The use of lasers in vitiligo, an overview
Funding sources
None.
Conflicts of interest
None declared.
Abstract
Various types of lasers have been demonstrated to be effective in the treatment of vitiligo. The mode of action of these lasers is just as varied as the purpose of intervention. Many clinicians are not aware of the unique opportunity these lasers offer to improve the outcomes of vitiligo treatment. To date, no clear overview exists of the use of lasers in vitiligo treatment. Thus, the aim of this review is to discuss the various types of lasers and provide an overview of the evidence for their efficacy. We found good evidence from a systematic review that the excimer laser is effective, induces repigmentation rates comparable to NB-UVB and has improved outcomes when combined with calcineurin inhibitors. Ablative lasers are commonly used for tissue graft or melanocyte–keratinocyte cell graft transplantation. They provide safe, fast and uniform denudation of the epidermis with propitious repigmentation outcomes. We found conflicting evidence from two systematic reviews regarding the efficacy of fractional ablative lasers for improving outcomes of NB-UVB therapy, a systematic review including only fractional ablative lasers provided evidence for efficacy. Q-switched nanosecond lasers have shown to be safe and effective for inducing depigmentation, although recurrence is common, and most studies were small and retrospective. Despite proven efficacy and safety, laser treatments are relatively expensive and suited for limited body surface areas and selected cases. Each type of laser has benefits and risks associated and should, therefore, be individually chosen based on location, extent, activity and type of vitiligo.
Introduction
Vitiligo is a psychologically impairing autoimmune disorder inducing skin depigmentation that affects 0.2–1.8%1 of the population and has a major impact on the quality of life.2 The mainstay of treatment consists of topical/systemic immunosuppressant’s and phototherapy, which serve to stabilize depigmented lesions and to stimulate repigmentation in both stable and unstable vitiligo. Tissue graft or melanocyte–keratinocyte cell graft transplantation (MKT) provides a more definitive surgical option for patients with stable and localized vitiligo or with segmental vitiligo who have failed repigmentation, despite topical treatments and light therapy. In addition, various types of lasers, used as both monotherapy and combination therapy, have been demonstrated to be effective in the treatment of vitiligo. The mode of action of these lasers is just as varied as the purpose of intervention and involves photo biomodulation for repigmentation (excimer lasers), photo ablation for recipient site preparation before grafting (ablative lasers), tissue stimulation to enhance efficacy of phototherapy (fractional lasers) and photo mechanic interactions for depigmentation (Q-switched lasers). Many clinicians are not aware of the various types of lasers that improve the outcomes of vitiligo treatment. Therefore, we aim to discuss the various types of lasers used in vitiligo and the evidence for their efficacy.
Excimer laser
The 308-nm excimer laser (EL), a targeted phototherapy device, was first described in 2002 for repigmentation of vitiligo.3 The EL emits coherent and monochromatic light at 308 nm, which is adjacent to 311 nm narrowband-UVB (NB-UVB) and has similar effects. It is indicated for depigmented body surface areas (BSA) <10% and has the advantage of not affecting surrounding skin.2 Similar to NB-UVB, the EL inhibits inflammation and induces T-cell apoptosis. In addition, the EL induces the differentiation of melanocyte stem cells, stimulates the production of melanin and the proliferation and migration of melanocytes inducing repigmentation.4 There is strong evidence demonstrating the efficacy of EL in treating non-segmental vitiligo.5
The efficacy of EL has been compared to the 308-nm excimer lamp and 311-nm NB-UVB in two meta-analyses.5, 6 Based on three randomized controlled trials (RCTs),7-9 a meta-analysis found no difference between EL and excimer lamp in achieving ≥ 50% and ≥ 75% repigmentation. Similarly, no difference was found in patients achieving ≥ 75% and 100% repigmentation between EL and NB-UVB in a meta-analysis based on four RCTs.10-13 Nevertheless, EL was more effective than NB-UVB when assessing ≥ 50% repigmentation as an outcome. Another study assessed non-segmental vitiligo patients treated with either EL or NB-UVB after punch grafting and showed no significant difference in repigmentation.10
A recently developed 311-nm titanium sapphire laser was shown not to be inferior to EL treatment in a randomized non-inferiority study with 74 paired lesions in 21 patients.14 Another meta-analysis13 assessed the benefit of adding topical therapy to EL and showed superior repigmentation for combination therapy with calcineurin inhibitors,15-18 however, insufficient evidence was found for combination therapy with topical vitamin D319-21 analogues and corticosteroids.22 Furthermore, the efficacy of EL with topical tacrolimus was assessed in the meta-analysis of Chang.23 Three RCT’s15, 16, 18 showed better improvements for ≥75% repigmentation when EL was combined with topical tacrolimus compared to EL alone. This was in line with the Cochrane review on vitiligo about combining NB-UVB phototherapy with topical interventions.24 Moreover, a RCT with 233 paediatric vitiligo patients showed better results after twelve weeks of treatment with EL combination therapy (tacrolimus, pimecrolimus or halometasone) compared to EL monotherapy.25 Wu et al compared EL monotherapy to tacrolimus 0.1% topical monotherapy and found no difference in ≥ 50% repigmentation after 6 months.26
There is insufficient evidence about the optimal regimen of EL therapy. One randomized, non-inferiority study showed a cyclic schedule (two months, twice weekly, one-month interval) to be equally effective compared to a continuous schedule of EL twice per week.27 This cyclic schedule may favour compliance and limits UV exposure. Moreover, no significant differences were found between one, two or three sessions per week.28, 29 However, repigmentation was faster with three sessions per week.28 According to the relationship between repigmentation and the total number of treatments, a minimum of 20 treatments is recommended.17 Inferior repigmentation was related to a longer disease duration, the presence of poliosis, location of lesions on hands and feet and a plurisegmental pattern. Facial lesions and younger patients were related to better outcomes.30-32
Multiple studies have proven the efficacy and safety of both EL and excimer lamps (together excimer therapy) in localized, non-segmental vitiligo.7-9 The repigmentation rate and side-effect profile are comparable to NB-UVB phototherapy, which should be reserved for patients with more than 5-10% BSA.3, 5, 6 The excimer lamp provides the same efficacy and is more cost-effective. Disadvantages of EL are the high costs for acquisition and maintenance, limited availability, and the laborious nature of procedures. Advantages of EL include the lower total cumulative UV dose compared to NB-UVB, lack of exposure of unaffected skin and high efficacy especially when combined with calcineurin inhibitors.10, 15-18
The efficacy of the excimer laser as adjuvant therapy following graft transplantation was assessed in two controlled trials. Firstly a comparative trial with 14 stable NSV patients treated with punch grafts showed no difference in repigmentation rate after adjuvant therapy with either EL or NB-UVB.10 Ebadi et al.33 showed in a non-randomized clinical trial with 10 stable NSV patients a difference between melanocyte–keratinocyte transplantation (MKT) and excimer laser combination therapy compared to excimer laser or MKT alone.
In summary, the combination of excimer therapy with topical immunosuppressive treatment is recommended in localized, non-segmental and segmental vitiligo. The safety of this therapy has been demonstrated recently in a large cohort of 25 694 vitiligo patients.34 However, in active vitiligo with BSA > 10%, the combination of oral mini-pulse therapy and NB-UVB was favored.35
Lasers used for melanocyte transplantation
There are multiple methods used for recipient site preparation in MKT such as liquid nitrogen, dermabrasion, psoralen ultraviolet A, suction blistering and lasers.36 Recipient site preparation is essential as it affects the adherence of the melanocyte graft, nutritional support for the graft, final repigmentation rate, aesthetic outcome and associated complications of the transplantation. Lasers, as opposed to other methods of recipient-site preparation, can be used on larger surface areas, delicate areas and cosmetically compromised areas such as the mouth, nose and eyelids without harming surrounding skin.37 Moreover, laser treatments can be standardized yielding highly reproducible effects, especially when using scanner devices. However, lasers are generally expensive, may increase the risk of dyspigmentation, and have attendant risk of scarring.38 Lasers, when appropriately handled, can offer control of depth and symmetry of the extirpated sites.
Short-pulsed carbon dioxide (CO2) laser for recipient preparation
The short-pulsed CO2 laser emits short bursts of high-energy 10 600-nm radiation, producing fast tissue ablation with minimal bleeding. Moreover, it induces less thermal damage to the surrounding tissues compared to the older, conventional continuous wave CO2 laser, that has a higher risk of scarring.39, 40 Modification with integrated scanner device provides more precise and uniform de-epithelialization with greater user reproducibility.41 Treatment with such a short-pulsed CO2 laser and scanner to the preparation site produced > 80% repigmentation in several MKT studies.40, 42, 43 An open, split-comparison study in stable vitiligo compared repigmentation results of mechanical dermabrasion to short-pulsed CO2 laser (82% density, 209-µm depth) for recipient site preparation. Overall, the dermabrasion seemed to have better repigmentation, although one patient developed hypertrophic scarring and atrophy at the dermabrasion site.38
Erbium YAG (Er:YAG) laser for recipient preparation
The Erbium-doped Yttrium Aluminium Garnet (Er:YAG) laser emits 2940-nm radiation which is absorbed by water approximately 10 times more than the CO2 radiation, reducing thermal damage and risk of scarring.36, 44 Gupta et al45 evaluated the use of Er:YAG laser vs. motorized dermabrader in recipient site preparation in a RCT with 32 patients. No difference in repigmentation or adverse events were seen.
Lagrange et al. compared microneedling to Er:YAG laser in a RCT with 6 patients.46 Three patients showed > 75% repigmentation, while none achieved any repigmentation with microneedling46, 47
Finally, a long-term retrospective study with 714 patients reported that motorized dermabrasion had a lower recurrence rate than Er:YAG laser.48 Limitations including laser user variability and the retrospective nature of the study may not allow to elucidate broader, more generalizable outcomes.
Fractional CO2 laser for recipient preparation
A RCT compared full surface superficial ablation (144 µm), deeper ablation (209 µm) and fractional ablation (225 µm) to negative control as a pretreatment for cell suspension transplantation.47 More than 75% repigmentation was found in 40%, 50% and 0% of the superficial, deeper, and fractional ablation respectively. The authors concluded that superficial full surface ablation is effective while fractional ablation is not effective for recipient site preparation.
In summary, ablative lasers appear to provide fast and uniform denudation of the epidermis with propitious repigmentation outcomes for recipient site preparation. Only pulsed lasers should be used for recipient site preparation because of the risk of scarring with continuous wave lasers. Conventional, full surface ablation is more effective than the fractional ablation or microneedling. Generally, Er:YAG lasers are regarded to induce less thermal damage, scarring and dyspigmentation than CO2 lasers. Moreover Er:YAG lasers offer a better assessment of the depth of the dermabrasion. Each choice of laser has benefits and risks associated and should be individualized to the patient and resources available at the time of transplantation.
Fractional laser for enhancing UV-induced repigmentation
Conventional ablative lasers, such as the CO2 laser and Er:YAG laser, have been reported to enhance repigmentation when combined with NB-UVB.49 However, these lasers have significant downtime and risk of scarring.
More recently, fractional ablative lasers offer less side-effects and have been reported to be effective when combined with NB-UVB.50
Unlike conventional ablative lasers, fractional lasers treat only a ‘fraction’ of the affected skin by creating microscopic thermal zones (MTZ) leaving intervening areas of skin untreated and results in rapid re-epithelization of the skin.51, 52 These ‘micro-wounds’ induce pro-inflammatory cytokines and growth factors, which not only promote rejuvenation and regeneration but also proliferation and migration of melanocytes.52-54 Fractional CO2 lasers also produce immediate tissue contraction and thereby temporarily reduce the vitiligo lesion size.55
In 2020, two systematic reviews with meta-analyses were published evaluating the safety and efficacy of fractional CO2 laser as an add-on therapy for NB-UVB.56, 57 Firstly, Kim et al. conducted a meta-analysis with 3 RCTs, comparing NB-UVB monotherapy and CO2 laser combined with NB-UVB therapy, excluding any other treatment methods.58-60 They demonstrated a higher repigmentation rate from combination therapy compared to NB-UVB alone. In contrast, Chang et al. published a meta-analysis involving 6 RCTs53, 58-62 showing a non-significant trend in favour of the CO2 laser and NB-UVB combination therapy. However, additional treatments (i.e. surgery, hair transplantation, topical agents) were included. Moreover, some of the contradictory results may be explained by the various degrees of disease stability in different studies.
King et al.63 demonstrated NB-UVB treatment for vitiligo was more effective when combined with ablation therapy in a systematic review and meta-analysis. However, these results can be interpreted in an ambiguous manner, as conventional ablative and fractional ablative lasers were pooled in the same meta-analysis while they are fundamentally different modalities.51, 52
In summary, based on the available literature, fractional ablative lasers are a safe option to improve the outcomes of NB-UVB. No severe side-effects from fractional therapy were reported and the Koebner phenomenon was not observed. A young age (< 14 years), short disease duration (< 1 year), stable disease and vitiligo on head and neck resulted in significantly better repigmentation.64, 65 However, the treatment is uncomfortable, time consuming and only feasible for relatively small areas (< 3% BSA) (Table 1).
| First Author, Year, ref | Laser type, wavelength | (sub)type vitiligo | Study design | Number of patients/ patches | Monotherapy/ combination therapy | Treatment compared to | Outcomes, results |
|---|---|---|---|---|---|---|---|
| Baltás, 20023 | Excimer laser 308 nm | Segmental, focal | Case series | 6 patients | Monotherapy | – | Percentage achieving ≥75% repigmentation 50% |
|
Sun, 20155 Lopes, 20166 |
Excimer laser 308 nm | NSV | Systematic review | 390 patients/764 patches | Monotherapy |
Percentage achieving ≥75% repigmentation EL 54.35% vs. NB-UVB 51.51% EL 34.87% vs. excimer lamp 33.33% |
|
| Bae, 201914 | Excimer laser 308-nm | NSV | Non-inferiority RCT | 21 patients/ 74 paired patches | Monotherapy | 311-nm Titanium:Sapphire laser (TSL) |
Mean repigmentation EL 55.4% TSL 58.2% |
|
Bae, 201630 Chang, 202123 |
Excimer laser 308 nm | NSV | Systematic review | 128 patients + 231 patches | Monotherapy | 308-nm excimer laser + topical calcineurin inhibitors15-18/vitamin D3 analogues19-21/Topical corticosteroids22 |
Percentage achieving ≥75% repigmentation EL 23.8% vs. EL + calcineurin inhibitors 46.2%* EL 2.9% vs. EL + vitamin D3 analogues 13.2%* EL 16.7% vs. EL + corticosteroids 42.9* |
| Li, 201925 | Excimer laser 308 nm | NSV | RCT | 233 paediatric patients | Monotherapy | 308-nm excimer laser + tacrolimus/ pimecrolimus/ halometasone |
Mean repigmentation EL monotherapy 57.7% EL + tacrolimus 76.6%* EL + pimecrolimus 72.9%* EL + halometasone 84.1%* |
| Wu, 201926 | Excimer laser 308 nm | NSV | RCT | 138 patients | Monotherapy | 0.1% tacrolimus ointment (+ betamethasone i.m. for active vitiligo) |
Percentage achieving ≥50% repigmentation Stable vitiligo EL 47.5% vs. 0.1% tacrolimus 35% Active vitiligo EL 80.7%* vs. 0.1% tacrolimus 50% |
| Sung, 201827 | Excimer laser 308 nm | NSV | Non-inferiority RCT | 12 patients/16 paired patches | Combination therapy + 0.1% tacrolimus ointment | Continuous vs. Cyclic on-off |
Mean repigmentation Continuous EL 51.4% Cyclic on-off EL 49.2% |
| Hofer, 200528 | Excimer laser 308 nm | NSV | Prospective study | 13 patients |
Monotherapy 1, 2 and 3 sessions per week |
– |
Repigmentation 1 session per week 60% 2 sessions per week 79% 3 sessions per week 82% |
| Shen, 200729 | Excimer laser 308 nm | NSV | Prospective study | 187 patients |
Monotherapy 20 sessions 0.5, 1, 2 and 3 sessions per week |
– |
Percentage achieving ≥75% repigmentation 0.5 session per week 0% 1 session per week 25% 2 sessions per week 26% 3 sessions per week 32% |
| Fa, 201731 | Excimer laser 308 nm | NSV | Prospective study | 979 patients | Monotherapy | – |
Repigmentation Mean 29.77% |
| Ebadi, 201533 | Excimer laser 308 nm | NSV | RCT | 39 patches | Monotherapy | MKT / MKT + excimer laser/no treatment |
Depigmentation reduction No treatment 0% EL + MKT 43.9%* |
| Silpa-Archa 201638 |
FCO2 laser 10 600 nm |
NSV, local | Open label split comparison study | 6 patients | Combination therapy + MKT | Dermabrasion + MKT |
Reduction of VASI Dermabrasion VASI 84% FCO2 VASI 73.5% |
| Oh, 200140 |
Ultrapulsed CO2 laser 10 600 nm |
NSV, local, focal | Case series | 11 patients / 34 patches | Combination therapy + MKT + topical or general PUVA | – |
Repigmentation Good (51–75%) 4 patches / excellent (76–100%) 30 patches |
| Hasegawa 200742 |
Short-pulsed CO2 laser 10 600 nm |
Segmental | Case series | 15 patients | Combination therapy + MKT | – |
Repigmentation Mean 100% |
| Sun, 201243 |
Ultrapulsed CO2 laser 10 600 nm |
NSV, segmental | Case series | 8 patients | Combination therapy + MKT | – |
Repigmentation Mean 84.4% |
| Kaufmann 199844 |
Erbium-YAG laser 2940 nm |
NSV | Case series | 3 patients / 9 patches | Combination therapy + MKT + UVA | – |
Repigmentation 22% ‘good’ growth |
| Gupta, 201845 | Er:YAG laser 2940 nm | NSV, focal, segmental | RCT | 32 patients | Combination therapy + MKT | Mechanical dermabrasion + MKT |
Total repigmentation Er:YAG + MKT 54.7% Dermabrasion + MKT 48.8% |
| Lagrange 201946 | Er:YAG laser 2940 nm | Local, segmental | RCT | 6 patients | Combination therapy + MKT | Microneedling + MKT |
Percentage achieving ≥75% repigmentation Er:YAG + MKT 16.7% Microneedling + MKT 0% |
| Lommerts 201747 |
Ablative CO2 laser 10 600 nm |
Segmental | RCT | 10 patients (3 vitiligo) | Combination therapy + MKT | 209- μm and 144-μm full surface ablation + MKT/No treatment |
Median repigmentation Fractional ablation 0% 209-μm full surface ablation 68.7%* 144-μm full surface ablation 58.3%* |
| Bayoumi 201249 |
Er:YAG laser 2940 nm |
NSV | RCT | 24 paired lesions | Combination therapy + hydrocortisone 17-butyrate cream + NB-UVB | Hydrocortisone 17-butyrate cream + NB-UVB |
Percentage achieving ≥50% repigmentation Dermabrasion + hydrocortisone 17-butyrate cream + NB-UVB: 45.9%* Hydrocortisone 17-butyrate cream + NB-UVB 8.4% |
| Kim, 202056 |
FCO2 laser 10 600 nm |
NSV | SR | 123 cases58-60 | Combination therapy + NB-UVB | NB-UVB |
Percentage achieving ≥75% repigmentation FCO2 + NB-UVB 8.1%* vs. NB-UVB 0.8% |
| Chang, 202057 |
FCO2 laser 10 600 nm |
NSV | SR | 140 patients53, 58-62 | Combination therapy + NB-UVB | NB-UVB |
Percentage achieving ≥75% repigmentation FCO2 + NB-UVB 10.6%* vs. NB-UVB 4.8% |
| Huang 201965 | Er:YAG laser 2940 nm | NSV | Retrospective study | 684 patients / 1,026 lesions | Combination therapy + laser-assisted delivery of topical compound betamethasone solution | – |
Repigmentation Mean 40.3% |
| Kim, 200171 | QS ruby laser 694 nm | Vitiligo universalis | Case report | 1 patient | Combination therapy + Neo-adjuvant PUVA | – | Relapse after complete depigmentation: no relapse after one year |
| Rao, 200472 | QS alexandrite laser 755 nm | Vitiligo universalis | Case report | 1 patient | Monotherapy | – | Relapse after complete depigmentation: minimal recurrence of pigment |
| Majid, 201373 | Frequency-doubled QS Nd:YAG laser 532 nm | Vitiligo universalis | Prospective open-label study | 15 patients / 26 patches | Combination therapy + Topical MBEH |
Percentage achieving ≥90% depigmentation 87.7% of patients |
|
| El-Mofty 201975 | (Frequency-doubled) QS Nd:YAG laser 1s064/532 nm | Vitiligo universalis | Comparative study | 40 patients | Monotherapy |
Facial: TCA peels 25% and 50% Non-facial: cryotherapy, phenol 88% |
Excellent/complete depigmentation Facial QSL 90%* vs. TCA peel 25 35% vs. TCA peel 50 60% Non-facial QSL 95% vs. cryotherapy 90% vs. phenol 100% |
| Majid, 201776 | Frequency-doubled QS Nd:YAG laser 532 nm | Vitiligo universalis | Retrospective study | 28 patients | Monotherapy | – | Relapse after complete depigmentation: 25% of patients partial to complete relapse |
| Thissen 199777 | QS ruby laser 694 nm | Vitiligo universalis | Open non-comparative clinical trial | 8 patients | Monotherapy | – | Complete depigmentation in 37.5% of patients |
| Komen 201378 | QS ruby laser 694 nm | Vitiligo universalis | Retrospective study | 27 patients | Monotherapy | – | Percentage achieving ≥75% depigmentation 48% of patients |
| Njoo, 200079 | QS ruby laser 694 nm | Vitiligo universalis | Retrospective study | 13 patients | Combination therapy + topical 4-methoxyphenol | – |
Complete depigmentation in 69.2% of patients Recurrence of pigmentation in 44.4% of patients |
| Van Geel 201580 | QS alexandrite laser 755 nm | Vitiligo universalis | Retrospective comparative study | 22 patients / 51 patches | Monotherapy | Cryotherapy |
Mean depigmentation after one session Cryotherapy 46.7% QS alexandrite 42.9% |
| Boukari 201481 | QS ruby laser 694 nm / QS alexandrite 755 nm / QS Nd:Yag 532 nm | Vitiligo universalis | Retrospective case series | 6 patients / 16 patches | Monotherapy | – |
Relapse after complete depigmentation 33% of patients/patches no relapse |
- ≥ 75% of repigmentation was chosen to be presented in Table 1 when different repigmentation thresholds were reported.
- * P < 0.05.
Lasers for depigmentation therapy in vitiligo
If depigmentation is non-responsive to treatment and extensive to nearly complete (vitiligo universalis), patients may wish to depigment the residual pigmented skin and thereby improve quality of life.66 Topical bleaching treatments with monobenzyl ether of hydroquinone (MBEH),67, 68 phenol peels,4 cryotherapy69, 70 and lasers are all used as depigmenting treatment. Topical bleaching treatments are associated with limitations such as skin irritation, limited availability and incomplete and slow clinical response to achieve depigmentation.67, 68 In comparison, lasers are relatively safer and more rapidly acting.71, 72
In general, Q-switched (QS) nanosecond lasers with various wavelengths (532, 694, 755 nm) have been used for depigmentation therapy. For picosecond lasers, evidence on efficacy for depigmentation is lacking so far. QS nanosecond lasers emit radiation with a high absorption by melanin and a very short pulse duration within the nanosecond range to match the thermal relaxation time of melanosomes. This results in a photomechanical laser tissue interaction leading to selective melanocyte damage.66, 73, 74
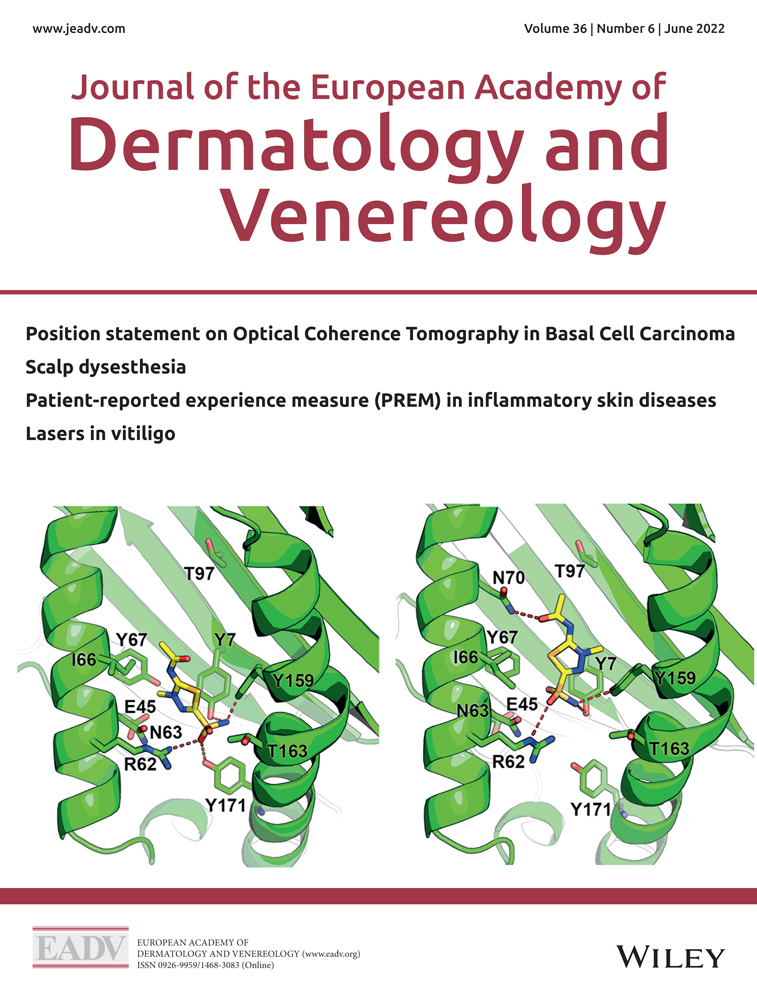
Frequency-doubled QS neodymium-doped yttrium aluminium garnet (QS Nd:YAG) laser
Majid et al.73 investigated the efficacy of the 532 nm QS Nd:YAG laser in a prospective open label study. Fifteen patients with > 80% depigmentation were treated 1–3 times. Thirteen of the 15 patients achieved ≥ 90% depigmentation and only one patient reported recurrence at 3 months follow-up. Moreover, a RCT with 40 patients showed better outcomes for the face in patients with active vitiligo for the QS Nd:YAG laser as compared to TCA peeling.75 Long-term depigmentation after QS Nd:YAG laser was evaluated in a retrospective study with 28 patients. After a follow-up period of 2–5 years, 85% of the patients were highly satisfied and 89.3% maintained depigmentation of > 90%.76
QS ruby laser (QSRL)
Thissen et al.77 achieved complete depigmentation in all 8 patients after 1 session using the QSRL. However, 5 patients developed follicular repigmentation during the 9-month follow-up. The other 3, all with initially positive Koebner phenomenon, remained depigmented on the treated areas. A retrospective study with 27 patients also evaluated the long-term efficacy of the QSRL after complete depigmentation was achieved. While only half of the patients showed > 75% depigmentation after a mean follow-up of 13 months, many patients (85%) were satisfied with the treatment.78 Similar to other studies, active disease was related to better outcomes. Another retrospective study in nine QSRL-treated patients observed recurrence in almost half of the patients after 2–18 months.79
QS alexandrite laser (QSAL)
Van Geel et al.80 compared cryotherapy with the 755-nm alexandrite laser in 22 patients and found no significant difference in the capacity to induce depigmentation (46.7% vs. 42.9%). However, side-effects were restricted to the group receiving cryotherapy.
Moreover a retrospective study with six patients with 16 normally pigmented skin areas with a BSA of 5-15% were treated with either 694 nm QS ruby laser, or 755 nm QS Alexandrite or 532 nm QS Nd:Yag laser until complete depigmentation with a median of two sessions. Two third of the patients had a relapse after a median follow-up of 36 months.81
In summary, laser-induced depigmentation therapy has proven to be a safe treatment with a high patient satisfaction.76, 77, 80 Short-term side-effects are common and include: purpura, crusts and oozing of the skin, but no long-term side-effects or scarring have been reported. Moreover, an advantage of laser therapy is that its effects are limited to the treatment site, while topical MBEH induces depigmentation in remote sites.68 However, laser depigmentation is a painful treatment, for which topical anaesthesia is often necessary. The therapy is also time consuming, limiting the treatment area.74 Long-term outcomes are highly variable and difficult to predict, besides in most cases maintenance sessions at least once a year are required. Active vitiligo and the presence of the Koebner phenomenon seem to be related to better depigmentation results.71, 80 For these reasons, it is recommended to perform test spots prior to treatment. While there are no head-to-head comparisons between these QS laser devices, it is likely that the efficacy is more related to the activity of vitiligo than the type of laser device.
Summary
Lasers are an effective therapeutic option with a diversity of indications in vitiligo. These indications comprise repigmentation monotherapy, combination with NB-UVB, recipient site preparation before grafting and depigmentation. The laser devices that have been used are as diverse as the indications. When aiming for repigmentation, monotherapy with a 308 nm excimer or a 311 nm titanium sapphire laser is effective. The combination of the excimer laser with topical calcineurin inhibitors provides higher repigmentation rates. A minimum of 20 excimer laser sessions two or three times per week is recommended. Lasers for recipient site preparation can be used on large, delicate and cosmetically compromised areas in order to achieve reproducible ablation without harming surrounding skin. Short-pulsed CO2 laser or Erb:YAG lasers should preferably be used, of which the Erb:YAG laser gives less thermal damage and a reduced risk of scarring. Fractional lasers improve the outcomes of repigmentation as an add-on therapy for NB-UVB. In universal vitiligo, Q-switched lasers are safe, rapidly acting and induce depigmentation in most of the patients although maintenance sessions are usually necessary.
The outcomes of laser treatment depend on many variables. High repigmentation rates after excimer laser treatment are more likely at a young age, with short disease duration and facial localization. However, high depigmentation rates with QS lasers are best achieved when vitiligo is active with the presence of the Koebner phenomenon. Overall, patients are highly satisfied with the results and severe side-effects are very uncommon. Laser treatments can be standardized, yielding highly reproducible effects. Nonetheless all laser treatments are relatively expensive, not available in every hospital, not home based and only suited for small areas. Each type of laser has benefits and risks associated and should, therefore, be individually chosen based on location, extent, activity and type of vitiligo.
Open Research
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.