ULTRASONOGRAPHIC IDENTIFICATION OF VASCULAR INVASION BY ADRENAL TUMORS IN DOGS
Abstract
Adrenalectomy is the treatment of choice for adrenal tumors that are producing adverse clinical signs. Surgical planning prior to adrenalectomy is aided by identifying tumors with invasion into adjacent vessels or the presence of a tumor thrombus extending into the caudal vena cava. In this paper, we evaluated the sensitivity and specificity of ultrasound in determining if vascular invasion or tumor thrombus is present. Thirty-four dogs with 36 adrenal tumors were reviewed retrospectively. Overall, 36% of tumors had vascular invasion. Abdominal ultrasound was 100% sensitive and 96% specific in identifying the presence of a tumor thrombus in the caudal vena cava. The sensitivity and specificity was 76% and 96%, respectively, when all forms of vascular invasion were evaluated and included patients with vascular wall invasion without concurrent thrombus. Abdominal ultrasound is a good screening tool for identifying vascular invasion or tumor thrombus associated with adrenal tumors in dogs.
Introduction
drenocortical tumors are relatively common in dogs and account for 10–20% of naturally occurring hyperadrenocorticism.1 These tumors secrete cortisol independent of pituitary control and, rarely, may secrete excessive amounts of aldosterone or sex steroid hormones.1-5 Pheochromocytomas arise from chromaffin cells of the adrenal medulla and secrete excessive amounts of catecholamines.6 Clinical signs and complications associated with adrenal tumors arise from the excessive elevation of steroid hormones and catecholamines or the presence of a space occupying mass.1, 6-12
Treatment of hyperadrenocorticism is aimed at controlling the excessive production of steroid hormones and adrenocortical tumors are typically resistant to medical management.13 Pheochromocytomas are frequently an incidental finding and can produce vague or nonspecific clinical signs. However, severe and life-threatening clinical signs have been reported. 6, 9-11 Adrenalectomy is the treatment of choice for functional adrenal tumors or tumors causing adverse clinical signs. Criteria influencing surgical candidates include age, concurrent disease, the size and invasiveness of the tumor, the presence of vascular invasion, the presence of metastatic disease, and anesthetic risk to the patient.6, 14 Accurate staging relies on identification of invasion into the surrounding vasculature. Regional vascular invasion may be as high as 82% for pheochromocytomas15 and ranges from 11% to 41% for adrenocortical tumors.8, 16-19 In two studies, the presence of a tumor thrombus did not affect outcome.7, 19 In one of these, with 40 dogs, there was no significant difference in perioperative complications or postoperative deaths between dogs with or without a caval thrombus. However, two of four dogs with intraabdominal metastasis had a tumor thrombus and two of five dogs with tumor thrombi had recurrence of their clinical signs. In a more recent study of 52 dogs, the presence of a tumor thrombus was associated with shorter survival.16 Also, tumor thrombosis was more likely with tumors greater than 5 cm in size. Additionally, dogs with vascular invasion necessitating nephrectomy had shorter survival times or increased perioperative mortality.7, 16 Finally, in 50 other dogs with pheochromocytoma, the presence of an intravascular tumor thrombus was associated with an increase in hepatic, regional lymph node, and distant metastasis.11
Ultrasound is used often to assess for vascular invasion of an adrenal tumor. In two studies of pheochromocytoma, ultrasound allowed for identification of four of 20 (20%), and four of seven (57%) adrenal tumors with invasion into the caudal vena cava but the accuracy of vascular invasion was not reported.9, 11 More recently, ultrasound was 80% sensitive and 90% specific for vena cava invasion.19 Our purpose was to evaluate the accuracy of ultrasound in detecting vascular invasion or tumor thrombi associated with adrenal tumors and confirm the ultrasonographic diagnosis with surgery, necropsy, and histopathologic findings.
Materials and Methods
Medical records from 1990 to 2002 were reviewed for dogs with a diagnosis of an adrenal mass. Selection criteria included an ultrasonographic exam of an adrenal mass, histologic confirmation of adrenal neoplasia obtained by surgical biopsy, necropsy, or both, and histologic or surgical confirmation of the presence or absence of vascular invasion or tumor thrombus. Thirty-four dogs with 36 adrenal tumors satisfied the selection criteria. All masses were confirmed histologically to be an adrenocortcical adenoma, adrenocortical carcinoma, or pheochromocytoma of the adrenal medulla and all masses were greater than 1.0 cm in size. Vascular invasion was defined as tumor thrombi extending into the lumen of a blood vessel or invasion of tumor cells into the tunica intima, media, or adventitia of the vein without formation of a thrombus. All original ultrasound images and reports were reviewed by a board-certified radiologist and the author (R.S.) and evaluated for the presence or absence of tumor invasion into the surrounding vasculature. Medical records, surgical and necropsy reports, and histopathologic reports were reviewed. Pearson's Chi-squared cross-tab analysis was used to evaluate the relationship between ultrasound and vascular invasion. Factors evaluated included the histologic diagnosis of tumor, the side of the tumor (right or left sided), evidence of vascular invasion on ultrasonographic exam, the vessel affected if reported, type of vascular invasion present (invasion into the adjacent vessel wall only or the presence of a tumor thrombus in the caudal vena cava), the accuracy of ultrasound to identify vascular invasion, and the correlation between a specific tumor type and the presence of vascular invasion. Statistical significance was determined to be present with a P-value < 0.05.
Results
Thirty-six adrenal tumors were evaluated for this study. Ultrasonographic descriptions of the masses ranged from well-circumscribed, homogenous, and isoechoic compared to the kidney cortex, to complex with heterogenous echogenicity, irregular, and poorly circumscribed. Eight tumors were right sided, 24 were left sided, and two dogs had bilateral tumors. Twenty-two tumors were adrenocortical with 13 adenomas and nine carcinomas. Fourteen were pheochromocytomas. Thickness measurements were available for 21 of 23 malignant tumors and 16 were greater than 2 cm.
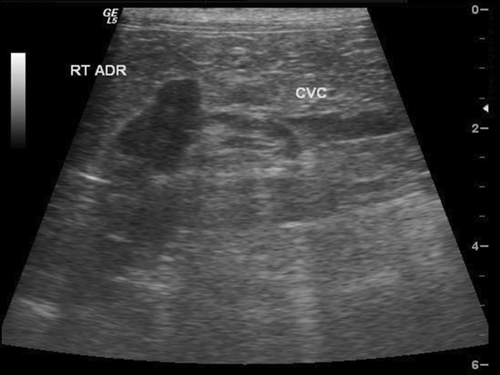
Twenty-two of the 36 tumors (61%) did not have surgical or histopathologic evidence of vascular invasion and were characterized correctly by ultrasonography (Fig. 1). Of these 22, 12 were adrenocortical adenomas, five were carcinomas, and five were pheochromocytomas.
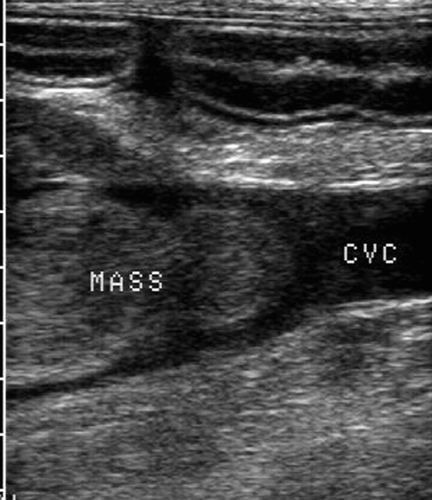
Nine of the 36 adrenal tumors were correctly identified by ultrasonography as having vascular invasion with a tumor thrombus that was confirmed by histology or surgery or both. In all nine of these, the thrombus was present in the caudal vena cava (Fig. 2). Tumor thrombi were characterized sonographically as a well-circumscribed mass with increased intravascular or intraluminal echogenicity. Histopathologically, tumor thrombi were described as an extension of neoplastic cells into the blood vessel lumen. Of the nine tumors with vena caval invasion, seven were pheochromocytomas and two were adenocarcinomas. Pheochromocytomas were statistically more likely to form a tumor thrombus than other adrenal tumor types (P < 0.003).
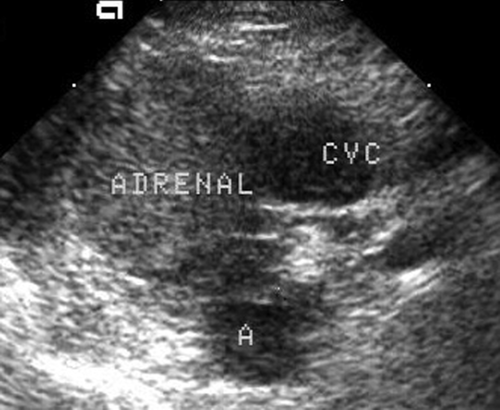
In four dogs, ultrasound failed to identify surgically or histopathologically confirmed vascular invasion when this occurred without development of a caudal vena cava thrombus (Fig. 3). In two of these, the caudal vena cava was reported to have no thrombus but the adrenal masses were immediately adjacent to the vena cava and in one patient, the vessel narrowed as it coursed around the tumor. Two of the tumors were carcinomas, one was a pheochromocytoma, and one was an adenoma. The two carcinomas and pheochromocytoma had histopathologic invasion into the caudal vena cava without the formation of an identifiable thrombus and the adenoma had vascular invasion into the phrenicoabdominal vein only. In one dog, a false-positive diagnosis occurred when a caudal vena cava thrombus was suspected on an initial ultrasonographic evaluation but was not identified upon a subsequent examination and surgery performed within 24 hours.
Overall, thirteen of 36 tumors (36%) had gross or histopathologic evidence of vascular invasion. Ultrasound correctly identified 86% of vascular invasion. Ultrasonography was 100% sensitive and 96% specific in identifying tumors with a thrombus extending into the lumen of the caudal vena cava. Ultrasonography was 76% sensitive and 96% specific when all forms of vascular invasion were included in the evaluation and included tumors with invasion into the wall of adjacent vessels without a concurrent intraluminal thrombus. There was a significant association (P < 0.001) between ultrasound detection of vascular invasion and surgical and/or histopathologic findings. Also, malignant adrenal tumors (pheochromocytomas, followed by adenocarcinomas) were statistically more likely to have vascular invasion than benign adenomas (P < 0.025). No other factors were found to influence the relationship between ultrasound, clinical factors, and vascular invasion.
Discussion
The incidence of a tumor thrombus or vascular invasion associated with adrenal tumors has been reported to be 11–82% in dogs undergoing surgical resection.7, 8, 11, 15-19 The incidence of vascular invasion and tumor thrombi for pheochromocytomas ranges from 12% to 82%.7, 9, 11, 12, 15, 17, 19, 20 In this study, pheochromocytomas were more likely to invade adjacent vessels and 57% of the pheochromocytomas had vascular invasion. In humans, vena cava thrombi associated with adrenal tumors often develop by intraluminal extension from the adrenal or renal vein and less commonly by direct invasion.21 In 40 dogs with surgical treatment of an adrenal tumor, most dogs with vena cava thrombi had extension of the thrombus from the phrenicoabdominal vein overlying the adrenal gland supporting the theory reported in humans.19 In 17 other adrenal masses, vascular invasion occurred from intraluminal extension by way of the phrenicoabdominal vein. 22 In our study, there were not adequate histopathologic data on most of the smaller adjacent vessels to support the theory of extension of tumor through the phrenicoabdominal vein.
In people, computed tomography (CT) and magnetic resonance (MR) imaging remain the primary mode of adrenal imaging and are useful for staging due to better characterization of tumors, identification of local invasion into adjacent organs, and identification of vascular invasion or tumor thrombi.23, 24 Using CT or MR imaging, adrenal tumors can often be characterized as benign or malignant using size, homogeneity of the tumor, contrast enhanced studies with relative washout on CT, and T2-weighted signal intensity and heterogeneity on MR imaging.23-25 In 15 dogs with 17 adrenal masses, CT was 92% sensitive and 100% specific for identifying vascular invasion.22 As in our study, a false negative was found in one dog with invasion limited to the phrenicoabdominal vein.
In a human study, ultrasonography and CT correlated closely in identifying adrenal lesions with ultrasound being 96% sensitive and 92% specific in correctly detecting adrenal masses and was accurate at identifying lesions less than 2 cm in diameter.26 In dogs, adrenal gland size has been correlated with malignancy and tumors with a maximum thickness greater than 2 cm were more likely to be malignant.27 In our population, 76% of malignant tumors had thickness measurements greater than 2 cm. Our study also had a higher distribution of adrenocortical adenomas than adenocarcinomas compared to previous studies that reported more carcinomas.7, 8, 18 The inclusion criteria, which required that dogs have an ultrasound description of an adrenal mass with surgical or histopathologic confirmation of an adrenal tumor, may have led to more benign tumors in our population. Not all dogs in this study had symptoms related to their adrenal tumor or had surgery specifically for an adrenal tumor. Also, histopathologic differentiation of adrenocortical adenomas from adenocarcinomas is challenging. Criteria for differentiating include size, vascular or capsular invasion, local extension, necrosis, or cystic degeneration.1
We found ultrasound 100% sensitive and 96% specific in detecting vascular invasion when a tumor thrombus was present in the caudal vena cava. However, identifying subtle invasion into vessel walls or into smaller adjacent vessels such as the phrenicoabdominal vein or renal vein remains challenging. Tumors abutting adjacent vessels, surrounding the vessel, or narrowing the vessel as it courses by should raise suspicion for vascular invasion. Advances in image quality and resolution may improve the ability to detect more subtle invasion and future prospective studies with attention to these details will be helpful in assessing the ability of ultrasound to identify all forms of vascular invasion.
In conclusion, we found that abdominal ultrasonography was useful in determining the presence of a vascular thrombus in dogs with adrenal tumors. Although CT or MR imaging may ultimately be used for surgical planning or to identify subtle invasion, ultrasound is a very useful screening tool for dogs with adrenal tumors, characterizing 86% of the tumors correctly.