RETRACTED: Effect of humanised care on the surgical site wound infection after caesarean: A meta-analysis
Abstract
Herein, a meta-analysis was conducted to systematically evaluate the effect of humanised care on maternal postoperative wound infections in patients who underwent caesarean section. A computerised search of Embase, Cochrane Library, PubMed, Web of Science, China National Knowledge Infrastructure, Chinese Biomedical Literature Database and Wanfang database was performed, supplemented by a manual search from database inception to September 2023, to collate randomised controlled trials (RCTs) regarding the application of humanised care during the perioperative period of caesarean section. Two researchers screened and selected studies identified according to inclusion and exclusion criteria, and the included literature was evaluated for quality, extracted information and required data. Data analysis was performed using RevMan 5.4 software. Twenty RCTs comprising 2408 patients were included. The results revealed the humanised care group had a lower incidence of postoperative wound infections (0.83% vs. 4.32%, odds ratio [OR]: 0.26, 95% confidence interval [CI]: 0.15–0.46, p < 0.00001) and fewer postoperative complications than the conventional care group (4.32% vs. 16.35%, OR: 0.23, 95% CI: 0.16–0.31, p < 0.00001), with lower anxiety scores (standardised mean difference [SMD]: −3.15, 95% CI: −3.90 to −2.40, p < 0.00001) and depression scores (SMD: −3.68, 95% CI: −4.49 to −2.88, p < 0.00001). The application of humanised care during the perioperative period of caesarean section can prevent postoperative wound infection, reduce postoperative complications and help alleviate maternal anxiety and depression, which is worthy of clinical promotion and application.
1 INTRODUCTION
Caesarean section is a foetal delivery method in which the fetus is delivered via an abdominal incision and labour is not terminated vaginally. Caesarean section ensures a smooth delivery and reduces labour pains, but disadvantages such as incision infection and postoperative pain need to be considered, along with substantially delayed incision healing in the absence of proper care.1, 2 Postoperative wound infections not only lead to physical discomfort and delayed recovery, but also induce anxiety, depression and other negative emotions.3, 4 Various factors can lead to poor incision healing after caesarean section, including postpartum hormonal changes, the shock of surgery and the arrival of a newborn baby, which places mothers under heavy psychological pressure and hinders appropriate rest; these factors are well-recognised to increase the risk of incision infection.5 Wound infection has been linked to poor prognosis and increased costs of treatment, as well as infectious diseases and even life-threatening organ failure in severe cases.6 Caesarean section is a traumatic approach for foetal delivery, and the effective implementation of clinical care plays an pivotal role in the postoperative recovery of the mother.7 The incidence of complications after caesarean section was found to be considerably higher than that following natural delivery, and thus nursing care is more demanding.8, 9 Traditional routine care primarily involves the mechanical implementation of medical advice, often ignoring the psychological changes experienced by the mother, resulting in poor nursing results. Moreover, interventions to address maternal postpartum complications, mood disorders and other aspects have failed to achieve satisfactory results.10
Humanised care is a type of nursing care centred on the physical and mental health of the mother, a novel service concept that can be planned and targeted according to the physical and mental condition of the mother.11 Compared with traditional nursing, humanised nursing emphasises that nursing staff should maintain a good service attitude, consider the mother as the main focus, meet all reasonable needs of the mother as far as possible and pay attention to psychological care and gain the mother's trust, thereby providing quality nursing services.9, 12 During the process of obstetric care, the use of a humane care programme can strengthen the existing nursing effect, as well as the nursing staff's own awareness of nursing, comprehensively clarifying the importance of developing maternity-centred work.13 In recent years, numerous studies have compared the application of humanised care and conventional care in the perioperative period of caesarean section; however, data regarding wound infections remain insufficient and controversial. Therefore, in the current study, we performed a meta-analysis to comprehensively assess the effects of humanised care interventions on surgical site wound infections in patients who underwent caesarean section to provide a better selection of protocols.
2 MATERIALS AND METHODS
2.1 Literature search
We performed a computerised search of Embase, Cochrane Library, PubMed, Web of Science, China National Knowledge Infrastructure, Chinese Biomedical Literature Database and Wanfang databases from database inception to September 2023, to identify randomised controlled trials (RCTs) on the application of humanised care during the perioperative period of caesarean section. The search keywords were (humanised nursing OR humanised care) AND (caesarean section OR caesarean delivery). Additionally, cited references of the included literature were manually searched to identify any relevant studies that were not retrieved in the initial search.
2.2 Selection criteria
Inclusion criteria were as follows: (1) the study was an RCT; (2) the study population included full-term mothers who underwent caesarean section; (3) the interventions were humanised nursing intervention methods for the intervention group and conventional nursing intervention for the control group; and (4) the primary outcome indicators were the occurrence of wound infections and complications, while secondary outcome indicators included post-intervention maternal self-rating depression (SDS) and self-rating anxiety (SAS). Exclusion criteria were as follows: (1) studies for which the full text was unavailable or data access was incomplete; (2) reviews, lectures, case reports and conference papers; (3) duplicate publications; and (4) studies that did not describe the outcome indicators needed for this study.
2.3 Literature screening and data extraction
All studies were independently screened, and data were extracted by two researchers. All literature obtained from the preliminary search was imported into Endnote X9 software to identify and eliminate duplicates. The titles and abstracts were screened to eliminate studies that did not meet the inclusion criteria, and the final inclusion of the literature was determined by reading the full text and extracting relevant data and information. To ensure the completeness and accuracy of the data and information, two researchers were required to integrate and compare the results; in case of disagreement, consensus was reached by discussion with a third researcher. The extracted information and data mainly included (1) general information: authors' names and year of publication; (2) study characteristics: sample size, age, gestational week status and type of labour of the study participants; and (3) outcome indicators.
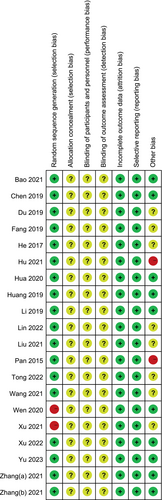
2.4 Literature quality assessment
The risk of bias in the included studies was evaluated using the quality evaluation criteria recommended by the Cochrane Handbook 5.1.0 for (1) random sequence generation, (2) allocation concealment, (3) blinding of subjects and researchers, (4) blinding of outcome assessors, (5) completeness of outcome data, (6) selective reporting of results and (7) other biases. Each entry was classified as high, unclear or low risk, according to the likelihood of the risk of bias. The results were cross-checked by two researchers after evaluating all the literature according to the evaluation table. In case of inconsistency, a third researcher adjudicated the results.
2.5 Statistical analysis
Data analysis was performed using the RevMan 5.4 software. Odds ratios (OR) were selected for count data and the standardised mean difference (SMD) was selected for continuous data. After combining the statistical effects, I2 and χ2 tests were used to detect heterogeneity between the studies; in the absence of significant heterogeneity (I2 < 50%, p > 0.1), a fixed-effects model was selected; otherwise, a random-effects model was selected. A 95% confidence interval (CI) was used for all findings and a difference of p < 0.05 was considered statistically significant. Sensitivity analyses were performed by sequentially removing each study and calculating the remaining data, which were considered robust and reliable if the data from the remaining literature did not significantly affect the combined results. To assess publication bias, included studies were subjected to funnel plot analyses.
3 RESULTS
3.1 Study selection
Based on the literature search strategy, a total of 705 articles were retrieved from seven databases; 369 duplicates were removed using Endnote software, as well as manually. Overall, 277 non-RCTs and articles inconsistent with the topic were excluded after reading the titles and abstracts. On reading the full text, 39 articles with missing data and lacking relevant endpoints were excluded; ultimately, 20 articles were included in the current meta-analysis.9, 10, 13-30 The literature screening process is shown in Figure 1.

3.2 Characteristics of included studies and quality assessment
The 20 included RCTs involved a total of 2408 patients, of which 1203 received humanised nursing interventions and 1205 received conventional nursing interventions. The included literature was all in Chinese, consistently reporting the incidence of incision infection and complications, and most reporting SAS and SDS scores. Table 1 presents the basic characteristics of the included articles. The risk of bias was assessed using RevMan 5.4 for the included literature and a literature quality evaluation map was plotted; two studies were assessed as high risk owing to the use of an incorrect randomisation method, two studies were assessed as high risk owing to large discrepancies in part of the data and most had unknown risk owing to the lack of data regarding allocation of concealment and blinding. Figure 2 presents the risk of bias.
| Author | Year | Number of patients | Age (years) | Gestational week | Maternal type (multipara/primipara) | Outcome indicators | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | |||
| Bao | 2021 | 65 | 65 | 27.79 ± 3.31 | 27.85 ± 3.25 | NR | NR | 26/39 | 27/38 | ①②③④ |
| Chen | 2019 | 40 | 40 | 37.8 | 37.06 | 39.1 | 39.6 | NR | NR | ①② |
| Du | 2019 | 20 | 20 | 29.42 ± 3.56 | 29.42 ± 3.56 | 39.65 ± 1.22 | 39.65 ± 1.22 | NR | NR | ①②④ |
| Fang | 2019 | 75 | 75 | 29.8 ± 0.9 | 29.9 ± 1.0 | 38.0 ± 0.6 | 38.1 ± 0.5 | 40/35 | 39/36 | ①②④ |
| He | 2017 | 45 | 45 | 26.1 ± 2.7 | 26.0 ± 2.5 | NR | NR | NR | NR | ①② |
| Hu | 2021 | 39 | 39 | 33.44 ± 2.56 | 32.54 ± 3.18 | NR | NR | NR | NR | ①②③④ |
| Hua | 2020 | 48 | 48 | 31.25 ± 2.36 | 31.12 ± 2.19 | 39.53 ± 1.12 | 39.42 ± 1.08 | NR | NR | ①② |
| Huang | 2019 | 60 | 60 | 25.1 ± 3.0 | 24.7 ± 3.9 | 38.6 ± 1.2 | 38.7 ± 1.3 | 0/60 | 0/60 | ①②③④ |
| Li | 2019 | 200 | 200 | 25.78 ± 2.41 | 25.76 ± 2.43 | NR | NR | NR | NR | ①②③④ |
| Lin | 2022 | 198 | 200 | 27.94 ± 2.85 | 27.63 ± 2.97 | 39.25 ± 0.96 | 39.41 ± 0.98 | NR | NR | ①②③④ |
| Liu | 2021 | 53 | 53 | 27.12 ± 3.31 | 26.54 ± 4.52 | NR | NR | 25/28 | 17/46 | ①② |
| Pan | 2015 | 50 | 50 | 25.5 ± 3.2 | 25.5 ± 3.2 | NR | NR | NR | NR | ①② |
| Tong | 2022 | 20 | 20 | 30.63 ± 2.75 | 30.13 ± 2.58 | 39.93 ± 1.86 | 39.82 ± 1.73 | NR | NR | ①②③④ |
| Wang | 2021 | 34 | 34 | 30.1 ± 3.2 | 30.2 ± 3.1 | 39.3 ± 1.0 | 39.2 ± 1.1 | 16/18 | 17/17 | ①② |
| Wen | 2020 | 40 | 40 | 28.84 ± 0.52 | 29.16 ± 0.57 | 38.71 ± 0.25 | 38.22 ± 0.23 | 10/30 | 13/27 | ①② |
| Xu | 2021 | 42 | 42 | 25.5 ± 5.2 | 25.4 ± 5.3 | 39.2 ± 0.6 | 39.3 ± 0.5 | 13/29 | 12/30 | ①②③④ |
| Xu | 2022 | 30 | 30 | 28.54 ± 2.63 | 28.12 ± 2.58 | 39.42 ± 1.01 | 39.54 ± 1.03 | NR | NR | ①②③④ |
| Yu | 2023 | 50 | 50 | 31.26 ± 2.51 | 31.43 ± 2.62 | NR | NR | NR | NR | ①②③④ |
| Zhang(a) | 2021 | 64 | 64 | 28.36 ± 5.47 | 28.58 ± 5.62 | NR | NR | NR | NR | ①②③④ |
| Zhang(b) | 2021 | 30 | 30 | 27.82 ± 3.48 | 27.78 ± 3.58 | 38.67 ± 1.31 | 38.76 ± 1.33 | NR | NR | ①②③④ |
- Note: ① Wound infection; ② complications; ③ self-rating anxiety; ④ self-rating depression.
- Abbreviation: NR, not report.
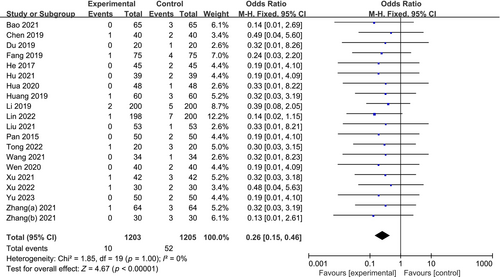
3.3 Wound infection
Wound infection was reported in all 20 included RCTs, including 2408 patients (1203 in the humanised care group and 1205 in the conventional care group). No significant heterogeneity was detected among the studies (p = 1.00, I2 = 0%), and a fixed-effects model was applied. Based on the results, the humanised care group had a significantly lower incidence of postoperative wound infection than the conventional care group (0.83% vs. 4.32%, OR: 0.26, 95% CI: 0.15–0.46, p < 0.00001; Figure 3).
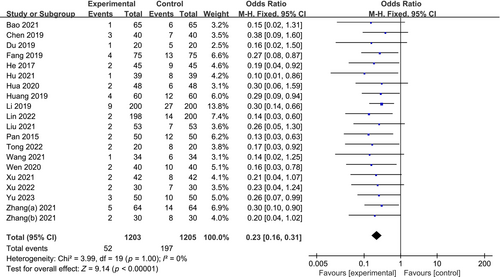
3.4 Complications
All 20 included studies reported complications, including 2408 patients, 1203 in the humanised care group and 1205 in the conventional care group. No significant heterogeneity was detected among the studies (p = 1.00, I2 = 0%), and a fixed-effects model was applied. The results revealed the incidence of postoperative maternal complications was significantly lower in the humanised care group than that in the conventional care group (4.32% vs. 16.35%, OR: 0.23, 95% CI: 0.16–0.31, p < 0.00001; Figure 4).
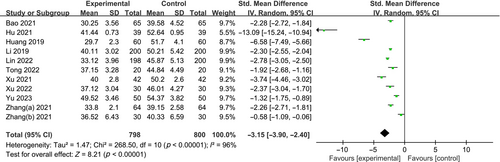
3.5 Self-rating anxiety
Eleven studies reported maternal postoperative SAS scores for 1598 patients (798 and 800 patients in the humanised care and conventional care groups, respectively). Significant heterogeneity was detected among the studies (p < 0.00001, I2 = 96%), and the source of heterogeneity was determined by excluding each study individually. Given that the results did not differ significantly after reanalysis, a random-effects model analysis was applied. Patients who received humanised nursing care had significantly lower postoperative SAS scores than those who received conventional nursing care (SMD: −3.15, 95% CI: −3.90 to −2.40, p < 0.00001; Figure 5).
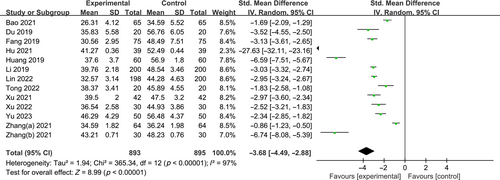
3.6 Self-rating depression
Thirteen studies reported maternal postoperative SDS scores, including 1788 patients, with 893 and 895 patients in the humanised care and conventional care groups, respectively. Significant heterogeneity was detected among the studies (p < 0.00001, I2 = 97%). The results were reanalysed by excluding each study individually, but did not differ significantly; hence, a random-effects model analysis was applied. Patients who received humanised nursing care had significantly lower postoperative SDS scores than those who received conventional nursing care (SMD: −3.68, 95% CI: −4.49 to −2.88, p < 0.00001; Figure 6).
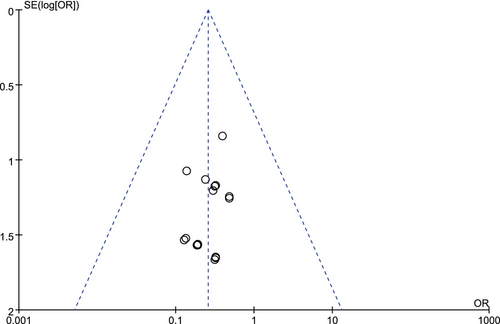
3.7 Publication bias
Considering wound infection as an example for drawing a funnel plot, as shown in Figure 7, the graph is basically symmetrical, indicating poor likelihood of publication. Each study that met the requirements was eliminated individually, and the effect size was reanalysed; the results did not differ significantly, and the conclusion can be considered relatively stable.
4 DISCUSSION
In obstetrics, caesarean section is one of the most common surgical procedures, a process of foetal removal via an abdominal incision through the skin, subcutaneous tissue, fat, muscle and uterine tissues of the pregnant woman's abdomen, layer by layer.31, 32 Caesarean section is a surgical procedure that can improve the outcome of a pregnancy, especially in cases of obstructed labour or complications of pregnancy, and can help to ensure the safety of both the mother and the newborn baby.14, 33 With the continuous advancements in technology, caesarean section has become the preferred method of delivery for women who are unable to have a natural birth.34 However, caesarean section is an unnatural method of delivery that requires an open abdomen and anaesthesia, and is prone to serious complications, including urinary retention, incision infection, abdominal distension and post-partum haemorrhage, delaying the recovery of the body's functions and worsening prognosis.5, 35, 36 Several factors can contribute to high requirements for clinical nursing work, and clinics need to strengthen the nursing care of caesarean section mothers to provide effective nursing interventions. Although conventional nursing provides basic nursing measures, it fails to meet the humanistic care needs of mothers and cannot alleviate adverse emotions; therefore, the quality of postnatal care cannot be effectively improved. Humanised care was first proposed in the United States, through the clinical nursing staff to maternal humanistic care and love, regulating the psychological state of the mother, for a variety of maternal needs, upholding the concept of ‘people-oriented’, from psychological intervention, pain, rehabilitation training and health education, to provide personalised, holistic maternal care. Under this concept, mothers receive personalised, holistic and effective nursing services in terms of psychological intervention, pain, rehabilitation training, health education, to facilitate the process of postoperative rehabilitation, improve prognosis and enhance the nursing effect.20, 37, 38
In the current study, a meta-analysis was conducted to comprehensively assess the effects of humanised care applied to caesarean sections on wound infections. Our results revealed that humanised care following caesarean sections could prevent postoperative wound infections, reduce postoperative complications and help alleviate maternal anxiety and depression. Lin et al. have conducted study to evaluate the application of humanised care during the perioperative period of caesarean section. The authors found a significant reduction in wound infection, along with a lower complication rate, and alleviation of maternal negative emotions; these findings are consistent with our findings.22 Hua et al. assessed 96 mothers and reported a summary analysis of the application of humanised care for caesarean section. The authors found that although humanised care can markedly reduce postoperative complications, there is no statistically significant difference between the two groups in the reduction of postoperative wound infections, a finding that contradicts the results of our findings.18 According to Huang et al. and Tong et al., although humanised care could substantially reduce the incidence of postoperative complications, it failed to significantly reduce the incidence of wound infections.19, 24 Zhang et al. analysed the effect of humanised care among 60 mothers who underwent caesarean section and concluded that humanised care could substantially reduce the incidence of postoperative wound infections, reduce postoperative complications and improve maternal anxiety and depression, reinforcing the advantages of humanised care during postoperative maternal care.30
Nevertheless, the limitations of the current study need to be addressed: (1) certain included studies had a small sample size, and the study populations were from China, which may have resulted in selection bias; (2) most included articles did not refer to the implementation of allocation concealment and blinding, and some employed incorrect grouping methods; and (3) given that humanised care interventions tended to differ across studies, there may have been a bias in the findings, potentially impacting the objectivity of the findings.
5 CONCLUSION
Compared with conventional care, humanised care can prevent wound infection after caesarean section, reduce postoperative complications and alleviate maternal anxiety and depression, which are worthy of clinical promotion and application. However, given the low quantity and quality of the included literature, multicentre RCTs that include a larger population are warranted to further validate the results of this study.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




