European S1 guideline for the treatment of hidradenitis suppurativa/acne inversa
Conflicts of interest:
None declared.
Funding source:
None declared.
Abstract
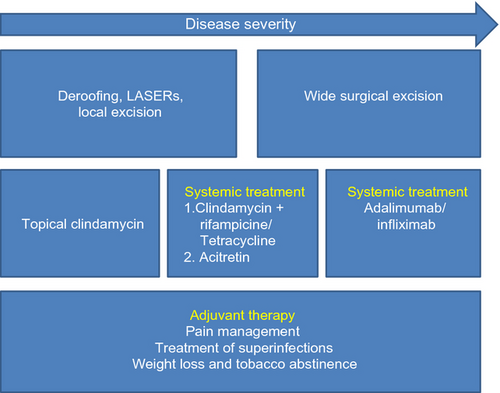
Hidradenitis suppurativa/acne inversa (HS) is a chronic, inflammatory, recurrent, debilitating skin disease of the hair follicle that usually presents after puberty with painful, deep-seated, inflamed lesions in the apocrine gland-bearing areas of the body, most commonly the axillae, inguinal and anogenital regions. A mean disease incidence of 6.0 per 100 000 person-years and an average prevalence of 1% has been reported in Europe. HS has the highest impact on patients' quality of life among all assessed dermatological diseases. HS is associated with a variety of concomitant and secondary diseases, such as obesity, metabolic syndrome, inflammatory bowel disease, e.g. Crohn's disease, spondyloarthropathy, follicular occlusion syndrome and other hyperergic diseases. The central pathogenic event in HS is believed to be the occlusion of the upper part of the hair follicle leading to a perifollicular lympho-histiocytic inflammation. A highly significant association between the prevalence of HS and current smoking (Odds ratio 12.55) and overweight (Odds ratio 1.1 for each body mass index unit) has been documented. The European S1 HS guideline suggests that the disease should be treated based on its individual subjective impact and objective severity. Locally recurring lesions can be treated by classical surgery or LASER techniques, whereas medical treatment either as monotherapy or in combination with radical surgery is more appropriate for widely spread lesions. Medical therapy may include antibiotics (clindamycin plus rifampicine, tetracyclines), acitretin and biologics (adalimumab, infliximab). A Hurley severity grade-relevant treatment of HS is recommended by the expert group following a treatment algorithm. Adjuvant measurements, such as pain management, treatment of superinfections, weight loss and tobacco abstinence have to be considered.
Definition
Hidradenitis suppurativa/acne inversa (HS) is a chronic, inflammatory, recurrent, debilitating skin disease of the hair follicle that usually presents after puberty with painful, deep-seated, inflamed lesions in the apocrine gland-bearing areas of the body, most commonly the axillae, inguinal and anogenital regions (Dessau definition, 1st International Conference on Hidradenitis suppurativa/Acne inversa, March 30–April 1, 2006, Dessau, Germany).1, 2
Clinical presentation
Recurrent inflammation occurring more than 2×/6 months or 3×/6 months in the inverse regions of the body, presenting with nodules, sinus-tracts and/or scarring.3
Diagnosis
Primary positive diagnostic criteria
History: Recurrent painful or suppurating lesions more than 2×/6 months.
Signs: Involvement of axilla, genitofemoral area, perineum, gluteal area and infra-mammary area of women. Presence of nodules (inflamed or noninflamed). sinus tracts (inflamed or noninflamed), abscesses, scarring (atrophic, mesh-like, red, hypertrophic or linear).
Secondary positive diagnostic criteria
History: Family history of HS.
Microbiology: A negative swab or the presence of normal skin microbiota may be indicative of HS.
Differential diagnosis
- Staphylococcal infection (lesions are spread in a random fashion and more pustular)
- Cutaneous Crohn's disease (associated intestinal Crohn's disease)
- Simple abscesses (usually single lesions)
- Neoplasms, primary or secondary (systemic and histological signs of tumour)
- Lymphogranuloma venereum
- Rare:
- ○ Cutaneous actinomycosis (presents with sinus tract disease)
- ○ Scrofuloderma type of cutaneous tuberculosis
Classification and severity assessment
Hurley staging
In 1989, a severity classification was first proposed by Hurley.4
- Stage I: Abscess formation, single or multiple, without sinus tracts and cicatrization.
- Stage II: Recurrent abscesses with tract formation and cicatrization, single or multiple, widely separated lesions.
- Stage III: Diffuse or near-diffuse involvement, or multiple interconnected tracts and abscesses across the entire area.
Stage I disease is most common (68% of patients), while stage II occurs in 28% of patients, and 4% of HS patients have stage III.5 Today, the Hurley classification is still useful for the determination of three severity groups but it has limitations. The Hurley classification is not quantitative, consisting of only three stages and based on static disease characteristics such as scarring and fistulas. Hence, it is not suitable for monitoring the efficacy of interventions in clinical trials.
Sartorius score
A more detailed and dynamic HS severity score was created by Sartorius et al.6, 7 and was later modified. The main parameter in the modified Sartorius score is the counting of individual nodules and fistulas. The modified Sartorius score was the first disease specific instrument for dynamically measuring clinical severity. However, it has been argued that its applicability is limited in severe cases in which separate lesions become confluent. Even if this score is more dynamic than the Hurley score it still includes lesions, which may not be sensitive to medical treatment (scars; distance between two relevant lesions).
Physician global assessment
Currently, a Physician Global Assessment (PGA)8 is the most frequently used assessment tool to measure clinical improvement in clinical trials of medical treatments. A recently developed six stage PGA was defined as follows.8
- Clear: no inflammatory or noninflammatory nodules
- Minimal: Only the presence of noninflammatory nodules
- Mild: Less than five inflammatory nodules or one abscess or draining fistula and no inflammatory nodules
- Moderate: Less than five inflammatory nodules or one abscess or draining fistula and one or more inflammatory nodules or 2–5 abscesses or draining fistulas and less than 10 inflammatory nodules
- Severe: 2–5 abscesses or draining fistulas and ten or more inflammatory nodules
- Very severe: More than five abscesses or draining fistulas
Other scores
Kerdel et al. created another HS specific severity score: the Hidradenitis Suppurativa Severity Index (HSSI).9 This score has been used in two publications studying the clinical efficacy of infliximab.9, 10 This score incorporated categorical objective parameters with categorical subjective parameters.
Epidemiology
Prevalence and incidence
Several studies aimed to assess frequency of HS using prevalence or incidence estimations in different settings (hospital vs. population-based), different time periods (from 1968 to 2008) different diagnosis methods (self-reported, medically assessed, diagnosis of treatments codes through automated requests in medical information systems) leading to an important variability in estimations and uncertainties regarding the actual frequency of HS.11, 12
One recent study estimated the incidence of HS12 in an American county (Minnesota) with a population of about 144 000 people. The source was the Rochester Epidemiologic Project, a medical information system gathering records from hospitals, clinics, private practitioners and nursing homes within the county. Between 1968 and 2008, 268 HS cases were identified leading to a mean incidence of 6.0 per 100 000 person-years with a twofold incidence between the extremities of the period (4 to 10 per 100 000 person-years). This increase may be due to an increase in detection and coding of HS in the medical information system. The strength of this study was to estimate the incidence of HS for the first time. The limit of the study was its retrospective design. Moreover, there may be a selection bias due to recruitment through medical information system leading to a possible underestimation of incidence. There also may be a classification bias due to missed diagnosis of mild early cases.
By postulating a duration of active HS being a maximum of about 20 years for a given subject, the incidence can be extrapolated to prevalence = incidence × duration of the disease. Accordingly, the prevalence would be:
- Max: 10/100 000 years × 20 years = 200/100 000 = 0.20%.
- Min: 4/100 000 years × 20 years = 80/100 000 = 0.08%.
This conclusion is supported by expert opinion.
A recent American prevalence study13 based on a health claims database estimated HS prevalence to be 0.05%. As reported by the authors, there may be a selection bias due to the setting including only health-insured subjects and therefore the results might not be representative for the general population. There also may be a classification bias as HS cases were identified only through drug reimbursement, leading to potential underestimations. Moreover, the mean age of cases was 38 years, i.e. older than the mean age of HS patients in European studies. Hence, young patients who have not yet sought medical advice may have been missed. Patients with no medical insurance may also be overlooked in this study.
These two estimations are much lower than two others from Europe11, 14 which both reported a prevalence of 1%. One study11 was a population-based study on a representative sample of the French population (10 000). HS cases were self-declared. To our knowledge, it is the only population-based study with a study sample representing the French population. Even though selection bias is unlikely in this setting, a classification bias is likely due to self-declaration leading to potential over-estimation of the prevalence rate. However, Jemec et al.14 medically assessed a sample of 599 Danish unselected subjects and found a prevalence of 1% (0.4–2.2). In another study,15 Jemec found a prevalence of 4% in young adult women. As HS is mainly a disease of young adults with a female predominance this result is not discordant with the figure of 1% in the general population.
The discrepancies between European and American studies may be due to different methodologies but may also reflect actual differences in prevalence/incidence of HS or different diagnostic criteria. Only the most severe cases having been reported in the USA.
Psychosocial impact
The skin is a very important organ for our proper psychosocial functioning, as it is the largest and most visible part of the body. It plays a crucial role in interpersonal relationships, self-esteem, and perception of self-image and public image. Undoubtedly, HS due to its character has a huge impact on patients' quality of life (QoL). Therefore, many HS sufferers have to deal with depression and embarrassment. In addition, fever and fatigue often arise in extreme cases and may prevent individuals from performing even common everyday-tasks.
Pain
One of the most important problems reported by HS patients is pain, usually linked to the deep seated inflammatory nodules. Patients describe it in many ways, e.g. as hot, burning, pressing, stretching, cutting, sharp, taut, splitting, gnawing, sore, throbbing or aching. HS patients rated their pain using a Visual Analog Scale (VAS) as 4.5 ± 2.4 points (range, 0–10 points) or by means of a Numeric Rating Scale-11 (NRS) as 3.6 ± 3.2. Moreover, when compared to other dermatological conditions, which served as a control, the difference of pain intensity was of significant importance (P < 0.001).16-18
Dermatology Life Quality Index
The influence of HS on patients' QoL was quite often evaluated with a population-specific questionnaire - Dermatology Life Quality Index (DLQI). Even though the data is still limited, the observations are consistent and convergent (Table 1).
| von der Werth and Jemec22 | Onderdijk et al.16 | Matusiak et al.21 | |||||
|---|---|---|---|---|---|---|---|
| DLQI total | 8.9 ± 8.3 | 8.4 ± 7.5 | 12.67 ± 7.7 | ||||
| Median (min-max) | Median | 7 (0–29) | 6 (N/A) | 12 (1–30) | |||
| DLQI domains | |||||||
| Symptoms and feelings | 2.72 | 2.42 ± 1.87 | 3.06 ± 1.5 | ||||
| Daily activities | 1.95 | 1.82 ± 1.76 | 2.62 ± 1.81 | ||||
| Leisure | 1.57 | 1.47 ± 1.89 | 2.37 ± 1.77 | ||||
| Work or school | 0.82 | 0.67 ± 0.98 | 1.25 ± 1.31 | ||||
| Personal relationships' | 1.55 | 1.62 ± 1.94 | 2.42 ± 2.17 | ||||
| Treatment | 0.64 | 0.35 ± 0.74 | 0.96 ± 0.97 | ||||
All of the DLQI subdomains were ‘hardly’ affected, but the greatest impact was reported for ‘symptoms and feelings’ and ‘daily activities’. According to the Global Question (GQ) indexing,19 HS impact on QoL was estimated as having large or extremely large effect on patient's life for nearly 60% of examined patients.20 As found by Matusiak et al.21 the main predictors of QoL impairment were HS clinical stage assessed accordingly to Hurley classification (P < 0.0001), number of skin areas involved by HS lesions (R = 0.28; P = 0.045) and anogenital localization (P = 0.0051). Similar findings were revealed in a study by Onderdijk et al.,16 where patients with more severe disease (with reference to Hurley staging or number of flares during the last month) had markedly higher DLQI scores (P < 0.05).
As mentioned above, von der Werth and Jemec22 pointed out the significant reduction in quality of life (measured by the DLQI) of patients with HS. In the work of Sartorius et al.6 the link of the severity of HS with smoking and increased body mass index as evaluated by the reduction in quality of life measured by the DLQI was reported. The comprehensive overview of Alikhan et al.23 considered several psychosomatic aspects of HS. Reference is made to the limited quality of life by DLQI, the problems in the social environment, such as in the family, and even suicidal ideas, but also to economic difficulties such as loss of job. Another recent study also compared the reduced quality of life of the patients was addressed in concomitance with HS.21 The investigations of Esmann and Jemec3 have shown a significant pressure in HS patients at work, in partnership, in sexual life and quality of life. The DLQI results found for HS showed significantly greater QoL impairment than has been found in some other dermatoses (e.g. acne, psoriasis, atopic eczema, skin tumours, etc.).16, 21 It can be concluded that HS is a highly distressing disease for many patients, probably one of the worst that has been analysed and evaluated in dermatology to date.
Depression
According to the database study by Vazquez et al.,12 42.9% of HS sufferers were diagnosed with depression. However, two other studies did not reveal such a high prevalence of depression in HS patients.16, 21 In order to estimate the probability of depression and its intensity, the Beck Depression Inventory-Short Form (BDI-SF) and Major Depression Inventory (MDI) were used. According to these studies, the depression prevalence rate was with 21% half as high as diagnosed by Vazquez et al.12 (cut-offs: BDI≥10 and MDI≥20). The BDI-SF and MDI scores showed that every fifth patient is threatened with co-existence of depression, which makes HS a disease of high risk for development of this kind of reactive disorder, even higher than those found for other dermatoses or any other serious somatic conditions.16, 21 It was confirmed in a study by Onderdijk et al.16 where mean MDI scores were significantly higher for HS patients than dermatological controls (11.0 vs. 7.2; P < 0.0001). However, clinically defined depression rates according to the ICD-10 criteria did not reach statistical significance (P = 0.06) when compared to controls (9% vs. 6%).16
The results of the two later studies revealed that depression level measured by means of BDI-SF was significantly positively correlated with the HS clinical stage (P = 0.0015), anogenital localization (P = 0.017) and later age at disease onset (P = 0.03). MDI levels were significantly correlated with the number of sick-days due to the disease during the last 3 months, number of days with lesions during the past month, itching, pain number of flares during the last month and Hurley stage (P < 0.05).16, 21
Stigmatization
It was found that HS has a great emotional impact on patients and promotes isolation due to fear of stigmatization.3 The analysis of this problem was conducted in a study by Matusiak et al.,20 where Evers et al. ‘6-Item Scale’ was used for assessment of stigmatization level. As in the case of the preceding aspects of the QoL evaluation, the stigmatization level among HS patients was proportionately dependent on the clinical stage of the disease (P = 0.006). The location of the lesions was again an important factor in reducing patients' self-esteem, although with involvement of exposed skin areas being the major contributors (P = 0.031).
Sexual health
Investigating patients' sexual health Kurek et al. found that patients with HS have a significantly higher impairment of sexual health compared to age-, gender- and BMI-matched controls (P < 0.01).24 Sexual distress was particularly higher in female than in male patients with HS. Surprisingly, severity of cutaneous alterations measured by the Sartorius score correlated neither with sexual dysfunctions nor with sexual distress.
Summarizing, HS affects patients' lives in many ways. The sufferers underline the problems linked to interpersonal contacts, especially in relation to appearance and smell, various emotional reactions, as well as feelings of lack of control. HS has a great emotional influence on patients and promotes the social isolation. Irritation and shame are frequent and relate to smell, pain, scars and itching.3 Moreover, not surprisingly, such a chronic and debilitating skin disease has its reflection in socio-economic status tightly related to professional activity. The studies underline the significant work disability rate together with high unemployment rate among HS sufferers, while most of them are in a productive age.19, 25, 26
Comorbidity
Jansen et al.27 describe HS as a chronic inflammatory dermatosis, which is associated with a variety of concomitant and secondary diseases, such as obesity, systemic amyloidosis, arthropathy and squamous cell carcinoma.
According to the review by Lee et al.28 extensive HS is associated with a considerable burden of disease (such as pyoderma, arthritis, Crohn's disease, anaemia, lymphedema). In the systematic review of Fimmel and Zouboulis1 the follicular occlusion syndrome, inflammatory bowel disease, e.g. Crohn's disease, spondyloarthropathy and other hyperergic diseases are the most common comorbid diseases in HS (Table 2).
| Disease | Gene locus | Dysregulated gene | Protein | Cases in the literature associated with HS/AI |
|---|---|---|---|---|
|
(1) Crohn's disease, Colitis ulcerosa (2) Crohn's disease and squamous cell carcinoma |
16q12 | NOD2/CARD15 | Caspase recruitment domain-containing protein |
81 1 |
| SAPHO syndrome (Synovitis, Acne, palmoplantar Pustulosis, Hyperosteosis, Osteitis) | 9 | |||
| Pyoderma gangraenosum | 7 | |||
| Adamantiades-Behçet's disease | HLA-B51, IL-12B | IL-12 promoter | 5 | |
| Spondylarthropathy |
6p21.3 9q31-q34 |
HLA-B27 IL-1, IL-23, ERAP1, TNFSF15, HLA negative |
Endoplasmic reticulum Aminopeptidase Tumour necrosis factor family |
59 |
|
Genetic keratin defects associated with follicular occlusion (1) Pachyonychia congenita(2) Dowling-Degos disease |
17q12-q21 12q13 12q13 |
KRT 17 KRT6B KRT5 |
Cytokeratin 17 Cytokeratin 6B Cytokeratin 5 |
42 26 16 |
|
Other genetic diseases (1) Keratitis Ichthyosis Deafness (KID) syndrome (2) Down syndrome |
13q11-q12 1q43, Xp11.23, 21q22.3 |
GJB2 z. B. GATA1 |
GAP junction protein beta-2 = connexin-26 Globulin transcription factor 1 |
4 3 |
|
Tumours (1) Squamous cell carcinomaa (2) Adenokarcinomaa |
7p11.2 11q13.3 |
ECOP CCND1 |
EGFR Co-amplified and overexpressed protein cyclin D1 |
38 37 1 |
- a Squamous cell carcinoma and adenocarcinoma only occur at the genitoanal region in cases of long-term chronic inflammation and therefore cannot be considered as primary comorbid diseases.
Sabat et al. reported that HS patients have a significantly higher prevalence of the metabolic syndrome (P < 0.05, odds ratio (OR) 4.46) and almost all of its criteria, namely central obesity [OR 5.88], hypertriglyceridaemia (OR 2.24), hypo-HDL-cholesterolaemia (OR 4.56) and hyperglycaemia (OR 4.09)29 compared to healthy controls. Remarkably, the appearance of the metabolic syndrome affects a disproportionately high number of young HS patients (patients < 35 years, OR 6.18).
In an overview by Meixner et al.,30 the reduced mobility of HS patients caused by contractures after healing with scarring development of malignant tumours including cancer of the anogenital area, chronic lymphedema and anaemia are listed as the major comorbid diseases and complications of the disease.
Pathogenesis
Histology31
Biopsies are not routinely performed for diagnostic purposes. Histological examination of skin specimens demonstrates keratin plugging of follicles as an early feature with or without inflammation.32 Early inflammation of the apocrine gland and duct appears to be a rare primary event.33 Established lesions show follicular plugging, follicular cysts, reduced volume of sebaceous glands, psoriasiform hyperplasia, neutrophilic abscesses, sinus tracts lined by a stratified epithelium. In long-standing severe cases granuloma formation, B cells and plasma cells in ‘pseudo’ follicles, abscesses and sinuses surrounded by a chronic inflammatory infiltrate containing histiocytes and giant cells, granulation tissue and occasional foreign body reaction can be seen.34 Extensive fibrosis is frequently seen as a late result of this inflammation.
Cytokeratin 17 (found in normal infundibulum), has been shown to be absent from infundibular-like keratinized epithelium, suggesting fragility of the draining sinus epithelium, which may be responsible for rupture.35 The sebo-follicular junction was found to be almost devoid of PAS positive material in both the border and centre lesions; this may explain its apparent fragility.
Although inflammation does not appear to originate within the apocrine glands, the exclusive finding of the disease within apocrine-gland-bearing skin does not allow the concept of the apocrine gland being an innocent bystander and indicates an apocrine effect.36
Inflammation
So far only little data are available about the precise mechanism leading to tissue inflammation and damage in patients with hidradenitis suppurativa. The central pathogenic event in HS is believed to be the occlusion of the upper parts of the hair follicle leading to a perifollicular lympho-histiocytic inflammation.2, 37, 38 In early lesions, neutrophilic abscess formation and influx of mainly macrophages, monocytes and dendritic cells predominate. In chronic disease, the infiltrate expands with increased frequencies of B cells and plasma cells.39 In the inflammatory infiltrates toll like receptor 2 (TLR2) was highly expressed by infiltrating macrophages and dendritic cells indicating that stimulation of inflammatory cells by TLR2 activating microbial products may be important trigger factors in the chronic inflammatory process.40 Furthermore, the proinflammatory cytokines IL-12 and IL-23 are abundantly expressed by macrophages infiltrating papillary and reticular dermis of HS skin.41 Both of these cytokines are believed to be important mediators in autoimmune tissue destruction and its blocking by biologics has been shown to be effective in the treatment of psoriasis.42 Especially IL-23 has been shown to be involved in the induction of a T helper cell subset producing IL-17, therefore, named Th17, which is distinct from the classical Th1/Th2 subsets. In chronic HS lesions IL-17-producing T helper cells were found to infiltrate the dermis.43 An overexpression of various other cytokines like IL-1beta, CYCL9 (MIG), IL-10, IL-11 and BLC has been described in HS lesion whereas IL-20 and IL-22 have been shown to be down regulated.43, 44 Interestingly, a therapy with the TNF-alpha blocking agent adalimumab could suppress the expression of most of these upregulated cytokines.43 Similar as in lesions of psoriasis also in HS the antimicrobial peptides beta defensin 2, psoriasin and cathelicidin were highly upregulated.45 This may at least in part explain the clinical finding that HS patients suffer only rarely from skin infections. Taken together the inflammatory reaction leading to HS are only poorly understood, but they show many similarities with other inflammatory reactions as e.g. in psoriasis.
Genetic background
The etiology of HS involves genetic and environmental factors. A role of genetic factors was firstly suggested by Fitzsimmons and Guilbert in 1985. The authors described that 34.3% of first-degree relatives of HS patients also suffer from HS and that the condition appeared to be transmitted as an autosomal dominant trait.46 Similar data were provided by current studies, in which 30 to 40% of HS patients reported a family history of HS.47 Due to the efforts of the last 3 years we now know the genetic reasons for the disease in approximately 5% of the HS patients.46 They are different heterozygous mutations in subunits of the gamma-secretase. The first of them were found in six Chinese families.48 They were subsequently confirmed, and further mutations in gamma-secretase were found in British, Chinese, Japanese and French families.49 It is important to note that HS patients with gamma-secretase mutations have a severe, extensive disease phenotype. gamma-secretase is an intramembranous endoprotease complex composed of four hydrophobic proteins: presenilin, presenilin enhancer-2, nicastrin and anterior pharynx defective. The enzyme can cleave multiple type-1 transmembrane proteins including Notch receptors. Most mutations found so far in gamma-secretase affected nicastrin that is involved in the integration of the different subunits into the gamma-secretase complex and in complex stabilization. Importantly, at least the majority of gamma-secretase mutations in HS were loss-of-function mutations, leading to reduced protease activity and, among others, attenuated Notch signalling.50 Interestingly, mice with disrupted gamma-secretase activity or Notch signalling showed skin alterations similar to the alterations observed in HS patients, including follicular keratinization, follicular atrophy, the formation of epidermal cysts, and epidermal hyperplasia.49 As mentioned above, gamma-secretase mutations seem to be responsible for approximately 5% of HS cases, and we might anticipate important discoveries regarding genetic predispositions for HS in the future. These can involve new mutations and/or single nucleotide polymorphisms (SNPs). Furthermore, a certain haplotype of the TNF gene seems to be associated with a greater reduction in disease severity after treatment with TNF agents.48 Finally, genetic factors might influence not only the appearance of HS but also the phenotype of disease.
Bacteria
HS is not a «classic» infectious disease: there is no unique bacterial agent but a polymorphic flora; it is a chronic disease with or without acute flares. Bacterial sampling of suppurations are frequently negative i.e. sterile. Several members of the normal skin flora are found in the HS lesions.50, 51
The normal microflora of the skin includes coagulase negative staphylococci (CNS); some of them are mostly prevalent in areas of apocrine sweat glands: Staphylococcus hominis, Staphylococcus epidermidis and Staphylococcus haemolyticus are mainly found in axillary and genital areas. Micrococcus species, Micrococcus luteus, Micrococcus varians colonize axillae, perineum and groin. Various bacteria belonging to the genus Corynebacterium are associated, mainly Propionibacteria, gram-positive, anaerobic bacteria: Propionibacterium acnes, Propionibacterium granulosum, Propionibacterium avidum. Acinetobacter subspecies, the only important gram-negative residents are found in the axillae and groin. They are responsible for severe nosocomial infections in hospital setting but are rarely a cause of community infections.
Bacteria found in HS lesions are various; they have been considered either as contaminants of the normal skin flora or as the result of a secondary infection of an initially sterile process. Samples collected at the surface of lesions entail the risk of contamination by the resident or transitory (Staphylococcus aureus) flora. By aspirating pus from deep parts or by vaporization level by level with CO2 laser, two studies have circumvented the problem and have shown the predominance of CNS and of anaerobes of the commensal flora52; Streptococcus milleri, a member of the normal oral flora, which had previously been considered the first bacterium responsible for HS53 was seldom recovered. The Swedish team of Karin Sartorius et al. has recently resumed the deep sampling after CO2 laser vaporization in 10 patients experiencing acute flare; CNS were present in deep levels in all 10 patients, whereas Corynebacteria and α-haemolytic streptococci (including S. Milleri) were present at other levels.54 The latter are microaerophilic or anaerobic and induce abscess formation. The absence of Staphylococcus aureus, whatever the level of sampling is striking. A recently reported study55 has partially confirmed these results showing the predominance of Staphylococcus lugdunensis in low severity grade lesions (Hurley I). In more severe lesions anaerobic bacteria, actinomycetes and streptococci of the Milleri group were present. Staphylococcus aureus was only found in superficial samples, which may indicate a clinically irrelevant colonization. Hence, CNS and anaerobic bacteria are the main bacteria recovered from HS lesions.
- Most CNS infections have a slow, subacute evolution. CNS are able to form biofilms on medical devices and hence escape an immune reaction. S. lugdunensis has special features in the group of CNS: as a frequent resident of the perineum it can be responsible for infections e.g. abscesses and wound infections. Clinically, infections caused by S. lugdunensis are similar to those caused by S. aureus rather than those caused by other CNS.56
- Sporulated anaerobes belonging to the genus Clostridium are rarely present in HS lesions. Nonsporulated anaerobes are saprophytic in natural human cavities. They do not produce toxins but enzymes and anti-phagocytic factors. Among the nonsporulated anaerobes are gram-positive cocci (Peptostreptococcus) and gram-negative cocci (Veillonella); gram-positive bacilli (Actinomyces, Propionibacterium) and gram-negative bacilli (Bacteroides, Prevotella, Porphyromonas, Fusobacterium, Bilophila). Most infections provoked by nonsporulated bacteria are polymicrobial with a mixture of aerobes and anaerobes. The presence of aerobes lowers the availability of oxygen and thus promotes the growth of anaerobes. Some anaerobes are able to inhibit aerobic phagocytosis. A bacterial synergy is thus created in these mixed infections.
- Anaerobes are frequently responsible for soft tissue infections: cellulitis, dermo-hypodermitis, myonecrosis; in HS their presence should be systematically suspected. It becomes self evident in case of foul odour of exudates. The absence of positive bacterial culture in spite of abundant flora on direct examination is a clue to their responsibility; ‘sterile pus’.
As a whole, bacterial infection in HS is mainly due to CNS and anaerobes and is polymicrobial, a usual feature of anaerobic infections.
Distinctive features of infection in HS
- There is no lymph node enlargement in the vicinity of the lesions in spite of inflammation and bacterial infection.57
- Acute super-infection by Staphylococcus aureus and/or Streptococci are exceedingly rare in spite of numerous openings on the skin.
Obesity
Association of HS with being overweight and obesity (overweight at BMI 25–30, obesity at BMI≥30, severe obesity at BMI≥35) has been recorded for a long time in open series:
In a case–control study of 302 medically assessed patients and 906 control subjects, an association with body mass index was significant [odds ratio = 1.12 (1.08–1.15)] for each increase in 1 U of BMI. The multivariate OR for being overweight was 2.08 (1.40–3.08) and was 4.42 (2.82–6.93) for obesity.11 In the same series of patients, severity as assessed by the Sartorius score was linked to BMI (P < 0.001).5
In a series of 251 patients overweight and obesity were prevalent: a mean ± SD BMI of 28.3 ± 6.5 kg/m2, one-third being overweight and one-third obese. For 110 of these patients for whom severity was assessed using HSS (a variant of Sartorius score) there was a significant but weak positive correlation (P = 0.036);(mostly women and only obesity, not overweight).6
A recent incidence study in USA in reported 268 incident cases; no link to BMI was found.12
In conclusion, overweight and obesity are clearly associated factors in HS; their role as severity factor is highly probable.
Tobacco
The link between HS and cigarette smoking has been well-established by several studies.2 The rate of active cigarette smokers has been recorded to be 88.9% in a case–control study.61
A multivariate analysis in a French population showed a highly significant association between the prevalence of HS and current smoking with an OR of 12.55 (8.58–18.38). The association did not exist for exsmokers.11 Only one study fails to support this association.62
Such a high link is considered an argument in favour of smoking being a risk factor for HS; there is majority approval of this opinion although there is no data about the temporal relationship between smoking and the first manifestations of HS.
The relationship between severity of HS and cigarette smoking has been studied with conflicting results: one study of 115 patients found a slight association: active smokers being more severe (as measured by HSS a modification of the Sartorius score) than nonsmokers (P = 0.03) but not different from ex-smokers.6 Conversely, no relationship with disease severity was found in a series of 302 patients5 and in a study of 268 incident cases in which the link observed in an univariate analysis disappears in a multivariate analysis.12
Studies of the temporal relationship between smoking and HS and follow-up studies of smoking initiation and cessation are highly needed
Mechanical stress
The role of mechanical stress as a trigger for the outburst of new lesions has been put forward by some practitioners in consideration of several facts:
- The role of obesity as a risk factor and a severity factor.
- The opinion and testimony of patients saying that wearing tight clothes induces outburst of lesions.
- HS–like lesions have been reported in a leg stump as consequence of mechanical friction.63
However, mechanical stress as a trigger for HS has still to be proven.
Complications
Acute complications
Acute super-infection by S. aureus and/or S. pyogenes is extremely rare. Enlarged lymph nodes are very unusual.57
Chronic local complications
Lymphatic obstruction and lymphedema, scrotal elephantiasis may complicate long-standing inflammation at the genitoanal area. Unusual complications of long-standing untreated disease at this location include: fistulae formation into the urethra, bladder, rectum or peritoneum (exclusion of Crohn's disease is required).
Cancer
Squamous cell carcinoma may arise from chronic (10–30 years of evolution) lesions particularly in men (some isolated reports in women) and in the buttock area; most published cases are isolated case reports; one case series with a review of > 50 published cases has recently been published.65 The diagnostic of cancer is usually tardy and therefore the prognosis very poor; Biopsy should be performed in every long-lasting lesion of the gluteal area.66
One registry based study from Sweden67 found an excess of many type of visceral cancers (SIR 1.1–1.8); this result has still to be confirmed.
Systemic complications
Chronic suppuration in severe widespread disease, anaemia, hypoproteinaemia. Amyloidosis are historical complications which have become rare.
Rheumatological disorders66, 68
Various types – but frequently mixed heumatological diseases – have been reported in association with HS: Axial arthritis; peripheral arthritis- including dactylitis; enthesopathies, SAPHO. The prevalence of the association is not known. The most documented is spondylarthropathies sometimes in association with Crohn's disease; even if HS and arthritis don't have a strict parallel evolution there is a general agreement that control of HS improves rheumatological symptoms. Arthritis almost always begins after HS; sacro-iliitis is frequently unilateral; thoracic anterior wall and peripheral large joints are frequently involved. Biological inflammatory markers are elevated; HLA-B27 is negative. Radiographic features include erosions, osteoporosis, sacroiliitis and syndesmophytes.
Nonsteroidal anti-inflammatory drugs, corticosteroids, methotrexate and anti-TNF drugs are used in the treatment of rheumatological diseases associated with HS.
Adjuvant therapy
Based on expert opinion it is recommended that adjuvant therapy is offered to patients in the form of general measures and specific help with bandaging lesions in order to improve the patients' quality of life.
There are no trials or studies to support this recommendation.
General measures
Descriptive studies have shown a positive correlation between disease severity and BMI and tobacco smoking.6 Although no data exist for improvement of HS lesions after reduction in weight and cessation of tobacco smoking, the general expert opinion is that cigarette smoking and overweight have to be avoided.
There is no evidence assessing the routine use of topical chlorhexidine or other aseptic washes, and bacterial swabs of lesions are frequently negative suggesting that superficial bacterial flora at the skin surface is not likely to play a significant role.
Bandages
Suppuration may occur in spite of appropriate treatment. Suppuration causes psycho-social and physical discomfort through maceration and odour, and influences the patients' quality of life negatively.
Bandages used must be customized due to the anatomical variation, and should be absorbent, nonirritant. They should keep the surface dry and absorb smell. Dedicated HS-bandages are not currently available.
There is no evidence to support specific bandages.
Psychosocial support measures
There is considerable evidence to suggest that patients quality of life is negatively affected by HS (see section 3.2) and the effect includes depression and general social integration.
No specific studies are available to describe the effect of psychosocial support measures in HS, by analogy to e.g. interventions in eczema and other chronic diseases it is speculated that such interventions may be of considerable benefit to the patients and are therefore recommended in a protocoled setting to facilitate accumulation of evidence.
Medical therapy
Topical therapy – nonantibiotics
Exfoliants and peels
Topical resorcinol is the only exfoliant described.69 A case-review of 12 women treated with topical resorcinol 15% described good effect of the treatment compared to previous experience, which included surgery (12/12) and antibiotics (8/12).
Resorcinol 15% was administered in an oil/water cream with emulsifying waxes; ingredients listed as cremor lanette, consisting of the following components: alcohol cetylicus et stearylicus emulsificans b (cetostearyl alcohol type b), acidum sorbicum (sorbates), Cetiol v (decyloleat), sorbitolum liquidum cristallisabile (sorbitol), aqua purificata (water).
Mechanism: Resorcinol (m-dihydroxy benzene) exhibits keratolytic, antipruritic and antiseptic activities.
Pretreatment assessment: Resorcinol has only been described in recurrent Hurley stage I or II patients.
Indication and contraindication: Recurrent lesions in patients with Hurley stage I or II HS.
Dosage and duration of treatment: In cases of flares, patients were instructed to start treatment twice daily with 15% resorcinol cream within hours. Patients were allowed to continue the topical treatment as a maintenance treatment once daily after the flare, but most used the topical medication only when flares occurred.
Response rate: All 12 women described responded by improvement of lesional draining and subsequent involution.
Follow-up investigations: None.
Complications: Structurally related to phenol and isomerically with catechol and hydroquinone, it can give rise to an aspecific irritant contact dermatitis, while its sensitizing power seems to be only moderate.70 A few cases of contact allergy to resorcinol from various sources have been described, and testing is possible.
Toxicity has been reported from ingestion of resorcinol and percutaneous absorption occurs. Systemic toxicity following topical use of resorcinol, is extremely rare, but physicians must be aware of the potential risk.
No formal studies or guidelines are available on the use of resorcinol in pregnancy.
Other therapies
No formal studies have been conducted but expert opinion suggests that the use of adapalene or azelaic acid may occasionally be beneficial, but must currently be considered experimental.
Topical antibiotics
Clindamycin is the only antibiotic that has been studied as a topical agent. No data are available on the topical use of any other antibiotics.
Clindamycin
It was tested in a double-blinded randomized trial of 27 patients with stage I or mild stage II HS.71 Patients were treated with topical clindamycin 0.1% or placebo. Patients and physicians made monthly evaluations of overall effect, abscesses and nodules. All patients' assessments were in favour of clindamycin (P < 0.01) and lesion counts were in favour of topical clindamycin at 2 and 3 month; the most significant effect was observed on superficial lesions i.e. folliculitis, papules, pustules; the effect on deep lesions i.e. nodules, abscesses was very low if any.
Mechanism: Clindamycin binds to the 50s ribosomal subunit of bacteria where it disrupts transpeptidation and subsequently protein synthesis in a similar manner to macrolides although not chemically related.
Pretreatment assessment: Allergy to constituents of topical compounds must be considered, but generally the potential of topical treatment for significant adverse effects is less than for systemic treatment.
Because of the increased risk of adverse events under systemic administration caution should be exercised when treating individuals with a history of gastrointestinal disease, particularly colitis, or risk of heavy colonization.
Selection of resistant microbes may occur with therapy, and appropriate measures should be taken as indicated by the clinical situation.
Indication and contraindication: Localized Hurley Stage I or mild stage II disease.
Dosage and duration of treatment: Application of lotion containing clindamycin b.i.d. for 3 months. Treatment may be prolonged if clinically indicated.
Response rate: There was a significant 4.5-fold better improvement to clibdamycin than to placebo using of a for the study constructed disease score.71
Follow-up investigations: As indicated clinically.
Complications: Stinging and skin irritation. Selection of resistant bacterial strains.
Systemic antibiotics
Systemic treatment is indicated when more severe or widely spread lesions are present.
Tetracycline
One small randomized controlled trial has compared topical clindamycin 0.1% b.i.d. with tetracycline 500 mg b.i.d. in a randomized, double-blind, double-dummy trial without finding any difference in neither physicians' nor patients' assessment of overall effect, soreness, nodules or abscesses.72 The trial was not designed to establish equipotency.
Mechanism: Tetracyclines bind to the 30S ribosomal subunit reversibly and prevents the binding of the amino acyl tRNA and thus translation.
Pretreatment assessment: Should not be administered to pregnant women or children younger than 9 years old due to risk of discoloration of permanent teeth (+10%).75
Patients should be advised that photosensitivity may occur on exposure to direct sunlight.
Renal impairment may cause accumulation of tetracyclines leading to liver toxicity, azotaemia, hyperphosphataemia and acidosis.
Indication and contraindication: More widely spread Hurley stage I or mild stage II disease.
Dosage and duration of treatment: Tetracycline 500 mg b.i.d. has been tested for 4 months. Can be prolonged if clinically indicated.
Response rate: An approximately 30% reduction in disease severity as assessed by the physician's general assessment.73
Follow-up investigations: As indicated clinically.
Complications: A comprehensive list of potential complications of tetracycline therapy is beyond the scope of these guidelines. Relevant adverse effects include the risk of microbial resistance, concomitant use of oral contraceptives and teratogenicity.
Clindamycin – Rifampicin
Three open case series involving a total of 114 patients have explored the combined use of systemic clindamycin and systemic rifampicin in the treatment of HS.74-76 All studies are open case-series, two have retrospective information,75, 76 one has prospective information.74 All studies conclude the treatment to be beneficial.
Mechanism: Clindamycin: Clindamycin binds to the 50s ribosomal subunit of bacteria where it disrupts transpeptidation and subsequently protein synthesis in a similar manner to macrolides although not chemically related.
Rifampicin: Inhibits DNA-dependent RNA polymerase activity in bacteria, by interacting with bacterial RNA polymerase.
Pretreatment assessment: Because of the increased risk of adverse events caution should be exercised when treating individuals with a history of gastrointestinal disease, particularly colitis or risk of heavy colonization.
Rifampicin is a strong inducer of cytochrome P450 and may influence the metabolism and toxicity of other drugs metabolized by the same pathway, such as e.g. oral contraceptives.
Selection of resistant microbes may occur with therapy.
Indication and contraindication: Any stage active inflammatory HS.
Dosage and duration of treatment: 300 mg b.i.d. given in combination with rifampicin (600 mg daily given either as 1 or 2 doses)74, 75 for 10 weeks, although one study suggested that results were similar when patients were treated <10 weeks. There were more nonresponders among those treated <10 weeks. Even if not present in the literature there is the need to adapt the doses to bodyweight 600 mg/day is for a BW of 60 kg.
Response rate: Reported outcome variables are not standardized. After 10 weeks of clindamycin (300 mg b.i.d.) and rifampicin (600 mg, either ×1 or b.i.d.) the following responses have been reported74, 75:
- Complete remission in 8/1075 and 8/7074 patients.
- An average 50% reduction in Sartorius score, and change in pain from 7 to 3 (NRS, 0–10).
- A reduction in number of patients with pain 15 + days per month from 40/70 to 10/70.
- A reduction in number of patients with suppuration 15 + days per month from 48/70 to 20/70.
Among patients with varying dosages of clindamycin and rifampicin for varying periods of time a clinically meaningful response was noted in 28/34 and complete remission in 16/34.74
Follow-up investigations: As indicated clinically.
Complications: A substantial number of patients interrupted treatment due to gastrointestinal adverse effects, none due to Clostridium difficile.
Mendonca & Griffiths75 reported four patients stopped treatment due to adverse gastrointestinal effects.
Gener et al.74 reported that 10/70 patients complained of adverse effects during 10 weeks of treatment. Eight of these stopped treatment (six due to temporary GI upset, one due to rash and one due to lack of effect after 7 weeks of treatment).
Van der Zee et al.76 reported adverse effects in 13/34 patients, and nine of these stopped treatment (six of these due to diarrhoea. Of the 13/34 patients who experienced adverse effects these were: diarrhoea in nine patients (26%). In addition, two patients experienced a Candida vaginitis, two nausea, two dizziness and one glossodynia.
Other antibiotics
Systemic treatment with a combination of rifampicin-moxifloxacin-metronidazole, either alone or preceded by systemic ceftriaxone in half of all patients, has been described as effective in an retrospective study of 28 patients with treatment resistant stage II and III disease.77 Patients who showed response after 12 weeks of initial treatment were treated for an additional 12 weeks using a combination of moxifloxacin and rifampicin. The intensive treatment lead to complete response in 16/28 patients. Main adverse effects were gastrointestinal disturbances (64% of patients) and vulvovaginal candidiasis (35% of female patients).
A range of other topical and systemic antibiotics have been suggested in case reports and in expert opinion, but none have been systematically evaluated even at the level of open prospective case-series. Currently, these should therefore be considered as experimental therapies.
Anti-inflammatory therapy
Intralesional corticosteroids
The use of intralesional triamcinolone acetonide 5–10 mg/ml has been advocated for the rapid reduction in inflammation associated with acute flares and for management of recalcitrant nodules and sinus tracts.78 It is utilized as both monotherapy and an adjunct to systemic therapies. When effective, clinical response (flattening, resolution or spontaneous discharge of nodules) is seen within 48–72 h. Therapy is contraindicated if clinical suspicion of bacterial infection exists. Local complications include atrophy, pigmentary change and telangiectasia. Systemic side-effects at recommended doses are uncommon.79 Complication with superinfection is reported as rare.78
Systemic corticosteroids
Mechanism: Synthetic corticosteroids have anti-inflammatory, immunosuppressive, antiproliferative and vasoconstrictive effects. Anti-inflammatory effects include inhibition of prostaglandin, leukotriene and cytokine production (tumour necrosis factor (TNF), interleukins (IL), interferon-γ, colony stimulating factor) resulting in inhibition of leucocyte access to sites of inflammation.
Pretreatment assessment: Assess baseline blood pressure, weight, haematology, renal and hepatic function, blood glucose and fasting lipids. Risk assessment for osteoporosis is required if long-term therapy is under consideration.
Indication and contraindication: There are limited data on the use of corticosteroids in HS. Short and long-term therapy can result in rebound flare on withdrawal. Short-term, rapidly tapering therapy can provide benefit in reduction in inflammation associated with acute flares.78 In the event of clinical relapse on dose reduction, introduction of a second line anti-inflammatory or immunosuppressive agent is recommended.78, 80, 81 Routine long-term use is not currently recommended.
Contraindications include untreated systemic infection; caution should be taken in the patient with a pre-existing disease that may be exacerbated by corticosteroids. Important drug interactions include the antimicrobials erythromycin, clarithromycin and rifampicin. Care should be taken in pregnancy due to the potential risk of neonatal adrenal suppression.82
Dosage and duration of treatment: Systemic corticosteroid dose and duration should be kept to a minimum to limit long-term complications. A dose of 0.5–0.7 mg/kg oral prednisolone is recommended for short-term use for acute flares; the dose should be rapidly tapered to stop over weeks.78
Response rate: Limited case reports and one case series describe response to the corticosteroid agents hydrocortisone, dexamethasone and prednisolone, as short-term monotherapy and long-term combination therapy. Use of short-term systemic hydrocortisone monotherapy (60–80 mg od tapering to stop at day 15–56) is reported in a series of four cases of variable severity with sustained remission observed at 12 months.83 Efficacy of long-term dexamethasone combination therapy is described in a single case of severe HS when used in combination with a Gonadotropin-releasing hormone agonist (leuprolide acetate).84 Use of prolonged prednisolone monotherapy (60 mg od reduced to 25 mg od; duration not specified) in a single case with severe disease resulted in 65% improvement.85 Prolonged prednisolone combination therapy (20 mg od to stop over 27 weeks) with antimicrobials followed by isotretinoin resulted in sustained clinical response in one case.86
Follow-up investigations: Monitor blood pressure, urinalysis for glucose and renal function after 1 month and then 2 monthly. Dual energy X-Ray absorptiometry (DEXA) scan at regular intervals is recommended in the event of long-term therapy.
Complications: A comprehensive list of potential complications of corticosteroid therapy is beyond the scope of these guidelines. Relevant cutaneous adverse effects include the risk of rebound disease flare on therapy withdrawal.
Dapsone
Mechanism: Dapsone (4′4′-diaminodiphenyl sulphone) is a sulphone drug with antibacterial and anti-inflammatory properties; it has established efficacy in dermatoses associated with prominent neutrophilic infiltration or immune complex deposition (particularly IgA). Antibacterial activity is mediated through inhibition of dihydrofolic acid synthesis; the mechanism of anti-inflammatory activity is less well defined and may relate to inhibition of chemoattractant-induced signal transduction, suppressing neutrophil recruitment and local production of toxic respiratory and secretory products.
Pretreatment assessment: Baseline haematology, reticulocyte count, renal, hepatic function and glucose 6-phosphate dehydrogenase (G6PD) levels are required.
Indication and contraindications: Use of dapsone should be reserved for patients with mild to moderate disease (Hurley stage I or II). Therapy should be initiated where standard first or second line agents fail.
Contraindications include severe G6PD deficiency, sulphonamide allergy, severe anaemia and acute porphyria. Potential relevant therapeutic interactions include trimethoprim and rifampicin amongst others. Dapsone is not teratogenic, although does cross the placenta. Neonatal haemolysis and methaemoglobinaemia are reported with third trimester use. Dapsone should be avoided during breast feeding.87
Dosage and duration of treatment: Efficacy is reported at doses of 25–200 mg a day. Use of high doses is often limited by symptomatic or haematological complications. Reported duration of therapy is variable. The minimal duration of therapy based on interval to response, is 3 months. When effective, rapid relapse may occur on therapy withdrawal. There are no data on maximum duration of therapy (reported range 3–48 months).
Response rate: In a retrospective review of 24 patients (majority female) treated with dapsone (50–200 mg a day for 1–48 months), a slight or significant clinical improvement was observed in 38% of cases. Significant complications led to therapy withdrawal in 8%. Rapid relapse was seen in patients who attempted therapy cessation. None of the cases with severe disease (Hurley Stage III) responded.88 In a retrospective series of five patients on dapsone (25–150 mg/day) improvement was reported in all cases after 4–12 weeks.89 Continuous therapy was required for sustained disease control over a median follow-up of 24 months.89 A second retrospective series of five patients (all female) on dapsone (25–100 mg a day, unspecified duration), reported almost complete resolution in all cases; continuous therapy was required to prevent relapse.90
Follow-up investigations: Assess haematology and reticulocyte count 1–2 weekly for the first month. Thereafter, haematology, renal and liver function monthly for 3 months then every 3–6 months. Assess methaemoglobin levels in any patient complaining of headache, fatigue or shortness of breath.
Complications: Major adverse effects include haemolysis, haemolytic anaemia, methaemoglobinaemia, hypersensitivity syndrome, agranulocytosis and peripheral naeuropathy. Haematological and neurological complications are often dose related. Other side-effects include sulphaemoglobinaemia, nephrotic syndrome, psychoses, reduced fertility (males) and hepatitis.
Ciclosporin A
Mechanism: Ciclosporin A is a calcineurin inhibitor with potent immunosuppressive activity. It specifically targets T lymphocytes, suppressing both the induction and proliferation of T-effector cells and inhibiting production of lymphokines (e.g. TNF-α and IL-2). A direct effect on keratinocytes has been demonstrated independent of functioning T cells.
Pretreatment assessment: Baseline assessment of blood pressure, screening for active infection and malignancy is required. Pretreatment investigations include haematology, renal and hepatic function, lipid profile, uric acid, magnesium levels+/- HIV testing.
Indication and contraindication: Beneficial effects of ciclosporin A are reported in limited cases. Use of ciclosporin A should therefore be reserved to cases where failure of response to standard first, second and third line therapies occurs until further evidence is available.
Contraindications include active infection, uncontrolled hypertension, malignancy and high cumulative doses of psoralens and UVA photochemotherapy. Careful consideration should be given to potential food and drug interactions. An exhaustive list is beyond the scope of this guidance; relevant examples include antimicrobial agents (e.g. macrolides, doxycycline, rifampicin, trimethoprim, quinolones), oral contraceptives and nephotoxic agents e.g. nonsteroidal analgesia.91
Dosage and duration of treatment: There are limited data assessing appropriate dose or duration of ciclosporin A for HS. Daily doses of 2–6 mg/kg have been used for variable duration (6 weeks–7 months).92, 93
Response rate: Beneficial response to ciclosporin A is reported in four cases. A single case treated with short-term high daily dose ciclosporin A monotherapy (6 mg/kg for 6 weeks) experienced moderate response after 6 weeks.92 A patient with severe hidradenitis and pyoderma gangrenosum responded to ciclosporin A monotherapy (4.5 mg/kg daily for 4 months) with sustained healing of sinuses and reduction in pain at month 15.94 Use of step down ciclosporin A monotherapy (4 mg/kg daily for 2 months, 2 mg/kg daily for 5 months) led to reduction in severe inflammatory episodes in one case.93 Combination ciclosporin A (3 mg/kg daily for 4 months) with tapering corticosteroids (2 months) resulted in 4 months of remission in one case.93
Follow-up investigations: Assess blood pressure, urinalysis, haematology, renal and hepatic function at 2 weekly intervals for the first 3 months and 3 monthly thereafter. Routine monitoring of ciclosporin A levels is not required unless concerns of drug adherence or toxicity from drug interaction exist.
Complications: The major adverse effects are nephrotoxicity, hypertension and an increased risk of malignancy (primarily skin cancer in patients previously receiving photo-chemotherapy). Other common complications include gastrointestinal disturbance, gingival hyperplasia, hypertrichosis, hepatic dysfunction, tremor, headache, paraesthesia, myalgia, fatigue, hyperlipidaemia, hyperkalaemia, hypomagnesaemia and hyperuricaemia.94
Hormones
Mechanism: There are indications that antiandrogens, such as cyproterone acetate, and estrogens improve HS,95, 96 while progestogens induce or worsen a pre-existing HS due to their androgenic properties.96
Pretreatment assessment: Baseline screening of ongoing pregnancy, cardiovascular risk (incl. cardiac and leg vein status, thrombotic markers, body weight, serum lipids, smoking), renal and hepatic function.
Indication and contraindication: Female patients with menstrual abnormalities, signs of hyperandrogensim or upper normal or high serum levels of dehydroepiandrosterone, androstenedione and/or sexual hormone-binding protein.
Dosage and duration of treatment: The combined treatment with the antiandrogen, cyproterone acetate and ethinyl oestradiol on four women with long-standing HS controlled the disease successfully in all patients with 100 mg/day cyproterone acetate using the reversed sequential regimen; lowering the antiandrogen to 50 mg/day caused deterioration.95 In further seven females receiving hormonal contraception, contraceptives with 19-nortestosterone derivatives, which exhibit androgenic properties, induced or exaggerated HS, whereas other contraceptives did not influence or improved HS at the same individuals.96 A double blind trial of two contraceptive pills one containing 50 mg of cyproterone acetate and the other one norgestrel showed no difference in the improvement observed in female patients with HS.97
Response rate: All reported patients improved but no evidence-based data exist.
Follow-up investigations: Cardiac and leg vein status, thrombotic markers, serum lipids, renal and hepatic function.
Complications: Mild headache, breast pain, nausea, dysmenorrhoea, neurosity, gain of weight, sinusitis, influenza-like symptoms, abdominal pain.
Biologics
According to current evidence adalimumab and infliximab are effective in the treatment of moderate to severe HS and improve the quality of patient life, with adalimumab more tolerable.98-100
Adalimumab
Mechanism: Adalimumab is a fully human therapeutic monoclonal antibody. It corresponds to the human immunoglobulin IgG1 and has heavy and light chain variable regions exhibiting specificity for human TNF-α. Adalimumab binds with high affinity and specificity to soluble and membrane-bound TNF-α. Thus, the binding to the TNF-α receptor is prevented (p55 and p75) and blocks the biological effect of TNF-α.
Pretreatment assessment:
- Exclusion of acute infection.
- Exclusion of tuberculosis in accordance with current national guidelines for the use of TNF-α inhibitors.101
- HIV infection or viral hepatitis should be excluded with appropriate patient history, clinical and/or laboratory evidence.
- Pregnancy in women of childbearing age should be excluded and secure contraception.
- Patients should be advised that the course of infections could be more severe or atypical during treatment and that they have to early visit a physician in uncertain cases.
Contraindications: Major contraindications/limitations
Absolute contraindications:
- Heart failure NYHA class III - IV
- Pre-existing tuberculosis or other severe infections
- Pregnancy and lactation
Important relative contraindications:
- Severe liver disease
- Demyelinating processes
- Malignancies (except: basal cell carcinoma) and lymphoproliferative disorders as well as a history of malignancy
- Vaccination with live vaccines
Dosage and duration of treatment:
Response rate: There are different rates of response to adalimumab reported in case series and in a current, prospective controlled study.
Administration of adalimumab with a cumulative response rate of 58% (improvement ≥50% in 23 patients) has been reported in case reports with 42 patients with moderate to severe HS10, 103-106 (Table 3).
| Biological agent | No. patients | Schema | Duration | Results | ||
|---|---|---|---|---|---|---|
| Improvement ≥ 50% | Relapse after discontinuation or surgery required | |||||
| No | Yes | |||||
| Adalimumab | 42 | 80 mg sc 1st week, 40 mg sc 2nd week | 19 | 23 (58%) | 10/14 (71%) | |
| Etanercept | 34 | 25 mg sc 2x/week | 3–10 m | 19 | 15 (44%) | 10/14 (71%) |
| Infliximab | 73 |
5–10 mg/kg iv 0, 2, 6 week |
2.5–72 m | 29 | 42 (58%) | 15/35 (43%) |
| Ustekinumab | 3 | 45 mg sc 0, 4, 16 week | 6 m | 2 | 1 (33%) | 2/3 (66%) |
- Studies with ≥ 3 patients; patients with Crohn′s disease were excluded.
In a prospective, open study with 15 patients with moderate-to-severe HS, medium-term treatment (3 months) with adalimumab resulted in significant reduction of Sartorius score by week 24 with a marked improvement during the first month.107 VAS score and DLQI showed a significant decrease at week 24. In another prospective, open study with six patients with moderate to severe HS, medium-term treatment (3 months) with adalimumab failed to reduce HSSI score in any of the patients at week 2, 4, 8 and 12.10 VAS and DLQI scores also failed to show statistically significant improvement.
In a prospective, randomized (2 : 1), double-blind, placebo-controlled study of adalimumab treatment (80 mg sc at 1st week and 40 mg sc every 2nd week) of 21 patients with HS for 3 months significant improvement was detected at 2 weeks (P < 0.024) but not at the end of treatment (P = 0.07)108 (Table 4). In another larger prospective, randomized (1 : 1 : 1), double-blind, placebo-controlled study of adalimumab treatment (40 mg sc once weekly: 40 mg sc every other week: placebo) of 154 patients with moderate to severe HS who were unresponsive or intolerant to oral antibiotics (tetracycline, doxycycline, minocycline) 17.6% of weekly patients (9 of 51), 9.6% of every other week patients (5 of 52) and 3.9% of placebo patients (2 of 51) achieved clinical response at week 16 [weekly vs. placebo difference 13.7% (CI, 1.7% to 25.7%), P = 0.025]; every other week vs. placebo difference 5.6% (95% CI, 4.0% to 15.3%, P = 0.25)8 (Table 4). Among patients with VAS pain scores of 10 mm or greater at baseline, the proportion with a clinically relevant improvement in pain at week 16 was significantly higher for patients in the weekly group (47.9%) than in the placebo group (27.1%) [difference 20.4% (CI, 1.2% to 39.7%), P = 0.037]. More than 40% of patients receiving weekly or every other week therapy crossed this threshold of pain reduction at week 2. Mean improvement in DLQI scores between baseline and week 16 were 6.3 for patients in the weekly group, 3.2 for those in the every other day group and 2.3 for patients in the placebo group (weekly vs. placebo, P = 0.001). Serious adverse event rates were 7.8%, 5.8% and 3.9%, respectively.
| Agent | No. patients | Schema | Duration (months) | Results |
|---|---|---|---|---|
| Adalimumab | 21 (2 : 1) |
80 mg sc 1st week 40 mg sc 2nd week |
3 m | Significant impovement (P < 0.024) after 2 week (but P = 0.07 after 12 week) |
| 154 (1 : 1 : 1) | (A) 40 mg sc/week | 3 m | (A) Improvement of 17.6% in weekly patients (P = 0.025) | |
| (B) 40 mg sc every other week | (B) Improvement of 9.6% in every other week patients (ns) | |||
| (C) placebo | (C) Improvement of 3.9% in placebo patients | |||
| Etanercept | 20 |
50 mg sc 2x/week |
3 m | No difference compared to placebo (cross-over) |
| Infliximab | 33 |
5 mg/kg 0, 2, 6 week |
2.5 m |
Significant improvement with infliximab (P < 0.001) (>50% improvement was 27% under infliximab; 5% under placebo) Recurrence of disease after discontinuation |
Follow-up investigations: Relapses after discontinuation of treatment and/or surgery required was reported in 10 of 14 among the case reports patients (71%).102 Relapses after discontinuation were also reported in the patients group reported by Miller et al.108 Mean time to relapse was 11 weeks after discontinuation of treatment, but even at the final visit Sartorius score was significantly lower than at baseline.107 A decrease in response was seen after the switch from adalimumab weekly to every other day dosing in an open follow-up study by Kimball et al.8 at weeks 16 to 52.
Complications: Under adalimumab treatment tolerance was satisfactory.8, 10, 107 In the placebo-controlled studies reaction at the injection site was the most commonly reported adverse drug reaction (adalimumab: 20% of patients, placebo: 14%). No major adverse events could be observed.8, 109 Under adalimumab therapy increased infections may occur, especially at the upper respiratory tract, bronchitis and urinary tract infections. Reported serious infections are pneumonia, septic arthritis, postoperative infections, erysipelas, diverticulitis and pyelonephritis. Autoantibodies (ANA, anti-dsDNA antibodies) can be induced, a rare ‘lupus-like syndrome’ was described. Very rarely, malignancies, especially lymphomas occur.
Women should receive contraception up to 5 months after the last dose of adalimumab. Should pregnancy be diagnosed under adalimumab treatment, it should be discontinued. Damage to the child cannot be expected due to lack of embryo or fetal toxicity (FDA classification B). During lactation Adalimumab is contraindicated due to the potential transition into the milk.
Infliximab
Mechanism: Infliximab is a chimeric (mouse/human) monoclonal antibody against TNF-α. It is an IgG1 immunoglobulin with human sequences in the constant regions and murine sequences in the complementarity-determining regions of the light and heavy chains. It binds specifically to both soluble and transmembrane, receptor-bound TNF-α. Soluble TNF-α is ligated and its proinflammatory activity is neutralized. Moreover, binding to cell membrane-bound TNF-α leads to an elimination of the affected cells, possibly due to complement activation and/or antibody-dependent cellular cytotoxicity, but also due to induction of apoptosis. Infliximab has a serum half-life of about 8 to 9.5 days. The elimination period is up to 6 months.
Pretreatment assessment:
- Exclusion of acute infection.
- Exclusion of tuberculosis in accordance with current recommendations of the Paul Ehrlich Institute in Germany.101
- HIV infection or viral hepatitis should be excluded with appropriate patient history, clinical and/or laboratory evidence.
- Pregnancy in women of childbearing age should be excluded and secure contraception.
- Patients should be advised that the course of infections could be more severe or atypical during treatment and that they have to early visit a physician in uncertain cases.
Contraindications: Absolute contraindications
- Heart failure NYHA class III-IV
- Known hypersensitivity to mouse proteins
- Pre-existing tuberculosis or other severe infections
- Pregnancy and lactation
Important relative contraindications
- Malignancies (except: basal cell carcinoma) and lymphoproliferative disorders as well as a history of malignancy
- Vaccination with live vaccines
- Autoimmune diseases
- Demyelinating processes
Dosage and duration of treatment:
-
(a) To condition for a curative surgical procedure: Infliximab 5 mg/kg body weight may be used.102
(b) For long-term therapy: infliximab 5 mg/kg body weight on day zero, two, six and then regularly every 8 weeks.
- With longer intervals between infusions, the probability of the formation of infliximab antibodies increases.
- Infliximab is administered intravenously over a period of 2 h. If no infusion reactions occur, it can also be given over 1 h. During the infusion and for 1 h after it monitoring of patients for infusion reactions is necessary.
Response rate: Administration of infliximab with a cumulative response rate of 58% (improvement ≥50% in 42 patients) has been reported in case reports with 73 patients with moderate to severe HS109-118 (Table 3). In a prospective, randomized, double-blind, placebo-controlled, cross-over study of infliximab treatment (5 mg/kg iv at weeks 0, 2, 6) of 33 patients with HS for 2 months no significant difference in the >50% improvement was detected (primary end point), while a significantly higher 25–50% improvement rate was detected under infliximab (27% vs. 5% under placebo9) (Table 4). In a retrospective comparative (1 : 1) study with 20 patients, a significantly greater reduction was detected for infliximab (5 mg/kg iv at weeks 0, 2 and 6) in mean Sartorius score (56%) in comparison with adalimumab (40 mg sc every other week) (34%).119
Follow-up investigations: Long-term treatment (1 year) of eight patients with moderate-to-severe HS with infliximab resulted in significant reduction of the number of involved sites (P < 0.001) and flares (P < 0.05).120 The mean initial DLQI 20/30 (range 9–30) significantly improved to 6/30 (P < 0.001). In a further study with long-term treatment (4 years) of 10 patients with moderate-to-severe HS with infliximab 80% responses were reported.116 Response (≥50%) occurred after 3 to 7 drug administrations (13 to 45 weeks). Four of eight patients relapsed despite treatment (after six administrations). Moreover, recurrences after discontinuation of treatment and/or surgery required was reported in 15 of 35 among the case reports patients (43%).102 In the study by Grant et al.9 recurrences also occurred after discontinuation of treatment.
Complications: The long-term tolerance (n = 8 patients, 1 year) was satisfactory with only four minor infections, one keratoacanthoma and one case of rapidly resolving hepatitis.120 In a retrospective comparative study on the safety of infliximab and adalimumab in 5 of 27 patients (18%) who were treated for an average of 12 months with infliximab a polyarthritis was detected, which healed spontaneously 4 months after discontinuation of infliximab.109 This side-effect was not observed under adalimumab treatment.
There are extensive data on the safety of treatment with infliximab in inflammatory bowel disease, arthritis and psoriasis vulgaris.102 Acute infusion reactions with mild chills, headache, flushing, nausea, dyspnoea or infiltration at the infusion site are common. The likelihood of an infusion reaction is higher in patients with infliximab-specific antibodies. Anaphylactoid reactions, regardless of whether infliximab-specific antibodies are present, can occur. Retreatment after longer treatment periods may induce arthralgia, myalgia and angioedema. A moderate infusion reaction can be prevented or attenuated by prior administration of antihistaminics or even prevented.105 By the addition of low-dose methotrexate (5–10 mg/week), the formation of antibodies to infliximab can be reduced. Infections, worsening of heart failure, demyelinating diseases, hepatotoxicity, leukopaenia, neutropaenia, thrombocytopaenia or pancytopaenia lupus erythematosus-like syndrome may also occur.
Other TNF-α inhibitors
Treatment of patients with HS with etanercept has also been reported in case reports121-124 and a clinical study.125
Mechanisms: Etanercept is a fusion recombinant protein, which fuses the TNF receptor and interferes with TNF-α.
Response rate: Administration of etanercept (25 mg sc twice weekly over 3–10 months) with a cumulative response rate of 44% (improvement ≥50% in 15 patients) has been reported in case reports with 34 patients with moderate to severe HS.121-125 (Table 3). Relapses after discontinuation of treatment occurred in 10 of 14 patients (71%).
In a prospective, randomized, double-blind, placebo-controlled, cross-over study of etanercept treatment (50 mg sc twice weekly) of 20 patients with HS for 3 months no difference compared with placebo could be detected125 (Table 4).
Other biologicals
Treatment of patients with HS with ustekinumab has also been reported in case reports.126
Administration of ustekinumab (three 45 mg sc injections on weeks 0, 4 and 16) with a cumulative response rate of 33% (improvement ≥50% in 1 patient) has been reported in a case series of three patients with moderate to severe HS126 (Table 3). Relapses after discontinuation of treatment occurred in two of three patients (66%).
Retinoids
Isotretinoin
Mechanism: Isotretinoin has little or no ability to bind to cellular retinol-binding proteins or retinoic acid nuclear receptors (RARs and RXRs), but may act as a pro-drug that is converted intracellularly to at least five biologically important metabolites that are agonists for RAR and RXR. It achieves its efficacy by influencing cell-cycle progression, cellular differentiation, cell survival and apoptosis.127 The main mechanism of action in HS seems to be that isotretinoin may prevent an affected pilosebaceous unit from being occluded by ductal hypercornification.
In addition, isotretinoin has been shown to have anti-inflammatory properties.127 It might act directly due to modifying monocyte chemotaxis and exerts secondary effect with regard to antikeratinizing action and avoidance of hair follicle rupture. Reduction of sebaceous gland size and inhibition of sebaceous gland activity (responsible for the rapid clinical improvement observed in acne vulgaris) seems not to be of relevance in the treatment of HS as an absence or reduced volume of the sebaceous glands are observed in hidradenitis suppurativa.128
Pretreatment assessment: According to recommendations of the European Directive liver enzymes and lipids should be checked before treatment. Moreover, therapy management includes also medically supervised pregnancy testing directly before introduction of isotretinoin therapy and provides advice on contraception.127
Indication and contraindications: If given early enough in the treatment of HS, isotretinoin may potentially prevent an affected pilosebaceous unit from being occluded by ductal hypercornification. However, its usage in HS is often disappointing and the literature data are inconsistent. Therefore, it is recommended not to use isotretinoin in the treatment of HS.129
It is suggested that both patients and prescribers must be fully aware of teratogenicity. The patient should acknowledge the problem by signing an informed consent form and should accept detailed counseling by the clinician prior to and during treatment. The regulatory authority in each country has approved a pregnancy prevention program. This program includes advice on education, therapy management and control of the drug distribution.127
The treatment with isotretinoin should be used with caution in case of liver enzymes and lipids elevation or even avoided/stopped when these lab values are increased three and two times over the upper normal range limit, respectively. Since both retinoids and tetracyclines can cause increased intracranial pressure, their combined use is also contraindicated.
Dosage and duration of treatment: In general, the recommended dosage and duration of treatment is similar to these proposed for severe forms of acne vulgaris. In seven available studies comprising a total of 174 patients the range of daily dosages was of 0.5–1.2 mg/kg administered within the period of 4–12 months.86, 129-134 In one study, a single patient was treated initially with prednisolone and erythromycin and then maintained on long-term isotretinoin.86
Response rate: In the light of available data, the therapeutic effect of isotretinoin is questionable. Summarizing, nonresponders were assessed as 64.4% (112/174).86, 129-134 The presence of acne vulgaris or of a history of previous acne had no impact on outcome.129 The observed response (evaluated as moderate-to-significant) among the rest of the patients was mainly restricted to these with mild HS forms (Hurley I). Moreover, approximately 13% of responders relapsed within a couple of months after cessation of the treatment.86, 130-134 Several issues should be taken into account, including side-effects, poor response rate and loss of treatment motivation – physicians should be aware of the substantial drop out rate of 29.4% (20/68) reported by Boer et al.130
Follow-up investigations: Liver enzymes and lipids should be verified at 1 month after starting and 3 monthly throughout the course of the treatment. Pregnancy testing should be done monthly during the whole period of drug intake and 5 weeks after therapy cessation.130 In diabetics, retinoids can either improve or worsen glucose tolerance. Therefore, blood-sugar levels have to be verified more frequently than usual in the early stages of the treatment.
Complications: Adverse events are quite common and typical for the usage of retinoids. In available literature data on HS treatment with isotretinoin the signs of so called retinoid dermatitis (i.e. xerosis, cheilitis, xerophthalmia, etc.) occurred most often. Headache and arthralgia were also reported.86, 129-134 Tiredness, mood changes, skin fragility, nose bleeds, myalgia should also be expected.135
Acitretin/Etretinate
Mechanism: Acitretin is a metabolite of etretinate and has replaced it in the treatment of various skin disorders as it is equally effective and has a much shorter elimination half-life. The efficacy of acitretin is mainly explained by the fact of influence on the growth cycle of skin cells. Specifically, acitretin helps to normalize cell differentiation and thin the cornified layer by directly reducing the keratinocytes' rate of proliferation. It also decreases inflammation in the dermis and epidermis by inhibiting the chemotaxis of polymorphonuclear cells and the release of proinflammatory mediators by neutrophils, influencing cyclo- and lipoxygenase (affecting the metabolism of arachidonic acid), and interfering with various cytokines (inhibits the synthesis of IL-6). The cellular mechanism underlying the pharmacological effects of acitretin has not been entirely elucidated. Acitretin appears to interfere with the intracellular metabolism of natural retinoids by targeting specific nuclear receptors (retinoid receptors such as RXRs and RARs).136
Pretreatment assessment: The recommended pretreatment assessments are similar to those proposed for isotretinoin therapy.
Indication and contraindications: However, it seems reasonable to indicate acitretin usage in early HS stages (Hurley I or mild II),30 the medication could also be advocated in the chronic stages of HS with recurrent abscesses with sinus tracts (even interconnected) and/or scarring.137, 138
The contraindications are common with isotretionin.
Dosage and duration of treatment: There were a total of seven studies on acitretin/etretinate therapy presented so far, comprising 32 patients. Patients treated with acitretin received daily doses of 0.25–0.88 mg/kg and the doses for etretinate ranged from 0.35 to 1.1 mg/kg. These retinoids were administered within the period of 3–12 months (mean 9.3 ± 3.3 months). Seventeen of all 32 evaluated patients were on isotretinoin (0.3–2 mg/kg per day) before starting acitretin/etretinate therapy without any improvement.137-143
Response rate: The response rate was undoubtedly high, as 21 of 32 patients (65.6%) improved significantly, eight patients (25%) improved moderately and three patients (9.4%) did not respond to the therapy.137-143 The improvement was also seen according to the evaluation done on quality of life aspects. As reported by Matusiak et al.138 the treatment with acitretin resulted with statistically significant improvement of clinical manifestation (observed already after 1 month of therapy) was also reflected in DLQI and HSSI. The progress was maintained during the next months, resulting with reduction of the mean score after 6 months of treatment assessed as 8.2 for DLQI (baseline, 16.6 ± 7.6) and 7.2 for HSSI (baseline, 12.8 ± 4.0).
Follow-up investigations: With regard to liver enzymes, lipids and glucose blood levels in the follow-up investigations are similar to those recommended for isotretionin usage. Due to elimination half-life of approximately 50 h for acitretin, 60 h for its main metabolite (cis-acitretin), and 120 days for etretinate (clinical evidence has shown that etretinate can be formed with concurrent ingestion of acitretin and alcohol) the pregnancy testing should be done monthly during the whole period of drug intake and preferably at 1–3 monthly intervals after therapy cessation for a period of at least 2 years (3 years according to U.S. labelling).136
Complications: The most common complaints among patients treated with acitretin/etretinate were retinoid dermatitis symptoms and, among women, hair loss. Decreased night vision, alterations in lipids profile headache, loss of concentration, joint pain, buzzing in ears, depression/fatigue were also reported. 16% (5/32) of HS sufferers treated with acitretin/etretinate discontinued treatment due to side-effects.137-143
Analgesics
Nonsteroidal anti-inflammatory drugs
Mechanism: HS leads to painful eruptions which cause a high degree of morbidity.3, 17 Pain in HS has been related to shame, irritation and a greater emotional impact.17 Quality of life is clearly adversely affected. Despite the severe pain and the high morbidity related to it, HS has been essentially ignored in the pain medicine literature.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a class of drugs with analgesic and antipyretic effects. In higher doses they also demonstrate anti-inflammatory effects. They block cycloxygenase enzymes leading to reduction of prostaglandins and thus to reduction of pain and inflammation. They are classified mainly in salicylates, propionic acid derivatives, acetic acid derivatives, enolic acid derivatives, fenamic acid derivatives and coxibs. These subcategories vary in potency, duration of action and strength of inhibition of cycloxygenase-1. Besides their systemic route of administration, topical preparations also exist.
Pretreatment assessment: Pretreatment assessment should most certainly include evaluation of the drugs that are already received by the patient, especially antidepressants, warfarin and antihypertensives, since there are well-described interactions with these categories, that can potentially lead to serious adverse events. Furthermore, haematology, coagulation activity, renal and hepatic function, gastrointestinal bleeding and recent ulceration history should all be carefully evaluated.
Indications and contraindications: No clinical evidence exists on the use of NSAIDs in the amelioration of pain and inflammation in HS. Their anecdotal use in the usual dosage schemas may be justified for the amelioration of acute pain related to HS.
Contraindications include liver and renal impairment, severe heart failure, recent or active gastrointestinal bleeding and symptomatic peptic ulcer, as well as inflammatory bowel disease. Coxibs are also contraindicated in people with ischaemic heart disease, cerebrovascular disease, peripheral arterial disease and moderate or severe heart failure.
Dosage and duration of treatment: The use of NSAIDs is recommended in the usual dosage schemas for the amelioration of acute pain related to HS. It was suggested that ketoprofen topical preparations, especially the patch one, could be useful for treating inflammatory pain, since they showed potent anti-inflammatory and analgesic activity with good skin permeability.144
Taken into consideration the benefit/risk ration assessed for other NSAIDs indication, coxibs would be better to be avoided, since they are also related to a higher risk for major adverse cardiovascular events compared to the other NSAIDs.145, 146 Naproxen use may be less related to the development of major adverse cardiovascular events.146
Response rate: No clinical evidence exists at present.
Follow-up investigations: Haematology, coagulation function, ECG, renal and liver functions are crucial evaluations in follow-up visits.
Complications: Well-known side-effects, especially in the long-term use, that must be carefully assessed and monitored include renal adverse drug reactions, renal failure, liver failure, ulcers and prolonged bleeding time. Most importantly, NSAIDs, except of aspirin, increase the major adverse cardiovascular events, especially myocardial infarction and stroke, in their long-term use. NSAIDS are not proven to increase the rate of infections.
Greater understanding of the pathophysiology of HS-related pain and clinical evidence of the efficacy of treatment options available for the amelioration of this pain are needed.
Opiates
Mechanism: Opioids work by binding to opioid receptors, which are found in the central and peripheral nervous system. They reduce the intensity of pain signals reaching the brain. Their action leads to decreased perception of pain, increased pain tolerance and decreased reaction to pain. Their primary use is as painkillers. Most known and used medications that fall into this class include hydrocodone, oxycodone, morphine and codeine.
Pretreatment assessment: Pretreatment assessment should most certainly include evaluation of the drugs that are already received by the patient, especially medications that suppress the central nervous system, such as antihistamines, barbiturates and benzodiazepines. Such interactions can lead to life-threatening respiratory depression. Furthermore, haematology, renal and hepatic function must always be assessed. Special attention must be given to the respiratory capability of the patient.
Indications and contraindications: No clinical evidence exists for the use of opioids in the amelioration of pain in HS. Their use should be restricted and limited to cases where all other painkillers have failed. Codeine should be the first treatment option for this drug class. Hydrocodone may also be an option.
Contraindications include liver and renal impairment and severe pulmonary and respiratory failure.
Dosage and duration of treatment: The usual dosage schemas of codeine and hydrocodone must be given for the treatment of acute pain in HS. Their use must be reserved only for the most resistant to other therapies cases and their use should be of strictly limited time. The development of opioid dependence with ongoing administration cannot be overlooked. Physicians are highly advised to keep in mind the withdrawal syndrome with abrupt discontinuation along with the dosage and administration of opioid antagonist naloxone, in cases where life-threatening opioid-induced suppression has occurred.
Zinc gluconate
Mechanism: An alteration of innate immunity in lesional skin (TLR 2, 3, 4, 7 and 9; ICAM-1; IL-6; TNF; α-MSH; TGF-β; β-defensin 2 and 4; and IGF-1) was partially restored in 12 patients after 3 months of zinc gluconate 90 mg/day.147 A review of mechanisms involved is available in.148
Indication and contraindication: Zinc seems to be a maintenance treatment in Hurley I and II.
Dosage and duration: High dosage is used: 90 mg/day at initiation, may be lowered according to results and GI tract side effects; long term treatment.
Response rate: One study treated 22 patients (Hurley I & II) with eight complete remissions and 14 partial remissions.148
Follow-up investigations: GI tract upset very frequently leading to doses adjustment; biological follow-up of iron, the absorption of which may be impaired.
Intramuscular gamma-globulin
Mechanism: Intramuscular gamma-globulin has numerous immune-modulatory actions.149 This immunomodulation is primarily used to decrease inflammatory reactions by controlling various, mainly antibody-mediated, components of immune mechanisms.
Pretreatment assessment: Pretreatment investigations include haematology.
Indication and contraindication: There is only one report on the use of intramuscular gamma globulin in HS,150 therefore its use is currently not recommended.
Contraindications include IgA deficiency, thrombocytopaenia or other coagulation disorders.
Dosage and duration of treatment: Intramuscular human immunoglobulin was administered at a dose of 12.38 mg/kg for an unrevealed duration.150
Response rate: Four of five HS patients treated with intramuscular immunoglobulin demonstrated 50–70% improvement, it's unknown how long these patients were treated.150
Follow-up investigations: Renal function and haematology.
Complications: The most common side-effect is pain and localized erythema at the injection site. Severe but rare adverse effects include shock, anaphylaxis, deep vein thrombosis or disseminated intravascular coagulation, impaired renal function.
Colchicine
Mechanism: Colchicine inhibits microtubule polymerization inhibiting several cytokine signalling pathways.151 In gout, colchicine suppresses inflammasome-driven caspase-1 activation and IL-1β processing and release.152 Colchicine also accumulates in neutrophils,153 inhibiting neutrophil expression of cell adhesion molecules and decreasing neutrophil degranulation, chemotaxis and phagocytosis.154 Its efficacy in neutrophilic auto-inflammatory diseases is attributed to its effect on neutrophils in addition to the inhibition of the inflammasome.154
Pretreatment assessment: Pretreatment investigations include haematology, renal and hepatic function.
Indication and contraindication: The efficacy of colchicine seems poor and has therefore no place in the treatments of HS.155 Contraindications include severe liver or kidney dysfunction, haematological disorders.
Dosage and duration of treatment: In HS 0.5 mg colchicine b.i.d. orally has been studied for up to 4 months.155
Response rate: In a small prospective pilot study (n = 8) after 1 month, twoof eight patients experienced slight improvement of their symptoms whereas six of eight reported no change.155
Follow-up investigations: Haematology, renal and hepatic function should be monitored periodically.
Complications: The most frequent adverse effect is gastrointestinal disturbance. Prolonged use can result in alopecia, neuropathy, renal and hepatic dysfunction.
Experimental therapies
Botulinum toxin
Two cases are reported in which botulinum toxin (BnTx) has been found effective. In one case a 6 years old girl was treated first with topical clindamycin 15%, azeleic acid and systemic erythromycin and later isotretinoin. The girl was treated with BnTX 40 mouse units and experienced a longer remission lasting 6 months.156 In a second study a 38 years old woman was treated with BnTX type A haemagglutining complex 250 units with good effect. 157 The mechanism remains unknown.
Indication and contraindication: Indication: Experimental therapy in Hurley stage I or II HS.
Contraindication: Infection in the area to be injected. Known allergy to BnTX product used.
Relative contraindications: peripheral motoneuropathy, concommittant treatment with aminoglycosides and other drugs that affect impulse-transmission, pregnancy or breast-feeding.158
Dosage and duration of treatment: Depending on area treated, cases use 40 – 250 units.
Response rate: Only two cases with positive results described.
Follow-up investigations: Continued disease severity assessment.
Complications: Refer to information about specific product used.
Surgical therapy
Since the most common nonsurgical methods seldom result in lasting cure, surgical treatment seems to be a quite common and accepted therapeutic modality for HS. Several surgical treatment methods co-exist and can be recommended (Table 5). The type of surgery and margins are selected based on the body region and severity of the disease.
| Number of treated patients/sites/lesions | Recurrence rate | Follow-up period | Reference | |
|---|---|---|---|---|
| Deroofing | 88 lesions | 17% | Median 34 months | van der Zee et al.195 |
| Excision | 100 sites (PIH) | 69.9% | 1–7 years (median 3) | Mandal and Watson162 |
| 87 sites (SIH) | 21.4% | 1 year | Bieniek et al.196 | |
| CO2 laser | 185 sites | 1.1% | 1 to 19 years | Hazen and Hazen 182 |
| 34 patients | 11.8% | 34.5 months (range, 7–87 months) | Lapins et al.187 | |
| 24 patients | 8.3% | 27 months (range 15–47 months) | Lapins et al.185 | |
| Electro-surgery | 30 lesions | 14% | Mean of 16 days (range 15 to 21 days). | Aksakal and Adisen160 |
Conventional surgery
Excision or curettage of individual lesions
Vigorous exteriorization by repeated electrocauterization and curettage of the draining sinuses may be curative in several cases.159 Grade I–II cases are likely to benefit from the electrosurgical procedure160 (12 pts 30 lesions 86% cure short follow-up). Deroofing and secondary healing is a similar concept recently published.161 The recurrence rate of partial excision is relatively high when compared with radical excision and more complex reconstructions (100 ops, 69.88% recurrence vs. 0% 43 ops).162
Total excision of the lesions and surrounding hair-bearing skin
Instead of such limited surgical intervention most surgeons recommend complete excision of the apocrine gland bearing area delineated by the hairy surface(s) of the affected region(s).163 When opting for surgical cure today, extensive removal of the affected skin and underlying tissue is a uniform requirement, while further treatment, application of various reconstructive methods varies on a wide scale.
Radical excision is the treatment of choice for HS. As Rompel concluded in a study of 106 operations, the method of reconstruction has no influence on recurrence and should be chosen with respect to the size and location of the excised area60 (Table 6).
| Number of treated sites | Recurrence rate | Follow-up period | References | |
|---|---|---|---|---|
| SIH | 87 sites | 31.6% | 1 year | Bieniek et al.196 |
| Primary closure | 92 sites | 34% | 1–5 years | Van Rappard et al.168 |
| Grafts (immediate or delayed) | 367 sites | 33% | 1–19 years | Bohn and Svensson170 |
| 24 sites (NPWT) | 20.9% | n.d. | Chen and Friedman171 | |
| Flaps | 50 sites | 18.75% | Mean 2 years | Alharbi et al.174 |
No reconstruction (second intention healing)
Excision of the affected skin and closure by secondary healing – without reconstruction – is an option that has been practiced since decades164 and followed even today165; (142 pts/mixed dgs/success rate 89–72% at 1 year166). If secondary healing was compared to skin grafting, patients' preference was for the former method.167 The main drawback of the technique is its lengthiness due to prolonged healing.
Primary closure
Less extensive defects and certain anatomical situations allow primary closure (66% success rate 92 ops in 57 pts).168
Reconstruction with immediate or delayed skin grafting
Split thickness skin graft (STSG) coverage of the exposed area either immediately or in a delayed fashion, 10–14 days later, is an extensively accepted method. Most descriptions do not separate the modalities (good results169; 138 pts, 367 ops, 33% recurrence170).
Reconstruction with skin grafting and NPWT
Wide surgical excision and skin grafting complemented with negative pressure wound healing therapy (VAC therapy) results in better outcomes (11 pts, 24 ops 79,1% success171; 5 pts, 8 ops, 90% graft take short follow-up172).
Reconstruction with flap plasty
The use of myocutaneous flaps for reconstruction is an option for recurrent disease (good results173). Defect coverage with fasciocutaneous and musculocutaneous flaps can be carried out with an acceptable recurrence rate therefore being recommended as a reasonable alternative (81.25% success rate, 35 pts, 50 ops).174 These interventions often require the use of a stool management system or colostomy for perineal/perianal lesions.174 The use of a thoracodorsal artery perforator flap (Busnardo et al., 12 pts, 24 ops, 6 mo follow-up) may increase upper limb movement significantly (98.7 preoperatively vs. 152.7 degrees postoperatively.175)
According to a meta-analysis of 24 studies176 only one study can be categorized as grade A and 6 as grade B evidence. A prospective randomized controlled study177 compared primary closure vs. closure over collagen-gentamicin sponge, and found the use of local antibiotics beneficial, resulting in faster wound healing and fewer complications (200 pts, early compl 35% vs. 52%, but same/40 vs. 42%/recurrence rate at 3 mo). A correlation can be made between the success of the surgical intervention and its extensiveness according to a retrospective study of 31 pts (recurrence rates: drainage 100%, limited excision 42,8%, radical excision 27%).178 In perianal disease wide excision is also more successful in prevention than limited excision.179
It is very difficult to compare surgical treatment modalities for HS because of the complex nature of the disease, the numerous complicated surgical interventions widely used for treatment and the variable results reported in the literature. More comparative studies are needed to move disease status from being a disease of incapacitated patients and frustrated physicians.180
Deroofing
The deroofing technique is an effective and fast surgical technique suitable as an office procedure.161 This not expensive technique convers, with limited surgery and maximal preservation of the surrounding healthy tissue, painful recurrent lesions into cosmetically acceptable scars.161
Due to the use of the electro surgical loop good haemostasis is achieved, allowing good visualization of the operative area. The technique is especially suited for recurrent HS lesions at fixed locations in Hurley 1 or 2 areas.
For electrosurgical cutting, an Erbotom operating at 35 W, with a manually controlled hand-piece fitted with a loop was used. A hyfrecator with a sharp tip and used in the fulguration mode would probably give a comparable effect.
The created defects were left open for healing by secondary intention.
Preoperative assessment: Pre-operatively HS lesions to be deroofed are identified by visual inspection and palpation, and are marked with ink. The skin is than disinfected with 0.05 mg/ml chlorohexidine solution.
Anaesthesia: Local anaesthesia solution, lidocaine 1% (10 mg/ml) plus adrenaline 1 : 200 (5 μg/ml) is injected in an around the lesion. Lidocaine prilocaine cream can be applied 1 h before the injections.
Technique: An electrosurgical device operating at 35 W, with a manually controlled hand-piece fitted with a loop can be used. A blunt probe is inserted in sinus openings. In case openings are detectable make a small incision to introduce the probe. The lesion is then explored with the probe in all directions in order to find and explore all communicating tracts. Care should be taken not to create false passages with the probe. In case a blunt probe is not available the blunt tip of a closed, fine forceps or ‘mosquito’ could also be used as a probe. Then surgically remove the roof of the lesion using the probe as a guide. The walls are then carefully probed again for other remaining communicating sinus tracts. The gelatinous and sanguinolent material on the floor of the exposed and inflamed lesions is then scraped away with a disposable curette.
Wound healing: Second intention.
Recurrence rate: Fifteen of 88 (17%) deroofed lesions showed a recurrence, after a median of 4.6 months (interquartile range 1.2–6.2).161 Seventy three deroofed lesions (83%) did not show a recurrence after a median follow-up of 34 months (interquartile range 24–44).164
Complications: Postoperative bleeding, infection.
Carbon dioxide laser therapy
All surgical techniques to treat HS aim at radically removing all keratinocytes and remnant of keratinocytes in nodules, abscesses and fistulas. This can be done through excision en bloc of the whole or parts of an involved skin area together with the pathological process.
Scanner assisted carbon dioxide laser treatment aims at focal radical vaporization of all nodules, abscesses and fistulas, leaving healthy tissues in between the pathological lesions. The lesions are vaporized from ‘inside and out’ until surrounding healthy tissues is reached, superficially and deep. In this way the technique can be tissue sparing and at the same time radical.
Carbon dioxide laser can also be used to excise smaller or larger skin areas en bloc with or without laser coagulation of remnants (marsupialization) in the deep tissues, with less bleeding and better visualization than in standard excisions.181, 182
The method was first described in 1987.183 Sherman and Reid published their results with carbon dioxide laser treatment of 11 cases with vulvar lesions184 and later a perhaps more radical modification was introduced.185 Following, variants of carbon dioxide laser HS treatment were published.181, 186 Recently, in a RCT of 61 HS patients, it was shown that carbon dioxide laser-treatment was effective.182 In most papers, healing by secondary intention was used.
Preoperative assessment: Symptomatic lesions are selected for the treatment (i.e., those with discharge, inflammation, infiltration, or suspected abscesses). Areas that had been asymptomatic for more than 2 years but showed signs of previous activity (e.g, scars with postinflammatory hyperpigmentation, sometimes with dry pseudocomedones) but no current inflammation are usually not treated. The diseased skin is examined macroscopically for scarring, tissue distortion and discoloration, dry or suppurating sinuses, macropseudocomedones, and other superficial signs. The examination is completed by palpating the defects for bulky indurations and small, firm subcutaneous nodules or fluctuating purulent tissue. The affected area is delineated with ink.
Anaesthesia: After the skin is cleaned with 0.05 mg/ml chlorhexidine solution, the area is anaesthetized by injection of lidocaine, 0.5–1.0 mg/ml, and epinephrine. To reduce pain, we apply a lidocaine prilocaine cream for an hour to richly innervated areas, such as the groin, before the injections. The solution is injected and infiltrated around and not directly into the affected site to avoid direct contact with inflamed tissue and injection into the abscess.
Technique: A scanner assisted carbon dioxide laser is used. This is a laser with a focusing hand-piece attached to the miniature opto-mechanical flash scanner delivery system that generates a focal spot, which rapidly and homogeneously spiral scans and covers a round area on tissue at the focal plane.
The area selected is ablated with the laser beam by passing it over the tissues with repeated ablations. Devitalized tissue is removed by cleansing the surface with a swab soaked in 0.9% sodium chloride solution. The depth of the level of vaporization is controlled by the selection of power, focal length, scanner-controlled spot size and the movements of the hand-held scanner. 20 to 50 W, a spot size of 3- to 6-mm, and a focal length setting of 12.5 or 18 cm, can be used. The vaporization procedure is repeated in downward and outward directions until fresh yellow adipose tissue is exposed in the deep, relatively thin and anatomically normal skin margins laterally, with no remaining dense or discolored tissue. Usually the vaporization reached the deep subcutaneous fat or fascia. In the axillary and inguinal region, major vessels and the nerve plexus must be protected, but this depth is seldom reached in Hurley stage II lesions. The smaller blood vessels are coagulated by the laser, but bleeding from vessels larger than 0.5 to 1 mm in diameter is usually better stopped with electrocoagulation or ligation.
Wound healing: The wound, left to heal by secondary intention, is immediately covered with dry dressings or ointment-impregnated dressings and a covering bandage attached with surgical adhesive tape or gauze underwear.
The dressings are initially left on for 2 or 3 days without changing to prevent early bleeding. Thereafter, the wound is cleaned and rinsed with tap water, and the bandage is changed as often as necessary, sometimes daily, pending complete healing. A hydrofiber dressing can be used. Patients are usually able to change dressings without professional help. The wounds are inspected after 1 week and 6 weeks.
Recurrence rate: The following recurrence rates have been published following carbon dioxide laser-treatment of HS: two of 185 sites,182 two of nine patients,186 two of 24 patients185 one of seven patients,181 and four of 34 patients.187 The follow-up times varies between the different publications.
Complications: Complications following carbon dioxide laser treatment of HS are of minor importance. Secondary infection, long healing time and scarring are included.
Nd:YAG laser therapy
Based on the assumption that HS starts in the hair follicle, neodium-doped yttrium aluminum garnet laser, designed for hair removal, was tried. In the first publication, 22 patients were given monthly Nd:YAG laser treatments for 3 months.188 The second publication from the same group showed the results following treatment once a month for 4 months.189 The study was randomized and contralateral body sites were used as controls. Both laser treated and control diseased skin areas were treated with benzoyl peroxide wash 10% and clindamycin 1% gel or lotion. The scoring of lesions was blinded. Percentage average change in HS severity on overall anatomic sites was −65.3% and 72.7% after laser treatment compared to −7.5% and 22.9% for control sites.188, 189 The effects appear to maintain 2 months after the fourth laser treatment. More work is needed before Nd:YAG laser can be established as a standard treatment for HS.
Experimental therapies
IPL therapy
By reducing the number of hairs in anatomical regions with a predilection for HS to occur, it is assumed that HS-recurrences would be less likely in those regions. Intense pulsed light (IPL) is one method for hair removal. In a prospective study, 18 HS patients showed a significant improvement after IPL-treatment, where lesions on contralateral sites served as controls.190 Further studies are needed to establish the role of IPL treatment in HS.
Photodynamic therapy (PDT)
Up to now, more than 20 HS patients have received photodynamic treatment, according to the literature. The first very promising publication by Gold et al.191 was a case study of four patients who underwent 3–4 treatments of short-contact 5-aminolevulinic acid–PDT therapy using blue light for activation and a 3-month follow-up period. All patients had a total or almost total clinical improvement. In a similar case series of four patients who had a maximum of four treatments of 5-aminolevulinic acid–PDT at weekly intervals, none had significant improvement in regional HS scores observed at follow-up visits.192 More recently, two open case series with PDT for HS were published. The first, with five patients, all remained unimproved.193 The second, three patients of 12 patients complete clearance.194 More studies are needed to establish the role of PDT treatment in HS.
Therapeutic conclusion
It is recommended that HS is treated based on the subjective impact and objective severity of the disease. Locally recurring lesions can be treated surgically, whereas medical treatment either as monotherapy or in combination with surgery is more appropriate for widely spread lesions. Medical therapy may include antibiotics and immunosupressants.
A Hurley severity grade-relevant treatment of HS is recommended by the expert group following the following treatment algorithm, which exhibits similarities but also some differences with the one of the German Dermatological Society1, 102 (Fig. 1).