Longterm follow-up of children with traumatic optic nerve avulsion
Abstract.
Purpose: We report the longterm follow-up of children with optic nerve avulsion (ONA) caused by traumatic events. The remarkable differences in courses and outcomes may elucidate the spectrum of ONA-associated symptoms and injuries.
Methods: During the last 15 years, three children with ONA were referred to our department. These cases are presented with special attention to their longterm follow-up.
Results: Two patients suffered from complete ONA after head injury. The third patient presented with partial ONA caused by a bicycle accident. Longterm follow-up varied between 7 and 15 years. In the first patient, a pale swollen retina without any visible retinal vasculature was observed early in the course of follow-up. The retina later completely detached. In the second patient, extended fibroglial scarring occurred and an extremely large epiretinal membrane formed and was finally released spontaneously into the vitreous. The third patient developed only mild fibroglial scarring and retinal pigment epithelium hyperplasia. The optic nerve head in this patient came to resemble a morning glory disc.
Conclusions: Optic nerve avulsion can adopt different courses and outcomes in different patients. Final visual outcome seems to depend on the degree of visual acuity immediately after injury. Substantial intraocular architecture changes can occur as a result of ONA.
Introduction
Worldwide, ocular trauma is an important cause of visual loss in children (MacEwen et al. 1999; Serrano et al. 2003; Beby et al. 2006). In the USA, a population-based study found an annual incidence of ocular trauma in children of 15.2/100 000 (Strahlmann et al. 1990). In general, males are more often affected than females (Takvam & Midelfart 1993; Serrano et al. 2003; Saunte & Saunte 2008).
Optic nerve avulsion (ONA) is an uncommon presentation of ocular trauma and has been infrequently reported since its first description in 1856 (Buchwald et al. 2003).
The optic nerve contains more than 1 000 000 retinal ganglion axons. It exits the globe at the optic nerve head (ONH) surrounded by pial and dural sheaths. A complete avulsion of the optic nerve implies that the optic nerve fibres are disinserted from the retina, choroid and vitreous and that the lamina cribrosa is retracted from the scleral rim (Salzmann 1903). In fact, histopathology of enucleated eyes has revealed the absence of optic nerve fibres from the lamina cribrosa (Chaudhry et al. 2006).
Optic nerve avulsion typically results from blunt injury to the orbit, concussion of the globe or massive trauma to the face (Anand et al. 2003). Common causes are accidents with motor vehicles and bicycles, stick injuries and falls (Steinsapir & Goldberg 1994; Buchwald et al. 2001, 2003). An increasing number of reports have been published about incidents of ONA caused by accidents with work tools and sporting injuries (Steinsapir & Goldberg 1994; Anand et al. 2003; Sawhney et al. 2003). In addition, ONA caused by door handles in children has recently been reported (Chaudhry et al. 2005, 2006). Even gun shots can lead to ONA (Salzmann 1903; Daxecker 1980; Buchwald et al. 2003). Optic nerve avulsion can occur completely or partially. It can be associated with other injury-related pathologies, such as limitations of ocular movement (Foster et al. 1997; Simsek et al. 2006), and ptosis and abnormalities of the retinal vasculature (Kline et al. 1988; Noro et al. 1990).
The mechanisms of ONA are not yet completely understood, although several theories have been postulated, such as direct trauma to the globe, shearing forces resulting from extreme rotation of the globe, a sudden massive increase in intraocular pressure resulting in rupture of the lamina cribrosa and expulsion of the globe, sudden forward displacement of the globe and focal or diffuse vasospasm in the optic nerve (Sanborn et al. 1984; Vries-Knoppert 1989). Another of the mechanisms described accuses concussion waves arising from facial injury, which are conducted through surrounding bones and tissues into the orbit (Temel & Sener 1988). However, despite the various mechanisms that have been postulated, the pathophysiological rationale for the occurrence of an ONA in a minor head injury without direct trauma to the globe is still unclear. Chaudhry et al. (2006) proposed a wedge effect as a possible cause in children who sustained ONA from door-handle trauma. In all their patients, pointed door handles had entered the orbital compartment medial to the globe, pushing the globe against the lateral orbital wall and towards the anterior.
Only a few case reports have focused on late changes associated with ONA (Stanton-Cook 1953; Roberts et al. 1992). The purpose of this report is to describe the longterm changes in children with ONA caused by traumatic injury. In particular, the remarkable differences in courses and clinical outcomes may elucidate the spectrum of morphological change and functional loss associated with ONA.
Materials and Methods
A retrospective chart review of our institutional diagnostic database was performed to identify all children with a history of ONA seen between 1993 and 2007. The clinical charts of these patients were reviewed in detail regarding the circumstances leading to the traumatic event. Patient demographics including age, gender and mechanism of injury were analysed. Clinical characteristics obtained from medical records included visual acuity (VA) at diagnosis and at outcome, presence of any relative afferent pupillary defect, use of any diagnostic tools such as fundus photography or computed tomography (CT), treatment, secondary morphological changes and length of follow-up.
Case Reports
Case 1
A 14-month-old girl was admitted to our emergency unit 1 hour after she had fallen down a staircase for a distance of about 2 m. Clinical examination revealed a bruise over the left zygomatic bone. The only neurological deficit was a left absolute afferent pupillary defect in an otherwise healthy child. Examination of the right eye showed a normal anterior segment and fundus. Function in the left eye was reduced to no light perception. No anterior pathology was found, but funduscopy revealed a 360-degree ONA including mild intravitreal haemorrhage, peripapillary haemorrhages and surrounding retinal oedema.
Computed tomography was consistent with, but not specific for, ONA. One week later, funduscopy revealed almost resorbed vitreous haemorrhage, progressive retinal oedema with venous tortuosity, as well as sub- and intraretinal bleedings. Three weeks later, a pale swollen retina without any retinal vasculature was seen (Fig. 1). Five months later, fibrovascular tissue obscured the ONH and extended into the vitreous. During routine follow-up 3 years after the injury, fundus examination revealed a complete retinal detachment. No remarkable morphological differences were detected during the rest of the 7-year follow-up.
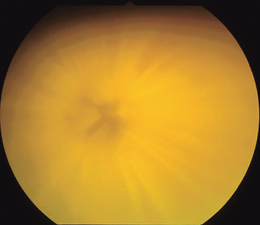
Optic nerve avulsion in patient 1. Ophthalmoscopy shows significant swelling of the retina without any visible retinal vasculature 4 weeks after trauma.
Case 2
A 6-year-old girl suffered a bicycle accident in which she hit the handle-bar. On initial presentation 3 hours after the accident, VA was light perception in the right eye and 20/20 in the left eye. External examination of the right eye revealed mild periorbital oedema, ecchymosis and a superficial skin laceration in the region of the nasal upper lid. Slit-lamp biomicroscopy showed a microhyphaema in the anterior chamber. The cornea and lens were intact and clear. There was an anisocoria caused by the right-sided traumatic mydriasis. A right relative afferent pupillary defect was also present. Funduscopy showed partial ONA with retrodisplacement of the temporal part of the optic disc. Further findings were vitreous haemorrhage that was most prominent inferiorly, peripapillary haemorrhages and surrounding retinal oedema (Fig. 2A).
Partial optic nerve avulsion (ONA) in patient 2. (A) The patient presented with temporal ONA, vitreous haemorrhage that was most prominent inferiorly, peripapillary haemorrhage and surrounding retinal oedema. (B) Complete resorption of haemorrhage and the beginning of fibroglial proliferation is demonstrated 2 months after injury. (C) This led to extended fibroglial scarring from the posterior scleral outlet 4 years after trauma. (D) The enormous epiretinal membrane is finally released spontaneously into the vitreous 11 years after optic nerve injury.
Computed tomography suggested partial ONA by demonstrating a discontinuity at the junction of the nerve and the globe and revealed non-dislocated fractures of the orbit floor and the medial wall of the orbit.
The patient was initially treated with 1 mg/kg bodyweight oral methylprednisolone daily for 5 days. On the third day after treatment, her VA increased to finger counting at 20 cm. Two months after injury, vision was 10/100 with no further recovery. The anisocoria disappeared, but the relative afferent pupillary defect was still present. Fundus examination showed an almost completely resorbed intraocular haemorrhage but new fibroglial scarring (Fig. 2B). Visual acuity 4 years later was preserved regardless of extended fibroglial scarring from the posterior scleral outlet (Fig. 2C). The opaque epiretinal membrane (ERM) grew further in dimension over time. At the patient’s last visit after 11 years of follow-up, the extremely large ERM was finally spontaneously released into the vitreous (Fig. 2D).
Case 3
A previously healthy, 5-year-old boy fell down a burrow, hitting a brick. The patient had concussion of the brain and no light perception in his left eye. The left pupil was unresponsive to light. Examination of the right eye showed a normal anterior and posterior segment. The left eye showed a small nasal subconjunctival haemorrhage and mild chemosis. The anterior chamber contained 2 + cells and flare. Funduscopic view was hazy in the presence of concurrent vitreous haemorrhage that was most prominent inferiorly. The ONH was obscured by the overlying vitreous haemorrhage, but a peripapillary subretinal haemorrhage and a pale, swollen retina were visible (Fig. 3A).
Optic nerve avulsion in patient 3. (A) The optic nerve head is obscured by the overlying haemorrhage, accompanied by peripapillary subretinal haemorrhage and a pale, swollen retina. (B) After 15 years, only some fibroglial scarring and mild retinal pigment epithelium hyperplasia remained, presenting an appearance reminiscent of a morning glory disc. In addition, mild venous tortuosity is present.
Computed tomography suggested ONA by demonstrating a discontinuity at the junction of the nerve and the globe. Although the haemorrhage resorbed, VA remained at no light perception. Follow-up examinations did not show substantial changes. The last examination 15 years later revealed only a little fibroglial scarring and some retinal pigment epithelium (RPE) hyperplasia. The ONH resembled a morning glory disc (Fig. 3B).
Discussion
In the three cases of ONA presented here, longterm follow-up revealed remarkable morphological differences. The diagnosis of ONA was easily established in the first two cases by fundus examination, which showed a pit of different dimensions in each case, rather than a normal ONH. In patient 3, an ONA diagnosis was initially suspected as a result of the complete visual loss, unresponsive pupil and the presence of a significant vitreous haemorrhage. Diagnosis was later supported by CT.
In patient 1, a pale and swollen retina without any visible retinal vasculature appeared early in the course of observation. The absence of retinal perfusion is quite common (Sanborn et al. 1984; Buchwald et al. 2003), although other authors have reported intact perfusion (Parks et al. 1971; Fard et al. 1997). Pulling forces seem to be better tolerated by vessels than by nerve fibres. Patient 1 later suffered a complete retinal detachment as a result of a tractive fibroglial scar. More common but still rare a limited tractive retinal detachment occurs in the parapapillary zone (Hillman et al. 1975; Sanborn et al. 1984).
Patient 2, who had a partial ONA, developed fibroglial scarring from the posterior scleral outlet within only 2 months of the trauma. The fibroglial membrane grew enormously during the following years. Fibroglial proliferation is a common finding in patients with ONA (Stanton-Cook 1953; Hillman et al. 1975; Simsek et al. 2006). However, the dimensions of the opaque secondary ERM seen in patient 2 are unique. Such membranes are composed of multiple cell types and collagen (Benhamou et al. 2002). In most cases, ERMs originate from retinal glial cells and RPE cells. Cells can proliferate through lesions of the internal limiting membrane or even migrate through intact retina (Trese et al. 1983). The ERM in patient 2 avulsed spontaneously into the vitreous after almost 11 years, indicating at least a partial separation of the posterior vitreous. This spontaneous release has rarely been seen in idiopathic and secondary membranes (Allen & Gass 1976; Greven et al. 1988).
Patient 3 developed only a few subsequent changes to the intraocular architecture, with minor fibroglial scarring and mild RPE hyperplasia observed during the 15-year follow-up period.
The longterm follow-up of our patients (7–15 years) is extraordinary compared with the considerably shorter follow-up periods of other studies. To our knowledge, only two reports of patients with ONA with comparable lengths of follow-up have described secondary changes to the intraocular architecture (Stanton-Cook 1953; Roberts et al. 1992).
The presenting VA of both patients with complete ONA (patients 1 and 3) was no light perception. Visual acuity did not recover over time. In patient 2, who had partial ONA, VA improved from light perception immediately after trauma to 10/100 early in the course of follow-up and remained constant despite the presence of an extensive ERM. In the absence of additional vision-impairing factors, such as vitreous haemorrhage or retinal damage, the individual’s final visual outcome seems to depend on his or her VA immediately after the injury (Foster et al. 1997). Early recovery of VA might be permanent, as observed in patient 2, whose follow-up has extended to 11 years. However, no late recovery of VA seems to occur.
In conclusion, the presented cases illustrate remarkable diversity in morphological longterm changes associated with ONA. However, late-stage morphology had no impact on visual outcome in our cases.




