A meta-analysis of the distance between lead-implanted site and tricuspid valve annulus with postoperative tricuspid regurgitation deterioration in patients with left bundle branch area pacing
Disclosures: None
Abstract
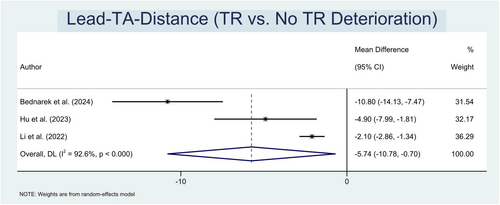
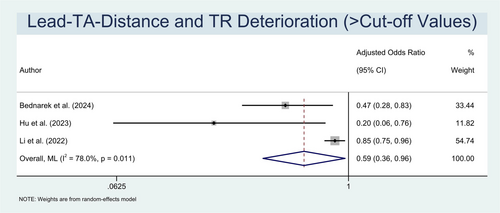
Tricuspid regurgitation (TR) is a known complication of cardiac implantable electrical devices (CIEDs), with prevalences ranging from 10% to as high as 30%. Despite left bundle branch area pacing (LBBAP) has emerged as an alternative to the limits of His-bundle pacing (HBP), the long-term safety of this procedure, notably the worsening of TR after implantation, has yet to be thoroughly investigated. This meta-analysis sought to determine the frequency of post-LBBAP TR deterioration and identify the predictors, particularly the distance between lead-implanted site and the tricuspid valve annulus (lead-TA-distance). A systematic literature search was conducted using PubMed, Europe PMC, and ScienceDirect for studies that reported the incidence of deterioration and measurement of TR grade at baseline and follow-up following LBBAP, in addition to the differences in exposure between short and long lead-TA-distances. A total of three studies involving 480 participants were included in this meta-analysis. The incidence of TR deterioration was 22%. Patients with TR deterioration also demonstrated a significantly shorter lead-TA-distance in comparison to the opposing group (MD: −5.74 mm (−0.70, −10.78); p < .001; I2 = 92.6%). The pooled results of three comparative studies suggest that participants in the longer lead-TA-distance group had a significant decrement in the likelihood of TR worsening (adjusted OR = 0.59 (0.36–0.96); p = .034; I2 = 79%). Multivariate analysis conducted in each of the included investigations supported the independence of the connection between lead-TA-distance and TR deterioration. A shorter lead-TA-distance was an independent risk factor for TR deterioration in individuals with post-LBBAP implantation.
1 INTRODUCTION
Conduction system pacing (CSP), commonly referred to as His-bundle pacing (HBP) and left bundle branch area pacing (LBBAP), is an emerging method of pacing that has garnered significant attention in recent years for providing a more physiological alternative to conventional right ventricular pacing (RVP).1, 2 LBBAP has emerged as a revered alternative to HBP implantation due to its broader zone, less reported ventricular undersensing, and lower, more stable threshold resulting from its pacing site in the myocardial septal tissue, which eventually enhances device longevity. In light of its novelty, reports on the long-term safety of this procedure have yet to be extensively investigated.3-5 The application of this technique was only implemented recently into practice, and there is currently no forthcoming registry explicitly investigating this particular area of concern.
Tricuspid regurgitation (TR) is a known complication of cardiac implantable electrical devices (CIEDs). A theoretical risk exists for TR or worsening TR with LBBAP, as the placement of an LBBAP lead is more proximal in the septum compared to RVP. This is due to the lead passing through the tricuspid septal valve leaflet and being secured into the septum close to the valve annulus.6-8 Still, in fundamental nature, the risk of lead-related TR in patients with LBBAP is expected to be lower than that in patients with RVP, attributed to the thinner pacing leads and a more physiological pacing effect. In contrast, RVP may result in right ventricle (RV) systolic dysfunction stemming from mechanical dyssynchrony in the RV, enlargement of the RV, and RV dysfunction. The movement of the tricuspid leaflet is hindered by these factors, leading to a greater incidence of TR in comparison to LBBAP.9, 10 Nevertheless, postoperative TR deterioration complications in LBBAP have been documented in various studies, with reported rates varying from 7.3% to as high as 32.6%.11
Despite investigations have been conducted to assess the occurrence of postoperative worsening TR, there is still a lack of consensus on the proper medical management regarding these patients. Whether lead removal will affect the grade of TR or, most likely, lead adhesion to the leaflet or tricuspid annular dilatation owing to TR-induced right ventricle remodelling may cause lasting damage that may not resolve even after lead removal.12, 13 Therefore, it is important to prioritize prevention over treatment and thoroughly investigate any risk factors that may worsen TR. The lead-implanted location is currently determined by the electrophysiologist's preference and experience, as there is no specific reference range provided.3, 14, 15 In this study, we aimed to characterize the incidence of post-LBBAP TR deterioration and identify its predicting factors, specifically the distance between lead-implanted site and tricuspid valve annulus (lead-TA-distance).
2 METHODS
2.1 Protocol and registration
This systematic review was conducted in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).16 The protocol was registered at the International Prospective Register of Systematic Reviews (PROSPERO), under identification number CRD42024547579.
2.2 Search strategy
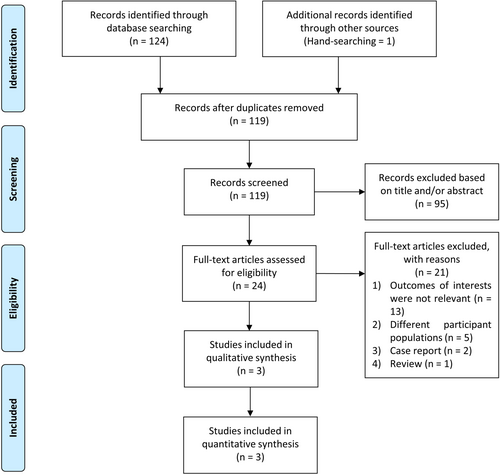
Electronic databases, including PubMed, Europe PMC, and ScienceDirect were searched by two independent investigators from inception to June 9, 2024. The search query encompasses keywords and search phrases that involve (tricuspid valve insufficiency [MeSH term]) AND (left bundle branch area pacing OR conduction system pacing). We utilized the least number of keywords necessary to optimize the initial area of inquiry and maximize the number of articles recorded. To expand our search results, we additionally conducted hand searches through the references of the included articles. The PRISMA criteria were implemented in our search, and Figure 1 depicts the search and screening processes.
2.3 Study selection
This meta-analysis focused on studies that investigated the lead-TA-distance and its correlation with TR deterioration in patients receiving LBBAP. The detailed inclusion criteria were outlined as follows: (1) prospective or retrospective observational studies; (2) patients aged 18 and older who successfully underwent LBBAP implantation for bradycardia, in accordance with the published recommendations available at the period of which the study was conducted, and had complete follow-up; (3) studies that reported the incidence of deterioration and quantification of TR grade before and after LBBAP; (4) studies that compared the short and long lead-TA-distance, defined as a value exceeding cut-off point reported within each study. Our investigation required the inclusion of studies that provided risk estimation data with 95% confidence intervals (CI), or alternatively, studies that presented sufficient data to calculate the effect size.
We excluded trials that involved patients who: (1) received triple chamber pacemaker implantation; (2) were switched to conventional RVP or LBBAP-optimized cardiac resynchronization therapy (CRT) during the follow-up period; (3) had any degree of tricuspid stenosis determined by echocardiography before the implantation or any history of tricuspid valve surgery (either before the implantation or during follow-up); and (4) had any history of congenital heart disease, defined as a condition characterized by abnormal development of the heart or blood arteries around the heart during fetal development. Conditions that may contribute to TR include Ebstein anomaly, congenital tricuspid valve dysplasia, and various congenital heart defects such as atrioventricular septal defect (AVSD) or pulmonary stenosis accompanied by ventricular septal defect (VSD). TR may also arise from annular dilatation resulting from right ventricular volume overload, such as in cases of atrial septal defect or pulmonary regurgitation.17, 18 Our meta-analysis also excluded review papers, editorials, comments, case reports/series, meta-analyses, and conference abstracts.
2.4 LBBAP implantation procedure
The LBBAP implantations were performed using the transseptal approach, adhering to the periodically available published recommendations.11, 19, 20 Concisely, a lumenless lead (model 3830, Medtronic) was introduced on the right side of the interventricular septum (IVS) using a delivery catheter in the right anterior oblique (RAO) 30° fluoroscopic view. Intermittent pacing at 2 V/0.5 ms allowed for precise real-time monitoring of the electrocardiogram (ECG) and intracardiac electrogram (EGM), which guided the implantation process. The lead will then be inserted perpendicularly into the IVS and routed to the left, reaching the left bundle branch region. Advancing the lead while monitoring the paced QRS morphology was necessary until the indicators for successful LBBAP were achieved.
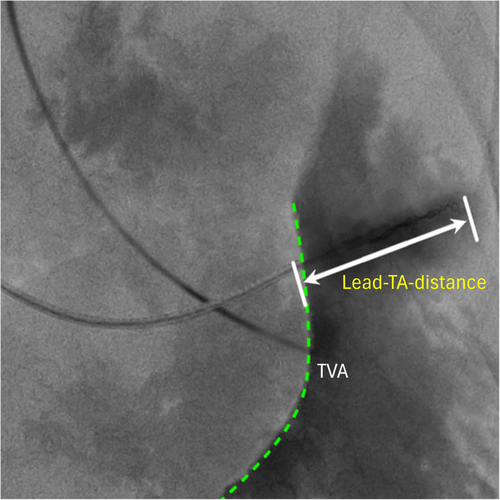
2.5 Echocardiographic evaluation
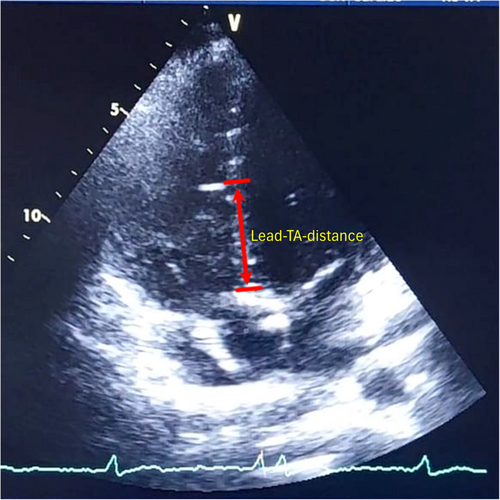
The American Society of Echocardiography criteria were used to estimate the severity of TR by employing two-dimensional (2D) echocardiography. The classification of TR was determined using a comprehensive method that considered several factors specified in the current recommendations. TR was classified as none/trivial, mild (grade 0/1 subgroup), moderate, or severe (grade 2/3 subgroup). The lead-TA-distance was measured at the ventricular end-diastolic phase using standard apical four-chamber views (Figure 2). The Bi-plane Simpson method was employed to calculate the left ventricular ejection fraction (LVEF). Our main objective was to determine the occurrence of TR deterioration during the most recent follow-up, which was defined as an increase in TR severity by at least one grade.21
2.6 Data extraction and risk of bias assessment
Two independent reviewers extracted the data from the eligible studies, consisting of (1) baseline characteristics, such as first author's name, the country in which the study was conducted, study design, total participants, age, male sex, comorbidities; (2) outcome-related data, including pacing indications, baseline LVEF, baseline TR, lead-TA-distance cut-off value, implantation procedure, and follow-up duration. Data extraction was conducted through mutual agreement, with any disputes resolved by a third researcher. If multiple follow-up times were documented in the research, the longest period was selected for analysis.
The Newcastle–Ottawa Scale (NOS) was implemented by the authors to independently assess the possibility of bias in each study. A study with a total score of seven or above was deemed bias-free. Research with a total score of six or less was deemed biased and thus excluded from the research. Author discussion was utilized to settle quality rating disagreements.22
2.7 Statistical analysis
The statistical analyses were conducted using STATA (Software for Statistics and Data Science) software version 17.0. The effect size in the current analysis was calculated as odds ratio (OR) with 95% confidence intervals (CI), while mean difference (MD) was used to estimate the comparison of continuous variables as an effect unit. Values presented using the median (interquartile range) were transformed into mean ± standard deviation (SD) for the purpose of statistical analysis.23 The studies that utilized hazard ratio (HR) to calculate effect size were also transformed into OR for the analysis. We employed random-effects models along with the restricted maximum-likelihood method to calculate the overall effect size, irrespective of the heterogeneity status.16 We utilized a meta-analysis of proportion to quantify the incidence of each event relative to the total. The I2 index was used to examine inter-study heterogeneity, with an I2 statistic of more than 50% or a p value less than 0.10 disclosed significant heterogeneity.24 Furthermore, the Egger test was utilized to quantify the publication bias. All statistical analyses were two-sided, with statistical significance attained by a p value < .05.16
3 RESULTS
3.1 Study selection, baseline, and clinical characteristics
The primary search results yielded 125 articles. Following the evaluation of the titles and abstracts, 24 papers were identified for further assessment based on the specified inclusion criteria. Eventually, three prospective observational studies with a total of 480 participants were included in our analysis.3, 14, 15 Figure 1 depicts the results of the literature search, including the basis for excluding certain publications. Table 1 presents the baseline and clinical characteristics of the studies included in the final review.
| No. | Author (year) | Country | Study design | Total participants | Age (years) | Male (%) | Pacing indications (%) | Comorbidities (%) | Baseline LVEF (%) | Baseline TR proportion (%) | Lead-TA-distance cut-off (mm) | Implantation procedure | Follow-up length | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bednarek et al.14 | Poland | Prospective, single-center observational study | 122 (17 vs. 105) | 80.2 ± 5.6 vs. 77.9 ± 12 | 41.2 vs. 52.4 | SND: 23.8AVB: 52.5HFrEF: 23.8 | Hypertension: 76.5 vs. 87.6 | 52.5 ± 9.7 vs. 50.4 ± 13.5 | Grade 0/1: 33.6 | <24.5 vs. ≥24.5 | Technique: Adhered to EHRA consensus recommendations11 | 21 months | 9 |
| Diabetes mellitus: 41.2 vs. 37.1 CAD: 29.4 vs. 39 | Grade 2/3: 66.4 | Lead: Lumenless lead (model 3830, Medtronic USA) | ||||||||||||
| AF: 35.3 vs. 19 Cardiomyopathy: 52.9 vs. 41.9 | Criteria used for confirmation of LBBAP: Adhered to EHRA consensus recommendations11 | |||||||||||||
| 2 | Hu et al.15 | China | Prospective, single-center observational study | 89 (29 vs. 60) | 63.8 ± 15.1 vs. 62.4 ± 14.7 | 27.6 vs. 48.3 | SND: 55.2 vs. 33.3AVB: 41.4 vs. 61.7 | Hypertension: 55.2 vs. 31.7 Diabetes mellitus: 34.5 vs. 15 | 63.1 ± 2.9 vs. 61.7 ± 3 | Grade 0/1: 65.2 | ≤16.1 vs. >16.1 | Technique: Chen et al.19 Lead: Lumenless lead (model 3830, Medtronic USA) | 19 ± 6.5 months | 9 |
| AF or flutter with bradycardia: 3.4 versus 5 | CAD: 65.5 vs. 51.7 | Grade 2/3: 34.8 | Criteria used for confirmation of LBBAP: Chen et al.19 | |||||||||||
| 3 | Li et al.3 | China | Prospective, single-center observational study | 269 (58 vs. 211) | NR | NR | NR | NR | NR | 42.5 (severity grade not specified) | ≤19 vs. >19 | Technique: Li et al.20 | 24 months | 8 |
| Lead: Lumenless lead (model 3830, Medtronic USA) | ||||||||||||||
| Criteria used for confirmation of LBBAP: Li et al.20 |
- Abbreviations: AF, atrial fibrillation; AVB, atrioventricular block; CAD, coronary artery disease; EHRA, European Heart Rhythm Association; HFrEF, heart failure with reduced ejection fraction; LBBAP, left bundle branch area pacing; NOS, Newcastle–Ottawa Scale; NR, not reported; SND, sinus node dysfunction; TR, tricuspid regurgitation; USA, United States of America.
Atrioventricular block (AVB) was the primary indication for treatment in 46.9% of cases, while sinus node dysfunction (SND) represented 39.5% of cases in which LBBAP was employed. The mean age of participants in both groups was notably similar (72 ± 10.4 vs. 70.2 ± 13.4 years old), with 42.4% being male. Two of three investigations reported a comparable mean proportion of baseline TR severity in both subgroups (grade 0/1: 49.4%; grade 2/3: 50.6%).14, 15 The mean duration of follow-up was nearly 2 years (21.3 months). Comorbidities associated with TR worsening were prevalent in both groups, as presented in Table 1. Diverse lead-TA-distance cut-off values were also acknowledged across the included research, ranging from 16.1 to 24.5 mm (mean: 19.9 mm).
3.2 Lead-TA-distance and TR deterioration
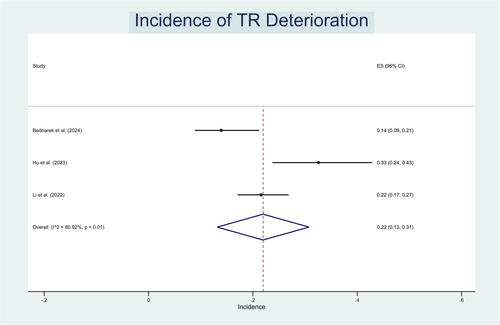
TR deterioration was observed in 22% (13%–31%; I2 = 80.9%; p < .001) of study population (Figure 3). Patients experiencing TR deterioration had a considerably shorter lead-TA-distance compared to the opposite group (MD: −5.74 mm (−0.70, −10.78); p < .001; I2 = 92.6%) (Figure 4). In addition, the pooled results from three comparative studies suggest that subjects within the longer lead-TA-distance group had a significant decrease in the risk of TR worsening (adjusted OR = 0.59 (0.36–0.96); p = .034; I2 = 79%) (Figure 5). One study reported that the deterioration of TR was mainly observed in individuals classified as grade 0/1.15 The likelihood of TR deterioration was not markedly altered by age, male sex, hypertension, diabetes mellitus, coronary artery disease, atrial tachyarrhythmias, ventricular pacing percentage, as all of the included studies adjusted for several of these confounding variables.
3.3 Publication bias
We were unable to conduct a qualitative analysis of funnel plots to identify publication bias due to a paucity of research in our analysis. Hence, the Egger test was used to quantitatively detect publication bias, and our findings revealed the absence of a small study effect.
4 DISCUSSION
To the best of our knowledge, no other meta-analysis has conducted a thorough lead position parameters analysis, particularly lead-TA-distance, to predict the likelihood of TR deterioration in patients experiencing LBBAP. Our investigation discovered that up to 22% of patients receiving LBBAP presented worsening TR, which is greater than the proportion reported in numerous similar observational studies. This could be attributed to the short follow-up duration, with observations extending for only up to a year.6-8 It is expected that the interference with tricuspid valve closure by the electrode in RVP research would only become apparent after a year of follow-up.25, 26 The extended follow-up period of the studies included in our meta-analysis observed that TR deterioration post-LBBAP is not as infrequent as it may seem, since current evidence suggests that TR is associated with a number of detrimental consequences, including lower survival rates and an increased likelihood of long-term mortality.27, 28 It is critical to recognize patients who are at risk of TR deterioration to anticipate and mitigate this condition through prompt identification.
The phenomenon known as pacemaker lead-mediated TR was initially documented in a 1969 paper by Nachnani et al.,29 who reported a patient exhibiting a TR murmur following an RVP procedure. The murmur notably diminished after the removal of the pacemaker lead. Commencing from this fundamental insight, the specific mechanism of lead-related TR deterioration in LBBAP patients is still unclear. However, similar to conventional RVP, the LBBAP electrode has the potential to breach the tricuspid valve, thereby potentiating the risk of TR. Nonetheless, the risk of lead-related TR in patients with LBBAP should be lower than those with RVP, due to smaller pacing leads and better coordination of myocardial contraction.30
A shorter lead-TA-distance (with the lead positioned closer to the tricuspid annulus) heightened the possibility of mechanical interference between the lead and the tricuspid valve or subvalvular apparatus, resulting in impairment and incompetence of valve function, as evidenced by our findings. Lead implantation significantly impacts valve function, encompassing both pacing-induced electrical and mechanical alterations; although additional investigation is required to validate this issue.14, 15 Previous RVP investigations have identified several factors, including advanced age, male sex, hypertension, diabetes mellitus, coronary artery disease, and atrial tachyarrhythmias, that may contribute to the deterioration of TR.10, 31-33 Fortunately, most of the included trials accounted for these factors and focused solely on adjusted OR, enabling us to fairly infer that the lead-TA-distance was independently correlated with TR deterioration, thereby minimizing confounding bias. From a clinical standpoint, one investigation15 identified that the TR degradation was primarily derived from the grade 0/1 category. Consequently, preventing TR deterioration in individuals with adequately functioning valves before implantation seemed to be more advantageous, further highlighting the crucial importance of early identification.
Before the present time, the optimal distance between the lead-implanted site and the tricuspid valve annulus remained in dispute. LBBAP is often located on the right side of the IVS, situated around 10–20 mm from the septal leaflet of the tricuspid annulus. Our meta-analysis revealed a multitude of lead-TA-distance cut-off values across the studies included, spanning from 16.1 to 24.5 mm, with a mean of 19.9 mm. According to this finding, identifying a lead-implanted spot with a lead-TA-distance of at least approximately 20 mm through fluoroscopy in regular clinical practice may help reduce the risk of TR deterioration in the near future.
Several studies indicate that CSP, particularly LBBAP, has demonstrated superior outcomes in preserving left ventricular function as compared to RVP.34 However, the long-term effect of LBBAP on RV function has not been comprehensively evaluated, and there is a lack of research, particularly those that focus on TR deterioration. To the best of our knowledge, only two studies14, 35 have evaluated RV function following LBBAP implantation. Nonetheless, the study done by Bednarek et al.14 was the sole investigation to address the debates regarding the deterioration of TR in relation to right cardiac function.
The long-term influence of TR following device implementation on clinical and functional outcomes is still disputed, yet numerous prior clinical investigations have discovered that considerable TR at discharge postimplantation predicted the incidence of right heart failure.36, 37 It is important to note that LBBAP typically presents with a right bundle branch block (RBBB) pacing pattern, indicating modified activation and possibly, contraction of the RV.38 The relationship between the RBBB pattern and postimplantation TR in terms of their impact on the decrease in RV function remains ambiguous. Nonetheless, Bednarek et al. indicate that there are no notable differences in echocardiographic RV-free wall strain during follow-up between TR and no TR-deterioration groups.14 Still, it underscores the importance of conducting additional, long-term prospective observational studies to validate these findings.
The management of lead-induced TR must be tailored to the specific underlying cause, as the etiology of this condition may be categorized into mechanical and functional processes.39 This is supported by the research conducted by Bednarek et al.,14 which demonstrates that an increase in LVEF is an independent predictor of improved RV function. This aligns with the ventricular interdependence hypothesis, which demonstrates that the left ventricle (LV) and RV are intricately connected in a closed-loop circuit.40 This is of great interest since, as mentioned in the preceding paragraph, Hu et al.15 discovered that the majority of the worsening in TR occurred within the grade 0/1 category. The study also found statistically significant differences in lead-TA-distance outcomes, suggesting that mechanical pathomechanisms played a more significant role. In the grade 2/3 category, on the other hand, it is evident that there is no statistically significant difference in the lead-TA-distance. The fact that the grade 2/3 group had a lower LVEF than the 0/1 group supports the notion that functional pathomechanisms may play a greater role in this group. Therefore, managing functional TR necessitates addressing the core fundamental causes associated with it.
Given the mechanical mechanisms of lead-induced TR (e.g., perforation of the tricuspid valve (TV) leaflet and lead impingement with the TV leaflets), TV repair is often advised, as the TR severity is linked to a higher mortality rate.41, 42 The current success rate of TV repair is notably high, with a relatively low recurrence rate, due to advancements in cardiovascular imaging and interventional technologies.43 Nevertheless, there is a scarcity of information regarding the surgical treatment of lead-related TR patients. Lead-related TR in RVP is the primary focus of the preponderance of studies.44, 45 Therefore, it is essential to conduct additional long-term investigations into the effects of TR from LBBAP, particularly on clinically significant TR, and to determine the most appropriate treatment for this condition.
The discussion of valve anomalies in the heart was inherently linked to the topic of echocardiography. Echocardiography is now routinely employed in a variety of electrophysiology procedures, particularly as a tool to assist in the insertion of pacemaker leads. Fluoroscopic visualization can be utilized to locate the tricuspid valve annulus (TVA) and improve the placement of leads. This allows for the measurement of the lead-TA-distance, which may help avoid the worsening of TR following the implantation procedure (Figure 6). Echocardiography, in comparison to fluoroscopy, offers more precise measurements of the lead-TA-distance.46 Thus, we propose that echocardiography should be relied on in the future to assist adequate LBBAP implantation.
4.1 Limitations
Several limitations still warrant consideration in this meta-analysis. First, significant heterogeneity was discovered in the analysis as a result of various cut-off values utilized across the studies. Second, we were unable to conduct meta-analyses on other lead position parameters (e.g., lead depth in IVS, IVS thickness) due to a paucity of research. Third, none of the papers included in our meta-analysis mentioned the specific site of LBBAP. Hence, we were unable to conduct a subgroup analysis of the effect of several LBBAP sites on TR incidence. Fourth, the limited amount of data provided in the research prevents us from doing a comprehensive diagnostic-test accuracy meta-analysis to strengthen the veracity of the study. Limitations also include a small number of studies and the lack of randomized controlled trial available. Our study adds to the body of knowledge of a topic that is gaining traction, since LBBAP is a relatively emerging technique and investigations in terms of outcome have only recently begun.
5 CONCLUSION
TR deterioration was a frequent complication following LBBAP implantation. Shorter lead-TA-distance was an independent predictor of TR deterioration and had a high predictive value in individuals with post-LBBAP TR deterioration. Given this prognostic finding, we would recommend routine echocardiographic assessment of TR and lead-TA-distance post-procedure. Further long-term research is still of great interest to better understand the effects of lead-TA-distance on tricuspid valve function and how post-LBBAP TR deterioration affects right heart function.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.