Pheochromocytoma: Positive predictive values of mildly elevated urinary fractionated metanephrines in a large cohort of community-dwelling patients
Abstract
The diagnostic utility of different thresholds of elevated urinary fractionated metanephrine (UFM) for pheochromocytoma-paraganglioma (PPGL) was evaluated in 10 164 community-dwelling subjects (2012-2017). Levels were ≥1.5× the upper normal limit (UNL) in 276 subjects (2.7%) and ≥2×UNL in 138 (1.4%). PPGL was subsequently diagnosed in 59 (mean age 51.9 ± 14.3, 64% female); 58 (98.3%) with UFM ≥ 2×UNL. Positive predictive values (PPV) were 42% for UFM ≥ 2×UNL, 55% for UFM ≥ 2.5×UNL, and 69% for UFM ≥ 3×UNL. The main reason for PPGL screening (52.5%) was adrenal incidentaloma. Mean (median) metanephrine/normetanephrine levels were 6.7 ± 9×UNL (3 × UNL) and 6.1 ± 8.9×UNL (2.5 × UNL). Six patients (10.2%) had an extra-adrenal tumor (one malignant paraganglioma); one had bilateral pheochromocytoma. Only one patient presented with the “classic triad” (headache, palpitations, sweating). In conclusion, after excluding obvious reasons for false-positive results, thorough diagnostic assessment for PPGL is justified in all subjects with UFM ≥ ×2UNL. The PPV of milder UFM elevations is very low.
1 INTRODUCTION
Pheochromocytoma and paraganglioma (PPGL) are tumors that arise from adrenal or extra-adrenal chromaffin cells that may secrete catecholamines.1 They may be associated with a clinical syndrome of hypertension, often extreme, and other sympathetic phenomena. Prompt diagnosis is essential, as PPGL can lead to hypertensive crisis and even death.2-4
Current guidelines recommend measurement of plasma-free metanephrines (MN) or urinary fractionated metanephrines (UFM) as the initial biochemical test for PPGL, as these tests are more sensitive than other tests of catecholamine excess.5-10 However, the rate of false positives is high because the pretest probability of PPGL is low, and the diagnostic specificity is suboptimal. Particularly high false-positive rates for urinary MN were reported in a Chinese cohort.11 Potential factors associated with false-positive results of urinary MN include the use of certain medications, particularly tricyclic antidepressants and phenoxybenzamine.12 In the absence of these medications, elevated levels of both MN and normetanephrines (NMN) to more than 3 times the upper limit of normal (UNL) and a lack of suppression of plasma metabolite levels following clonidine administration were associated with a much lower false-positive risk.1, 12 Borderline elevations of MN are frequently encountered by clinicians, and in the vast majority of these cases, the diagnosis of PPGL is refuted when long-term follow-up is performed. Therefore, it is recommended that most of these patients be followed clinically and with repeat testing to decide if imaging is required.
Data on the diagnostic utility of urine metanephrine levels in the outpatient setting are scarce. The aim of the present study was to determine the diagnostic value of different thresholds of urine MN in a large cohort of community-dwelling subjects.
2 METHODS
The study was conducted at Maccabi Health Care Services, the second largest publicly funded health maintenance organization (HMO) in Israel, insuring approximately two million residents or one-fourth of the Israeli population. It was approved by the institutional Ethics Review Board. Laboratory testing for UFM is part of the medical services “basket” covered by the Israel National Health Insurance Law, but measurement of plasma-free MN is not. Thus, practically, screening for PPGL is almost invariably performed with UFM tests.
The computerized database of Maccabi Health Care Services was reviewed for all individuals who underwent tests for 24-hour urinary catecholamines and MN from January 1, 2012, to December 31, 2017. Those for whom values of urinary metanephrines (MN) and/or normetanephrines (NMN) were higher than 1.5 times the upper normal limit (UFM > 1.5×ULN) were identified (UNL of urine metanephrine, 300 mcg/24 hours, UNL of urine NMN, 530 mcg/24 hours). For every patient, the higher result (urinary MN or NMN) was recorded as the UFM value.
In all individuals with UFM > 1.5×ULN, the following demographic and clinical data were retrieved from the medical files: sex, age at time of UFM test, reason for UFM test, clinical features at time of referral for UFM test, performance and results of imaging studies, and subsequent diagnosis of PPGL based on the pathological evaluation of a surgical specimen. The year of surgery for PPGL (2012-2017) was considered the time of diagnosis. In patients who underwent surgery, data on clinical and biochemical findings after surgery were retrieved. In patients who were not diagnosed with PPGL, the medical files were screened for the results of repeated UFM tests, potential reasons for false-positive UFM results, and further follow-up.
Urinary fractionated MN levels in 24 hour urine collection were measured by high-performance liquid chromatography (HPLC, Shimadzu) using an electrochemical detector (Bio-Rad.) Isolation of MN and NMN was performed using Bio-Rad Kit.
2.1 Statistical analysis
Categorical variables are presented as number and percentage, and continuous variables are presented as mean and standard deviation or median and range. Categorical variables were compared between groups using chi-square test, and continuous variables, using Student's t test. Analyses were generated with IBM SPSS Statistics for Windows v24.0.1 (IBM Corp., Armonk, NY). A P value of <.05 was considered statistically significant.
Positive predictive values (PPVs) for the diagnosis of PPGL were calculated from the percentage of true-positive results divided by the total true-positive plus false-positive results. PPVs were calculated for the whole cohort as well as by different threshold levels of elevated UFM.
The annual incidence of new cases of PPGL in 2012-2017 in the general population insured by Maccabi Health Care Services was calculated on the basis of the data of the Israel National Insurance Institute, which publishes the yearly number of individuals insured by each of the HMOs in Israel on a public website (https://www.btl.gov.il/Publications/ survey/Documents/seker_271.pdf).
3 RESULTS
Between January 1, 2012, and December 31, 2017, 10 164 individuals were screened for PPGL by urinary catecholamine/metanephrine levels at the Central Laboratory of Maccabi Health Care Services. The number of subjects referred for evaluation gradually increased by 48.4%, from 1421 in 2012 to 2109 in 2017. During the same years, the number of individuals insured at Maccabi Health Care Services increased by 12.1%, from 1 975 300 to 2 246 966. Thus, the number of individuals screened for PPGL increased both absolutely and relative to the total HMO-insured population.
Of the 10 164 individuals assessed for PPGL, 276 (2.7%) had UFM levels ≥1.5×UNL, including 138 (1.4%) with UFM ≥ ×2UNL. PPGL was subsequently diagnosed in 59 patients, or 0.58% of the total population of screened individuals during the study period. Of the 59 patients with PPGL, 58 (98.3%) had UFM ≥ ×2UNL, constituting 42% of all patients with UFM ≥ ×2UNL. In the remaining patient, diagnosed with a glomus tumor of the ear, UFM level was 1.5 × UNL. This patient had very high urinary level of 3 methoxytyramine (9.7 × UNL).
The calculated mean incidence of new cases of PPGL included in our cohort of the HMO-insured population in 2012-2017 was 4.7 per million per year (median 4.5, range 3-7).
3.1 Patients with pheochromocytoma
The demographic, clinical, and biochemical characteristics of the 59 patients diagnosed with PPGL are shown in Table 1. Mean age at diagnosis was 51.9 years (range 20-79). An adrenal tumor was detected in 53 patients, one bilaterally (pheochromocytoma), and an extra-adrenal tumor was detected in 6 (10.2%): retroperitoneal paraganglioma in 4 (one malignant with bone metastases) and left ear glomus tumor and paravertebral paraganglioma in one patient each.
| Characteristics | Number |
|---|---|
| Age (y), mean (SD) | 51.9 (14.5) |
| Median | 56 |
| Female, n (%) | 38 (64) |
| Tumor location, n (%) | |
| Left adrenal | 28 (47.5) |
| Right adrenal | 24 (40.7) |
| Bilateral adrenal | 1 (1.7) |
| Extra-adrenal | 6 (10.2) |
| Tumor size (mm), mean (SD) | 38 (22) |
| Median | 31 |
| Urine metanephrine (mcg/24 h), mean (SD) | 2017 (2700) |
| ×UNL | 6.7× UNL |
| Median (mcg/24 h), ×UNL | 900, 3× UNL |
| Urine normetanephrine (mcg/24h), mean (SD) | 3253 (4766) |
| ×UNL | 6.1× UNL |
| Median (mcg/24 h), ×UNL | 1318, 2.5× UNL |
Note
- UNL of urine metanephrine, 300 mcg/24 h.
- UNL of urine normetanephrine, 530 mcg/24 h.
- Abbreviations: PPGL, pheochromocytoma-paraganglioma; UNL, upper normal limit.
The reason for PPGL screening was clearly documented in the computerized files of 53 patients, of whom 31 (58.5%) were screened following the detection of an adrenal incidentaloma. There was no statistically significant difference in age, gender, and size of the adrenal mass between patients with PPGL who presented with an adrenal incidentaloma and those who were screened for other reasons (Table 2).
| Patients | Adrenal incidentaloma | Clinical suspicion | P value |
|---|---|---|---|
| N | 31 | 22 | |
| Age (y), mean ± SD | 54 ± 15 | 52 ± 14 | NS |
| Female, n (%) | 18 (30) | 18 (25) | NS |
| Max systolic blood pressure mean (mm Hg) ±SD | 139 ± 25 | 161 ± 49 | 0.05 |
| Urine metanephrine (mcg/24 h) mean ± SD | 1737 ± 2226 | 1898 ± 2383 | NS |
| ×UNL | 5.8 ± 7.4 | 6.3 ± 7.9 | |
| Urine normetanephrine (mcg/24 h) mean ± SD | 2584 ± 2987 | 4027 ± 6622 | NS |
| ×UNL | 4.9 ± 5.6 | 7.6 ± 12.5 | |
| Size of adrenal mass (mm), mean ± SD | 34 ± 18 | 38 ± 22 | NS |
Note
- UNL of urine metanephrine, 300 mcg/24 h.
- UNL of urine normetanephrine, 530 mcg/24 h.
- Abbreviations: PPGL, pheochromocytoma-paraganglioma; UNL, upper normal limit.
The performance of genetic analysis was documented in 13 patients. Mutations were identified in NF1 (neurofibromatosis type I) in four patients, in SDHD (succinate dehydrogenase D) and VHL (von Hippel–Lindau syndrome) in one patient each, and one patient was diagnosed with multiple endocrine neoplasia type 2.
The medical files recorded the presence of the classical triad of pheochromocytoma symptoms, namely headache, palpitations, and sweating, in only one patient. In 33 patients (56%), none of these symptoms was mentioned.
3.2 Patients without pheochromocytoma and UFM ≥ 2×UNL
In 80 of the 138 patients (57.2%) with UFM ≥ ×2UNL, the diagnosis of PPGL was not established. Table 3 compares the patients with UFM ≥ ×2UNL with and without PPGL. The PPGL group had a female predominance, and the non-PPGL group had a male predominance. Patients with PPGL had a significantly higher level of UFM and significantly larger adrenal mass. Hypertension was the main reason for UFM testing in the non-PPGL group; by contrast, only one-third of the patients with PPGL underwent UFM screening because of hypertension.
| Patients | Pheochromocytoma | No pheochromocytoma | P value |
|---|---|---|---|
| Number of patients | 58 | 80 | |
| Age (y), mean (SD) | 52 (12) | 57 (14) | NS |
| Female, n (%) | 38 (64%) | 24 (30%) | |
| Max systolic blood pressure (mm Hg), mean (SD) | 147 (29) | 156 (21) | NS |
| Adrenal mass size (mm), mean (SD) | 38 (22) | 19 (8) | <.001 |
| Urine metanephrine (>×UNL), mean (SD) | 7.6 (11.1) | 1(1.7) | <.001 |
| Urine normetanephrine (>×UNL), mean (SD) | 5.9 (8.9) | 3(0.9) | <.001 |
| Reason for evaluation, n (%) | |||
| Hypertension | 17 (29%) | 50 (63%) | .001 |
| Adrenal incidentaloma | 31 (53%) | 24 (30%) | |
- Abbreviation: UNL, upper normal limit.
3.3 Positive predictive values (PPVs) of different thresholds of UFM for the diagnosis of PPGL
The PPVs for the different thresholds of UFM levels for the whole cohort are shown in Table 4. Overall, the PPV for UFM ≥ ×2UNL was 42% (58/138 patients). The value increased with an increase in UFM level; UFM ≥ 2.5×UNL predicted the diagnosis of pheochromocytoma in more than 50% of the patients.
| UFM (×UNL) | Tested patients n (%)a | Patients with PPGL n (%)b | PPV (%) |
|---|---|---|---|
| ≥2 | 138 (100) | 58 (98) | 42 |
| ≥2.5 | 92 (67) | 51 (86) | 55.4 |
| ≥3 | 64 (46) | 44 (75) | 68.7 |
| ≥3.5 | 62 (45) | 42 (71) | 67.7 |
| ≥4 | 49 (36) | 42 (71) | 85.7 |
| ≥4.5 | 44 (32) | 38 (64) | 86.4 |
| ≥5 | 41 (30) | 36 (61) | 87.8 |
| ≥5.5 | 40 (29) | 36 (61) | 90 |
| ≥6 | 38 (28) | 34 (58) | 89.5 |
| ≥6.5 | 34 (25) | 30 (51) | 88.2 |
| ≥7 | 28 (20) | 27 (46) | 96.4 |
| ≥7.5 | 26 (19) | 25 (42) | 96.2 |
| ≥8 | 25 (18) | 24 (41) | 96 |
| ≥9 | 20 (14) | 19 (32) | 95 |
| ≥10 | 17 (12) | 16 (27) | 94.1 |
| ≥12 | 16 (12) | 15 (25) | 93.8 |
| ≥14 | 14 (10) | 14 (24) | 100 |
- Abbreviations: PPGL, pheochromocytoma and paraganglioma; PPV, positive predictive value; UFM, urinary fractionated metanephrines.
- a Number and percent of tested patients with different thresholds of elevated UFM, of the 138 patients with UFM ≥ ×2UNL.
- b Number and percent of patients with different thresholds of elevated UFM who were diagnosed with PPGL, of the 59 patients diagnosed with PPGL.
4 DISCUSSION
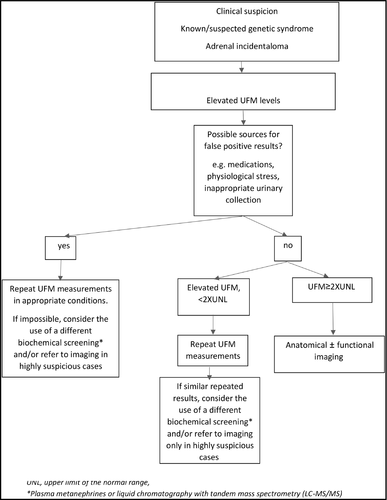
The importance of highly sensitive screening tests for PPGL is clear. However, a low level of specificity may lead to unnecessary biochemical and imaging investigations and even surgical procedures.13 Therefore, for patients with elevated values of MN, it is essential to establish a rational threshold for performing prompt thorough diagnostic investigations including anatomical and functional imaging studies. Based on the results of this study, we propose a diagnostic algorithm for the interpretation of metanephrine levels obtained during evaluation for PPGL (Figure 1).
To the best of our knowledge, this is the first analysis of the diagnostic value of elevated UFM values among community-dwelling adults in a large population-based study. The results showed that of 138 patients with UFM ≥ ×2UNL, 58 were diagnosed with PPGL, for a PPV of 42%. By contrast, only 1 of the 138 patients with UFM 1.5-2×UNL was diagnosed with PPGL. Therefore, we suggest that a finding of UFM ≥ 2UNL justifies additional biochemical and imaging studies for PPGL.
A study from China investigated the prevalence of false-positive results of 5 different tests for pheochromocytoma performed in 1896 patients with markedly elevated levels (≥2.5×ULN) of catecholamines and their metabolites who attended a large general hospital in 2000-2008.11 Fifteen patients (0.8%) had a confirmed diagnosis of PPGL. Of the 1220 patients tested for plasma or urine MN, 35 (2.9%) had elevated results; 9 of them were subsequently diagnosed with PPGL, for a PPV of 25.7%.11 In the present cohort, the number of patients who underwent PPGL screening (10 164) was more than fivefold higher than in the Chinese cohort. Although we used a lower threshold of UFM levels of ≥×2UNL, the PPV for a diagnosis of PPGL was considerably higher (42.8%). Applying the Chinese threshold of UFM ≥ 2.5×ULN to our data would yield a PPV of 56.5% (51 patients with PPGL out of 92 with UFM ≥ 2.5×ULN). However, 7 of the 59 patients with UFM 2-2.4×ULN who were subsequently diagnosed with PPGL (11.9%) would have been missed.
A possible reason for the better predictive value of elevated UFM in our cohort than in the Chinese cohort is the different study setting. Our study was conducted in community-dwelling adults whereas the Chinese study was conducted in hospital-referred patients. The physiological and psychological stress associated with excessive catecholamine production in the hospital setting might have led to more frequent false positives on screening tests for PPGL in the Chinese cohort.
The present study was performed at Maccabi Health Care Services, the second largest HMO in Israel. As the number of individuals insured by the HMO is published annually in the official website of the National Insurance Institution, we were able to calculate the incidence of PPGL in the HMO-insured population at 4.7 new patients per million per year. However, this is certainly an underestimation, as we missed patients diagnosed with PPGL by other methods, such as measurement of plasma MN or pathological examination of adrenal specimens. It is also possible that some patients diagnosed with PPGL during the study period had only mild elevations of UFM of <1.5×UNL. Furthermore, it has been estimated that at least 25% of all individuals with a pheochromocytoma were never diagnosed during life.2 In an older series, 50% of pheochromocytomas were diagnosed at autopsy.14
Owing to the rarity of the disease, large-scale studies of the incidence of PPGL are scarce. A 1983 study from Rochester, Minnesota, reported an annual incidence of ∼0.8 per 100 000 person-years. However, the calculation was based on only 11 cases of pheochromocytoma that were diagnosed in this population during a 30-year period (1950-1979), including 5 diagnosed at autopsy.15
Large health care databases are a valuable source for epidemiological research of rare diseases, provided the diagnoses are valid. Yet, it has been shown that the diagnostic codes for rare diseases are frequently inaccurate and might have a low PPV for the final diagnosis. In a recent study that sought to validate diagnostic codes of individuals registered with pheochromocytoma or catecholamine hypersecretion in Denmark in 1977-2016, the PPV of the Danish National Patient Registry codes was only 21.7%.16 Only after applying algorithms to identify cases of confirmed PPGL based on a combination of three different national registries (total 588 patients with PPGL) did the authors achieve a much higher validity of 93.1%.16 Their study period encompassed 40 years with an average population of 5.3 million inhabitants, for a mean incidence of 2.77 new cases of PPGL per million per year. The higher incidence found in the present study (4.7 new cases per million per year) is attributable to the completely different methodology we used to identify patients. In contrast with the Danish study, we did not have to rely on accurate reportage and coding of PPGL by the participating physicians.
The most common reason for PPGL screening in our cohort was the detection of an adrenal incidentaloma, in 31/59 patients (52.5%). This finding is compatible with previous series showing a frequent incidental discovery of pheochromocytoma. Three studies of patients operated for pheochromocytoma from 1990 to 2011 reported rates of adrenal incidentaloma at presentation ranging from 33% to 49%.17-19 In a German cohort of 201 patients diagnosed between 1973 and 2007, nearly 30% had an incidentally discovered pheochromocytoma.20 Furthermore, the authors found that before the introduction of CT scans to clinical routine in 1989, the rate of incidentally discovered pheochromocytomas was much lower, <10%.20 A temporal increase in the rate of diagnosis of PPGL after detection of an adrenal incidentaloma was also reported in a French study of 192 patients evaluated from 1975 to 2003. In the last quartile of this period, 25% of cases of pheochromocytoma presented as incidentaloma.21 This finding, too, was probably associated with the increasing use of imaging studies. Accordingly, a recent Swedish study of 92 patients diagnosed in 2005-2016 reported that 64% presented with an adrenal incidentaloma.22 This high rate together with our finding that most community-dwelling patients diagnosed with PPGL in the last 6 years presented with an incidentaloma can be viewed as a continuation of the aforementioned temporal changes.20, 21 Furthermore, the high proportion of adrenal incidentaloma may explain the low rate of bilateral PPGL (only one patient in both the Swedish and present series) and the relatively old age at diagnosis (56.3 ± 16.1 and 51.9 ± 14.3 years in the Swedish and our cohort, respectively). In earlier cohorts, with a lower percentage of adrenal incidentalomas, patients were diagnosed in the fifth decade.17, 21 This is in line with studies showing an increase in the frequency of adrenal incidentaloma with age.23-26
In the 80/138 patients (58%) in the present study with UFM levels >×2UNL and a false-positive diagnosis, the most common reason for PPGL screening was hypertension (approximately 60% of cases). The diagnostic cutoffs for most 24-hour UFM assays are based on normal ranges derived from a normotensive volunteer reference group. It has been shown that in individuals who are tested for pheochromocytoma but do not have the neoplasm, UFM levels are significantly higher than in normal volunteers, and this can result in a high rate of false positives.27
4.1 Strengths and limitations
The strengths of the present study are the inclusion of a relatively large number of consecutive patients with PPGL diagnosed during a recent 6-year period and the availability of detailed clinical and laboratory data. Temporal trends in the features of PPGL have been reported,20, 21 such that modern cohorts like the present one might contribute to current knowledge on pheochromocytoma. We analyzed data in a large cohort of community-dwelling patients screened for PPGL, apparently for the first time. Most previous studies focused on patients who underwent surgery for PPGL in tertiary centers, which poses potential risks of referral bias and substantial loss to follow-up.17-22
One limitation of our study was the retrospective design and its associated risk of missing data. In addition, our cohort was not fully representative of all patients diagnosed with PPGL in the study years. Finally, UFM was measured with HPLC. In a previous study, use of a tandem mass spectrometry assay to measure 24-hour UFM was found to have 97% sensitivity and 91% specificity for the diagnosis of pheochromocytoma.27 However, only a limited number of institutions worldwide have access to liquid chromatography-tandem mass spectrometry (LC-MS/MS) technology.
In conclusion, in community-dwelling patients screened for catecholamine excess, a measurement of UFM ≥×2UNL has a high PPV for PPGL. Once obvious potential reasons for a false-positive result are excluded, a finding of UFM ≥×2UNL justifies prompt clinical, laboratory, and imaging investigations. The incidence of PPGL diagnosed by UFM level ≥×1.5UNL is 4.7 new patients per million per year. Our study confirms that currently, the most common presentation of PPGL is adrenal incidentaloma, and the diagnosis of PPGL based on the classical triad of symptoms is rare.
CONFLICT OF INTEREST
The authors report no specific funding in relation to this research and no conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
“Pheochromocytoma: positive predictive values of mildly elevated urinary fractionated metanephrines in a large cohort of community-dwelling patients”. Dania Hirsch: study design, data collection, data analysis, and writing of manuscript. Alon Grossman: study design, data collection, data analysis, and writing of manuscript. Varda Nadler: Data interpretation and approval of draft. Sandra Alboim: Data interpretation and approval of draft. Gloria Tsvetov: study design, data collection, data analysis, and writing of manuscript.




