Influence of severity of illnesses on risk of death in intensive care unit patients with severity of pressure injuries as mediating variable
Abstract
This study was to verify whether the severity of pressure injuries (PIs) in intensive care unit (ICU) patients plays a mediating role in the relationship between severity of their illnesses and risk of death. I examined adult patients admitted to the ICUs between 1 January 2014 and 31 August 2021. The average follow-up period was 11.34 months. A total of 390 ICU patients suffered from PIs. The influences of the APACHE II score of the ICU patients on the mediating variable ‘unstageable & DTPIs vs. Stage 1&2 PIs’ and on risk of death were significant. After controlling the influence of APACHE II score on risk of death, the influences of mediating variables ‘Stage 3&4 PIs vs. Stage 1&2 PIs’ and ‘unstageable & DTPIs vs. Stage 1&2 PIs’ on risk of death were also significant. The regression coefficient of APACHE II score of the ICU patients declined after the severity of PIs was included. The Sobel test on the indirect effects also reached the level of significance. The severity of illnesses is a factor that is beyond my control, severe PIs should still be prevented to lower the risk of death.
1 INTRODUCTION
The intensive care unit (ICU) is a unique department that cares for critically ill patients. Its medical care objective is to save lives and restore patient health; however, due to the severity of their illnesses, approximately 20%–50% of patients die in ICUs.1-3 Faced with a high mortality rate and rapid changes in the conditions of ICU patients as well as the complexity and variability of treatment, medical personnel often focus on treating patients and dealing with symptoms whereby physical care, unfortunately, tends to be overlooked.4 The incidence rate of pressure injuries (PIs) is a crucial indicator for monitoring nursing quality.5 Means of controlling the mortality rate of ICU patients while providing them with quality nursing have always been the goal for which medical personnel aim.
PIs are the most common problem encountered by patients requiring acute or long-term hospitalization. Caused by tissue hypoxia and ischemia due to compression, PIs can eventually lead to ulcers or necrosis if adequate treatment is not given. In the United States, over 2.5 million patients suffer from PIs every year resulting in an estimated USD 9–11 billion in expenses.6 Most critically ill patients in the ICU are bedridden and unable to move freely. In addition to this, multiple factors including the high severity of their illnesses, unstable haemodynamics, the use of vasoconstrictors or sedatives and malnutrition all contribute to limited mobility and a reduction in the ability to change positions on their own, thereby extending the time that tissues are subjected to continued pressure. Consequently, ICU patients are at increased risk of developing PIs.7 The incidence rate of PIs in ICU patients ranges from 6.9% to 14.3%,8-10 which is 10 times higher than that in patients in general wards.11
A number of severity scoring systems exist for illnesses in ICUs. At present, most hospitals employ the Acute Physiology and Chronic Health Evaluation (APACHE) scoring system to assess the mortality rate of critically ill patients. The APACHE II scoring system was developed more than 20 years ago and remains the most versatile and widely accepted scoring system among hospitals. It is employed to assess the severity of diseases in ICU patients and their prognosis.12, 13
For ICU patients, PIs are a complex problem with multiple factors that are often overlooked by medical personnel.14 The more damaged an ICU patient's skin becomes due to PIs, the more easily it is for bacteria to invade the soft tissue layer, causing redness, swelling, warmth and pain, with cellulitis being one of the possible complications.15 If a PI is deep and near a bony prominence, bacteria could also invade the bone, causing severe infections such as septic arthritis or osteomyelitis that could even develop into systemic sepsis, which can lead to death.16 Thus, the severity of PIs in ICU patients is likely associated with their risk of death.
Despite the numerous studies that have been conducted on PIs in ICU patients, they have been limited to assessing the risk factors of PIs and the knowledge of medical personnel.17-19 Moreover, any mentions connecting PI occurrence and the severity of illnesses in the ICU patients were only acknowledgements.20 Because analyses on PI severity are extremely rare, I aimed to determine whether the severity of PIs in ICU patients plays a mediating role in the relationship between severity of illnesses and risk of death. Figure 1 displays the research framework.
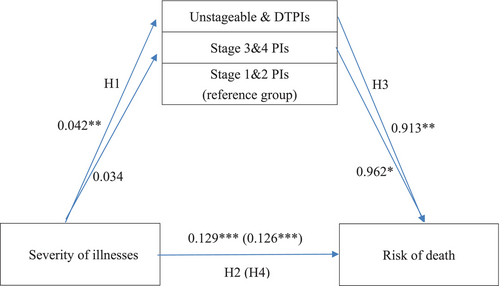
H1.The severity of illnesses in ICU patients exerts a significant influence on the stage of their PIs.
H2.The severity of illnesses in ICU patients exerts a significant influence on their risk of death.
H3.The stage of PIs in ICU patients exerts a significant influence on their risk of death.
H4.The stage of PIs in ICU patients mediates the relationship between illness severity and risk of death.
2 MATERIALS AND METHODS
2.1 Design and participants
I collected cases involving adult patients admitted to the ICUs of a teaching hospital in northern Taiwan. This retrospective cohort study compiled a list of patients who had suffered from PIs in the ICUs using the hospital's adverse event reporting system (AERS) and data regarding the location, time of occurrence and severity of their PIs. This was coordinated with an electronic medical record review to obtain the basic attributes, disease diagnoses and examination results of the patients.
I examined adult patients over the age of 20 who had been admitted to the ICUs between 1 January 2014 and 31 August 2021, had suffered from PIs during their hospital stay and had been confirmed as having PIs in the hospital's AERS. Patients who had suffered from PIs before the study period were excluded. A total of 390 cases were examined.
2.2 Sample size
Binary logistic regression analysis was conducted using G-power to derive the required number of samples. For a type-I error of 5% and 90% power, I estimated that I needed at least 347 samples; thus, the 390 samples in this study were adequate.
2.3 Data collection
I collected data by reviewing the medical records of the patients and comparing them with records on the AERS. The data included the age and gender of the patients, albumin reports within 3 days of PI occurrence, haemoglobin reports on the day of PI occurrence, the use of a ventilator, comorbidities (hypertension, diabetes, kidney diseases and cancer), APACHE II score (the poorest score within 24 h of being admitted to the ICU), as well as the area, location and stage of the PIs. I then followed up on the survival conditions of the patients.
The APACHE score is currently the index most widely used in ICUs to represent the severity of illnesses. The APACHE II score is the sum of three score points: the acute physiology score points, age points and chronic health points. The acute physiology score points include 12 variables, including body temperature, heart rate, mean arterial pressure, respiratory rate, arterial PO2, blood pH, serum sodium, serum potassium, serum creatinine, haematocrit, white blood cell count and the Glasgow Coma Score. The age points are divided into five ranges: 75 years old and above, 65–74 years old, 55–64 years old, 45–54 years old and 44 years old and below. For the chronic health points, the following must be determined: whether the patient has cirrhosis, class IV heart failure (according to the functional classification of the New York Heart Association (NYHA)), severe COPD or pulmonary hypertension (> 40 mmHg), and whether the patient is using a ventilator, on regular dialysis or immunocompromised. The APACHE II score ranges from 0 to 71 points, with a higher score indicating greater illness severity. The APACHE II score is a good predictor for mortality; its area under the curve (AUC) value can reach 0.863.21 For every 5-point increase in the APACHE II score, the mortality rate increases significantly. For instance, the mortality rate of a patient with an APACHE II score between 30 and 34 is 73%; an increase in the APACHE II score to 35 or higher increases their mortality rate to 84%.21 Furthermore, Kruse et al. demonstrated that there were no significant differences between the APACHE II scores calculated by doctors and those calculated by nurses and that their judgements were consistent.22
The National Pressure Injury Advisory Panel (NPIAP) defines PIs as damage induced by prolonged external pressure to the skin and the soft tissue under the skin.23 Stage 1 PIs present intact reddened skin that does not blanch when pressed with a finger. Stage 2 PIs show a pink wound and blisters but no dead tissue or bruising. Stage 3 PIs refer to full-thickness skin damage that reveals subcutaneous fat but not any bone, tendons or muscles. Stage 4 PIs present full-thickness skin tissue damage that reveals bone, tendons or muscles. There may be dead tissue or scabs usually accompanied by undermining or tunnelling wounds. Unstageable PIs show full-thickness skin tissue damage. The base of the wound beds, however, is covered by dead tissue or eschar, thereby preventing the depth of the ulcer from being confirmed. Deep tissue pressure injuries (DTPIs) present deep tissue damage caused by pressure or shear force. Local intact skin is purple or maroon or presents blood-filled blisters. In this study, I divided the severity of PIs into three groups: Stages 1&2, Stages 3&4 and unstageable and DTPIs.
I compiled a list of adult ICU patients who suffered from PIs between 1 January 2014 and 31 August 2021. With the date of PI occurrence as the time point of the starting event and death as the endpoint/event, I followed up on all of the patients until 30 September 2021, to confirm whether an event had occurred. The results were then used to calculate the survival statistics of the patients. The average follow-up period of the patients was 11.34 months (SD = 17.63, range = 0.03–93.57).
2.4 Ethical considerations
This study was approved by the Taipei Medical University Joint Institutional Review Board (TMU-JIRB No. N202003064). I explained to the hospital My study objective and method of collection before collecting data regarding adult ICU patients who had been reported for PIs on the AERS and before reviewing the medical records of the patients to collect their basic attributes and examination results. In consideration of ethics and patient rights, the personal data and privacy of the patients remained confidential, and I ensured that their inclusion or exclusion in this study did not affect their treatment or care.
2.5 Data analysis
The data collected in this study were computer-coded and filed. Statistical analyses were performed using SPSS 25.0 for Windows. The descriptive statistics included quantity, mean, percentage and standard deviation. The inferential statistics were obtained using independent t-tests, analysis of variation (ANOVA) and chi-square tests. Finally, I examined the indirect influence of the severity of illnesses in ICU patients (independent variable) on the risk of death (dependent variable) via the severity of PIs (mediating variable). I adopted the mediation analysis process established by Baron and Kenny, which requires four conditions to be met: (1) the independent variable is significantly correlated with the mediating variable, (2) the independent variable is significantly correlated with the dependent variable, (3) the mediating variable is significantly correlated with the dependent variable and (4) the relationship between the independent variable and the dependent variable is weakened when the mediating variable is included in the regression model.24
As the severity of PIs was a categorical variable with three categories, I employed multinomial logistic regression to test the correlation between the independent variable and the mediating variable. The risk of death was a binary categorical variable; therefore, I adopted binary logistic regression to test the correlation between the independent variable and the dependent variable, between the mediating variable and the dependent variable and between the independent variable and the dependent variable when the mediating variable was included in the regression model. Furthermore, I added Sobel's test to determine whether the indirect effect of the mediating variable, that is, severity of PIs, was significant.25
3 RESULTS
3.1 Demographic characteristics and pressure injuries data
As shown in Table 1, based on the statistics of the collected cases, a total of 390 ICU patients suffered from PIs, over half of whom did not survive until the end of the study period (n = 267, 68.5%). The mean age of the patients was 69.11 years old (SD = 14.24). Most of the patients were male (n = 274, 70.3%). The mean haemoglobin level of the patients on the day of PI occurrence was 9.71 g/dL (SD = 2.02), and their mean albumin within 3 days of PI occurrence was 2.68 g/dL (SD = 0.61). The majority of the patients had used a ventilator (n = 300, 76.9%), and kidney diseases were the most common comorbidity (n = 203, 52.1%). Their mean APACHE II score was 24.19 (SD = 7.85), and the mean area of their PIs was 19.75 cm2 (SD = 49.39). Their PIs were most commonly found at the sacrum and the ischium (n = 142, 36.4%), and the second most common area was on the face (including the ears) (n = 128, 32.8%). Stage 3&4 PIs were the most common (n = 184, 47.2%), followed by Stage 1&2 PIs (n = 112, 28.7%).
| Item | n | % |
|---|---|---|
| Patients | 390 | |
| Survivors | 123 | 31.5 |
| Non-survivors | 267 | 68.5 |
| Gender | ||
| Male | 274 | 70.3 |
| Female | 116 | 29.7 |
| Using ventilator | 300 | 76.9 |
| Comorbidities | ||
| Hypertension | 170 | 43.6 |
| Diabetes | 184 | 47.2 |
| Kidney diseases | 203 | 52.1 |
| Cancer | 94 | 24.1 |
| Location of PIs | ||
| Upper limbs and torso | 39 | 10.0 |
| Lower limbs | 62 | 15.9 |
| Back (including scapula, occipital bone) | 19 | 4.9 |
| Face (including ears) | 128 | 32.8 |
| Sacrum and ischium | 142 | 36.4 |
| Severity of PIs | ||
| Stages 1&2 | 112 | 28.7 |
| Stages 3&4 | 184 | 47.2 |
| Unstageable and DTPIs | 94 | 24.1 |
| Item | Mean | SD |
|---|---|---|
| Age (years) | 69.11 | 14.24 |
| Haemoglobin (g/dL) | 9.71 | 2.02 |
| Albumin (g/dL) | 2.68 | 0.61 |
| APACHE II score | 24.19 | 7.85 |
| Area of PIs (cm2) | 19.75 | 49.39 |
- Abbreviations: DTPI, deep tissue pressure injury; PI, pressure injury; SD, standard deviation.
3.2 Mediating effect testing
As shown in Table 2, the influence of the independent variable ‘severity of illnesses’ on mediating variable ‘unstageable & DTPIs vs. Stage 1&2 PIs’ was significant (OR = 1.04, p = 0.007), thereby meeting the first condition for mediating effects. In contrast, the influence of ‘severity of illnesses’ on mediating variable ‘Stage 3&4 PIs vs. Stage 1&2 PIs’ was not significant (OR = 1.03, p = 0.129). The influence of the independent variable ‘severity of illnesses’ on the dependent variable ‘risk of death’ was significant (OR = 1.14, p < 0.001), thereby meeting the second condition for mediating effects. After controlling the influence of ‘severity of illnesses’ on ‘risk of death’, the influences of mediating variables ‘Stage 3&4 PIs vs. Stage 1&2 PIs’ (OR = 2.62, p = 0.042) and ‘unstageable & DTPIs vs. Stage 1&2 PIs’ (OR = 2.49, p = 0.004) on ‘risk of death’ were significant. Furthermore, the regression coefficient of the independent variable ‘severity of illnesses’ declined from 0.129 to 0.126, thereby meeting the fourth condition for mediating effects.
| Dependent variable/independent variable | B | SE | OR (95% CI) | p |
|---|---|---|---|---|
| Stages 3&4/severity of illnesses | 0.034 | 0.02 | 1.03 (0.99–1.08) | 0.129 |
| Unstageable and DTPIs/severity of illnesses | 0.042 | 0.02 | 1.04 (1.01–1.08) | 0.007 |
| Risk of death/severity of illnesses | 0.129 | 0.02 | 1.14 (1.10–1.18) | <0.001 |
| Risk of death/severity of illnesses | 0.126 | 0.02 | 1.13 (1.09–1.18) | <0.001 |
| Risk of death/severity of PIs (ref: Stages 1&2) | ||||
| Stages 3&4 | 0.962 | 0.47 | 2.62 (1.04–6.62) | 0.042 |
| Unstageable and DTPIs | 0.913 | 0.32 | 2.49 (1.34–4.62) | 0.004 |
- Abbreviations: B, unstandardized coefficients; CI, confidence interval; DTPI, deep tissue pressure injury; OR, odds ratio; SE, standard error.
In summary, using Baron and Kenny's mediation analysis to examine the mediating effect of mediating variable ‘unstageable & DTPIs vs. Stage 1&2 PIs’ on the relationship between ‘severity of illnesses’ and ‘risk of death’ revealed that all four conditions were met, thereby indicating that ‘severity of PIs: unstageable & DTPIs vs. Stage 1&2 PIs’ is a mediating variable of the influence of ‘severity of illnesses’ on ‘risk of death’. I then employed the Sobel test to test the indirect effects, and the results also reached the level of significance (Z = 2.52, p = 0.012). I therefore confirmed that the hypothesis regarding the mediating effects of ‘severity of PIs: unstageable & DTPIs vs. Stage 1&2 PIs’ was supported. When Baron and Kenny's mediation analysis was used to examine the mediating effect of mediating variable ‘the severity of PIs: Stage 3&4 PIs vs. Stage 1&2 PIs’ on the relationship between ‘severity of illnesses’ and ‘risk of death’, not all four conditions were met. Moreover, the result of the Sobel test on the indirect effect was not significant (Z = 1.48, p = 0.139).
4 DISCUSSION
The results of this study indicated that ‘severity of PIs: unstageable & DTPIs vs. Stage 1&2 PIs’ in ICU patients was a mediating variable of the influence of ‘severity of illnesses’ on ‘risk of death’. This means that ICU patients with more severe illnesses are more likely to suffer from unstageable and DTPIs compared to Stage 1&2 PIs, which further increases their risk of death.
Studies on the severity of illnesses and PIs have merely discussed whether patients with severe illnesses suffered from PIs. For instance, Cox examined 347 patients in internal medicine and surgical ICUs and discovered a significant difference (t = −5.58, p < 0.01) between the APACHE II scores of patients who suffered from PIs (mean = 21.89, SD = 6.71) and those of patients who did not suffer from PIs (mean = 14.63, SD = 2.65).26 In a retrospective cohort study conducted by Gulin et al.27 21 out of 142 ICU patients (14.7%) suffered from PIs. After including age, the Braden scale risk score, the APACHE II score, length of stay in ICU and cause of ICU admission into the logistic regression analysis, they found that the APACHE II score was significantly correlated with the occurrence of PIs (OR = 1.05, p = 0.008). In a study involving 286 ICU patients, Theaker et al. recorded data for PI-related risk factors once every 8 h28; 77 of the patients suffered from PIs. They included Norepinephrine, APACHE II score 13, faecal incontinence, anaemia and length of stay 3 days in their logistic regression, which revealed a significant correlation between APACHE II score 13 and the occurrence of PIs (OR = 3.4, p = 0.004). This study is the first to examine the correlation between the severity of illnesses and the severity of PIs in ICU patients. The results revealed that ICU patients with more severe illnesses are more likely to suffer from unstageable and DTPIs compared to Stage 1&2 PIs. Note that this finding will require further support and verification from more research.
The APACH II score enhances the ability to predict the death of ICU patients in a hospital. It can quantify the severity of illnesses to predict mortality rates and aid clinical doctors in directing treatment and allocating medical resources. A number of studies have demonstrated that the APACHE II score can be used independently to predict the mortality rate of ICU patients.29, 30 For instance, Naved et al. obtained a mean APACHE II score of 20.84 from patients on their second day in the ICU and divided the APACHE II scores into five levels: 3–10, 11–20, 21–30, 31–40 and >40.31 They found that only three of the 30 patients (10%) with an APACHE II score of 3–10 died, whereas 33 of the 39 patients (84.6%) with an APACHE II score of 31–40 died, thereby highlighting that the mortality rate increases with higher APACHE II scores. The results of my study also indicate that ICU patients with more severe illnesses are at a greater risk of death. A statistical method has even been developed to estimate the mortality rate of ICU patients based on the APACHE II score.
Despite some studies indicating that PIs do not have a direct impact on the mortality rate of ICU patients, those studies did report that PI occurrence can indirectly increase the mortality rate of ICU patients.32, 33 However, other studies have advocated that PI occurrence is directly associated with increased rates of patient mortality. In a two-year prospective cohort study, Manzano et al. examined surgical ICU patients who had been on a ventilator for over 24 h.34 Among 563 patients, the mortality rate of the 110 patients who suffered from PIs was 48.7%. After applying the Cox model with time-dependent covariates, PI occurrence was confirmed as a crucial independent predictor of mortality rate (HR = 1.28, p = 0.047). In a retrospective cohort study, Ahtiala et al. examined 6089 ICU patients and found a PI incidence rate of 6.9% (423 patients).8 Their logistic regression analysis also demonstrated that PIs are an independent predictor of mortality rate. In my study, I further discovered that patients with Stage 3&4 PIs or unstageable and DTPIs were at greater risk of death than those with Stage 1&2 PIs. It is extremely likely that once PIs develop, the deteriorating natural defence mechanisms induced by severe illnesses in ICU patients not only lead to pain and discomfort but also delayed healing, which lengthens hospital stay, increases the chance of infection or bacteremia and even increases mortality rate.8, 35
This study demonstrated that ‘severity of PIs: unstageable & DTPIs vs. Stage 1&2 PIs’ of ICU patients played a mediating role in the relationship between severity of illnesses and risk of death. This means that ICU patients with severe illnesses and unstageable and DTPIs were at a greater risk of death than patients with Stage 1&2 PIs. The diseases of ICU patients are characterized by high complexity, and the main focus of medical personnel is on treating patient emergencies; as a consequence, the integrity of the skin of patients can be overlooked.36 Some researchers believe that even if medical personnel carefully evaluate the clinical conditions and the PI risk factors of patients, PI occurrence is still unavoidable in some patients.37 Other researchers believe that most PIs can be avoided or be stopped from worsening in ideal hospital conditions; however, medical personnel are limited, overworked or have no time to perform preventive measures. Nonetheless, the means of preventing PIs from occurring or worsening should be an essential issue in critical care.38
This was a retrospective study; thus, other conditions besides PIs, such as medical history and potential diseases, could not be controlled. Furthermore, I did not adopt a control group design, which could render the evidence somewhat weaker. I therefore suggest that future studies employ clinical trials with a greater number of participants and stricter inclusion and exclusion criteria. In addition, a control group and random designation should be included. Therefore, the results would present a higher level of evidence and more strongly demonstrate that the severity of PIs is indeed a mediating variable of the relationship between the severity of illnesses and risk of death in ICU patients.
5 CONCLUSION
The study found that ICU patients with more severe illnesses are at greater risk of death. Furthermore, unstageable and DTPIs and Stage 3&4 PIs increase the risk of death more than Stage 1&2 PIs do. This means that if ICU patients with severe illnesses have unstageable and DTPIs, their risk of death is greater than that of patients with Stage 1&2 PIs. Thus, the severity of PIs plays a mediating role in the relationship between the severity of illnesses and risk of death of ICU patients. Healthcare institutions should implement aggressive strategies to prevent PI deterioration. The discovery of a PI in an ICU patient should trigger the provision of good care, especially during the initial period of the PI, to prevent it from worsening, thereby reducing the patient's risk of death.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data analyzed during the current study are available from the corresponding author upon reasonable request.




