceramic, and zirconia was higher than that of Panavia V5 coupled with the ceramic primer (Kuraray Noritake)48 and comparable to lithium-disilicate to that of G-Cem One used with the G-MultiPrimer (GC).49 PSAU demonstrated comparable bond strength to ceramics to Panavia SA Plus (Kuraray Noritake) used with a separate ceramic primer.51 However, it seems that the application of a separate silane further improves bond strength of PSAU to ceramics.53 In fact, the hydrophobicity of the polished or HF-etched lithium-disilicate surfaces was higher in groups treated with a silane-containing primer compared to the PSAU-treated groups, possibly due to the better rheological properties of the silane in the liquid primer compared to the one in the cement, which has a higher viscosity.53 Furthermore, when bonding to composite materials, a system that employs a primer showed better bonding performance compared to the PSAU universal cement used in self-adhesive mode.54 The apparent efficacy of these two novel universal luting systems to silanize glass ceramics was made possible through adjustments in their chemical composition. In the RXU + Scotchbond Universal Plus system, it is the adhesive resin that contains a mixture of silanes and is recommended for use as a primer for ceramic and composite-based restorations. However, it was reported in a recent meta-analysis that universal adhesives advocated as ceramic primers are less effective compared to separate silanes.55 This is probably due to the acidic and hydrophilic nature of the universal adhesives which likely cause premature condensation of the most commonly used silane monomers, such as methacryloxypropyl trimethoxysilane (γ-MPTS). Nevertheless, the Scotchbond Universal Plus adhesive contains alternative silane molecules, 3-(aminopropyl)triethoxysilane and γ-methacryloxypropyltriethoxysilane, that might be more resistant to the hydrophilic acidic environment, as demonstrated by the previously mentioned studies.48, 49 On the other hand, a proprietary long-chain silane monomer was added directly to Panavia SA Universal cement, in the more hydrophobic and pH neutral paste. This seems to have prevented the premature hydrolysis of the silane molecule. Since separate silane primers are probably activated by atmospheric water,56 there might be concerns that a highly viscous mixture of cement pastes could not effectively use water from the atmosphere to hydrolyze the silane-coupling monomer.51 However, it was clearly demonstrated by means of an NMR analysis that the silane-coupling monomer undergoes hydrolysis upon mixing of the two pastes, possibly due to water absorbed onto glass,51 as well as to the water molecules released in the setting mechanism of the cement. As for the SOC, although the manufacturer recommends luting of composite, ceramic and zirconia restorations without any pretreatment, it is not clear whether this universal cement contains a silane. This information is not provided by the manufacturer and according to the SDS information, it does not seem to be the case.
It should be noted that the bonding performance of resin cements can be greatly influenced by the restoration's mechanical and chemical surface treatment. For instance, shear bond strength of PSAU to differently pretreated translucent zirconia (alumina sandblasting, several protocols for silica coating) was recently tested.57 In this study, at baseline, PSAU performed better or equally well than the other luting protocols (Panavia SA Plus with or without a silane/universal adhesive pretreatment) regardless of the chemo/mechanical treatment of the translucent zirconia. After thermocycling, nearly all the tested groups had a significant decrease in bond strength. PSAU still performed better on silica-coated surfaces than the protocols that did not contain silane, but worse than those that entailed a separate silane application.57
It is indeed tempting to simplify the luting procedures, and adhesive procedures in general, and preferably blend in all the different components that might come in handy during this process, such as a silane and 10-MDP, but these must be performed with caution, since, for instance, 10-MDP might cover some of the γ-MPTS free methacrylate groups, and therefore these molecules could cancel each other's effect.58 Moreover, although the silane formulation within the universal adhesive or universal cement seem to provide a rather efficient chemical bond strength to different types of ceramics, it is paramount that these materials are resistant to hydrolytic degradation. It was recently reported that the application of Scotchbond Universal Plus + RXU on several novel lithium disilicate glass ceramics yielded bond strength at baseline comparable to the groups where an additional silane was used.59 However, after thermocycling, the bond strength in the groups pretreated only with the universal adhesive decreased significantly more. This could indicate that the silane-containing universal adhesive is more prone to hydrolytic degradation, which could have led to plasticization of the adhesive layer, and monomer leaching due to breaking of the polymer covalent bonds.
3.4 Considerations on polymerization efficacy
Universal cements are dual-cure materials, meaning that free radical polymerization is initiated both by a redox chemical and a photo-initiation route. This enables their polymerization in the areas of difficult access to curing light. Adequate polymerization of resin-based cements is essential for their mechanical properties and long-term bonding performances.60 This was also demonstrated in the reports from the previous sections, where dual-cure groups nearly always demonstrated superior physical properties as well as bonding performance compared to their chemical-cure counterparts. In the dual-cure products, the different polymerization initiation and acceleration components are divided into separate pastes to prevent their premature activation. As the components introduced in the acidic paste need to be acid-resistant, the polymerization initiators added in self-adhesive and universal cements had to be modified accordingly. Hence, benzoyl peroxide and tertiary amines needed to be replaced with other oxidants, and reductants, such as cumene hydroperoxide and various thioureas.1 As regards the photo-initiation, apart from the traditional camphorquinone (1,7,7-trimethylbicylo[2.2.1]heptane-2,3-dione, CQ)/amine complex, other, more efficient initiators, such as diphenyl-(2,4,6-trimethylbenzoyl) phosphine oxide (TPO) have been added in self-adhesive and universal cements (Table 3). To improve the acid-resistance of chemical and photoinitiators, aryl borate salts, as well as sodium aryl sulfates, have been introduced.6 Aryl borate salts can also contribute to the curing activation of dual-cure resin-based cements, as part of the “touch-cure” polymerization strategy, intended to improve the monomer network formation in areas with limited exposure to the curing light.61
The polymerization initiates once the two pastes are mixed and the inhibitor, added to slow down the setting and enable an adequate working time, has been consumed. During the setting of the cement, which is initially hydrophilic and acidic, the functional acidic monomers react both with hydroxyapatite and alkaline fillers. Consequently, the tooth tissues are slightly demineralized, and the functional monomers are bound chemically to hydroxyapatite.11 The remaining portion of the acidic monomers is neutralized through a reaction with cement fillers.62 As the reaction proceeds, the cement's pH increases, and the water molecules released in the reaction are reused, supposedly leading to the formation of a more hydrophobic material.63 It is important to emphasize that very often clinically the cementation substrate is not dentin or enamel, but a composite build-up material, meaning that the setting and neutralization reaction of the acidic monomers relies solely on their reaction with the ion-leachable glass fillers.16 This could lead to inadequate polymerization of the cement, and deterioration of its mechanical properties. Namely, acidic monomers can inhibit the amine accelerators necessary for photopolymerization.64 Further, unreacted hydrophilic acidic monomers can determine higher water sorption and solubility of the cements.64
The information on the curing efficacy of universal cements is scarce. A recent study comparing the RXU to several one- and multi-step cement systems reported that DC of RXU was comparable to other investigated cements. Interestingly, the DC in self-cure mode reached that of the dual-cure mode after 24 h and the DC was higher in RXU compared to its self-adhesive predecessor.34 These results could corroborate the manufacturer's claims on introducing a novel amphiphilic polymerization initiator system that should supposedly initiate polymerization effectively both in the segments of the cement layer that are in contact with dentin, and the more hydrophobic portion of the cement layer. Furthermore, in order to avoid incompatibility of the polymerization initiation between the adhesive resin and the cement and to enable chemical curing initiation of universal adhesives during the luting procedures, polymerization accelerators (Scotchbond Universal Plus for RXU), or dual-cure activators (Clearfil Bond Quick for PSAU) were introduced in their formulations, precluding the need for polymerization before the application of the cement. OneCoat 7 Universal is the only adhesive in the universal cement/adhesive systems that requires polymerization prior to luting. The efficiency of the polymerization activation of PSAU by Clearfil Bond Quick was demonstrated in a recent report,53 since the application of Clearfil Bond Quick before the cement significantly increased (p < 0.05) the degree of conversion of the cement in self-cure mode. In dual-cure mode however, the DC was not influenced by the adhesive resin application and was comparable to the DC of PSAU's predecessor in the dual-cure mode, and higher in the self-cure mode.
4 CONCLUDING REMARKS
Definitive resin-based cements demonstrated to be beyond a doubt a highly esthetic, and reliable choice for luting of indirect restorations. Considering the plethora of resin-based cements available on the market, note should be taken that cements that belong to the same category can have different chemical compositions and performances. One might be more reliable on tooth tissues, while another might perform markedly better in a certain type of restoration. Therefore, the available laboratory and clinical studies should be interpreted with caution, more associated with the specific material tested, than with the group of materials. Only after obtaining an important body of evidence on a vast array of available materials in each group can there be generalizable conclusions on laboratory and clinical outcomes. We therefore encourage researchers to investigate the performance of cements that have not been investigated so far and contribute to the pool of knowledge on different categories of resin-based cements. Further, long-term independent clinical trials on universal resin-based cements are needed.
It is still early to say whether the current universal resin cements will actually reach the goals they were set out to achieve, or will they be deemed inadequate, like the early one-bottle adhesives. The universal cements however build up on the experience already gained with self-adhesive cements. They inevitably also inherited certain shortcomings of the self-adhesive cements, being more hydrophilic and acidic than the adhesive ones. Nevertheless, it is clear that massive efforts have been invested, and important advances accomplished in terms of dental cements' versatility and simplification, while minding their reliability. Therefore, we consider that the new classification proposed in the present work reflects and appreciates these current advances. Undoubtedly, modification of the present classification will be warranted with future developments in adhesive dentistry.
DISCLOSURE
The authors declare that they do not have any financial interest in the companies whose materials are included in this article.
ACKNOWLEDGMENTS AND DISCLOSURE
Open Access Funding provided by Universita degli Studi di Bologna within the CRUI-CARE Agreement.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.