RETRACTED: Efficacy of anti-vascular endothelial growth factor and mitomycin C on wound healing after trabeculectomy in glaucoma patients: A meta-analysis
Abstract
Trabeculectomy is the main surgical treatment for glaucoma, but scar formation during wound healing may lead to surgical failure. In this study, we evaluated the efficacy of anti-vascular endothelial growth factor (anti-VEGF) and mitomycin C (MMC) on wound healing after glaucoma surgery. We have been looking for Pubmed, Embase and other databases. The last time we looked at an electronic database was August 2023. A case control study was conducted to compare the use of anti-VEGF and mitomycin C for the treatment of glaucoma. We used the Cochrane standard methodology for collecting and analysing the data. Based on the criteria of inclusion, we have determined 369 related papers and selected seven eligible trials for data analysis. Three hundred and twenty-six cases were treated with trabeculectomy, of which 166 were injected with anti-VEGF and 160 were given MMC for trabeculectomy. In six trials, anti-VEGF and MMC were not found to have any statistical significance on postoperative wound leakage after surgery (OR, 1.55; 95% CI, 0.71, 3.35 p = 0.27). The three trials showed that anti-VEGF and MMC did not differ in terms of reducing postoperative wound hypotony after surgery (OR, 0.78; 95% CI, 0.20, 3.11 p = 0.73). Five trials demonstrated that anti-VEGF and MMC were not associated with a lower incidence of shallow anterior chamber (OR, 1.17; 95% CI, 0.5, 2.76 p = 0.71). There is no significant difference in the effect of anti-VEGF and MMC on wound healing after glaucoma surgery. A multicentre randomized controlled trial with a larger sample size is needed to confirm this study.
1 INTRODUCTION
Glaucoma is a diverse set of conditions which, if left untreated, may result in progressive optic nerve damage and permanent blindness. It is one of the main reasons for irreversible blindness worldwide, and it has an impact on many people worldwide. Over 8 million of them have bilateral blindness.1 Elevation of IOP is one of the main risk factors for glaucoma.2, 3 In a published meta-analyses of studies, it was found that a reduction in IOP may help to decrease the risk of long-term vision loss in the long term.4
Glaucoma filtering operation is one of the most common IOP-lowering treatments in glaucoma. In a review of the efficacy of both operative and pharmacological therapies for glaucoma, it was shown to be significantly superior to drug therapy in reducing IOP, though it has not been shown to be linked to reduced vision deterioration.5 The fundamental principle of glaucoma filtering operation is to form a drainage path from the anterior chamber to the lower conjunctiva through the atrium. Nevertheless, scarring in the filter zone can cause limited water flow across the filter bubble, which makes it less effective in reducing the internal pressure. In a retrospective cohort study of patients who had been treated with trabeculectomy, a 20 year success was about 60% for trabeculectomy without topical drugs.6 To decrease the occurrence of scar after operation, MMC and 5-Fluorouracil(FU) have been extensively applied to suppress the growth of fibroblast activity.7, 8 But because of their non-specific mechanism of action, MMC and 5-FU may result in widespread cellular death, resulting in vision threats, including eye-low-pupil squint, bubble leak and broad-related endophthalmitis.9-12 While anti-metabolites may lower the chances of surgery for non-operative eyes and for those who are at greater risk for surgery because of filter failure, there are a number of cases that need supportive treatment. In a multi-centre study in which patients with glaucoma who had previously undergone cataract removal in combination with an artificial lens implant, a failed filter operation or a combination of two nondrug-controlled procedures, the cumulative odds of failure in MMC-treated glaucoma were nearly one half over 5 years of follow up.7, 8, 13 Thus, there is a need for an alternate physiological anti-metabolite.
VEGF is one of the most important components of angiogenic and vascular heredity.14 Ranibizumab is a recombinant human monoclonal antibody that neutralizes all the VEGF-A activity.15 Bevacizumab is a recombinant, whole-body, humanized antibody that has been successfully applied to treat multiple malignancies.16-19 A number of recent researches have suggested that the use of anti-VEGF as an adjunct to trabeculectomy may decrease the occurrence of post-trabeculectomy.9, 20, 21
How Intervention May Work Wound healing involves multiple pathways, such as angiogenesis and fibroblast proliferation.22, 23 VEGF is responsible for the stimulation of wound healing by various mechanisms.24 VEGF-mediated angiogenic activity is crucial for wound healing by enabling the migration of inflammation and fibroids into the wound, thereby creating a vessel framework for granulating tissue formation.25 Recently, VEGF receptors have been found to be a key facilitator for the development of scar tissue following filtering surgery.14 Following the operation of glaucoma, the expression of VEGF was elevated and the growth of fibroblast was stimulated. Anti-VEGF antibodies decrease postsurgical scar formation by suppressing angiogenesis, but they can also suppress the growth of fibroblast and cause fibroblast death.12
The development of scar tissue is the main reason for the failure of the blister following trabeculectomy, which influences the long-term success. Recent research has shown that anti-VEGF medicines are likely to be a option, and there has been an increase in the use of VEGF agents during glaucoma operations. The purpose of this study was to evaluate the effect of anti-VEGF and MMC on the wound heal outcome of trabeculectomy.
2 METHODS
2.1 Literature search
An overall review of the literature was carried out by two independent authors. The search period included all available records in each database up to August 2023. Both the title and the free text are combined in the document search. The search policy is illustrated in Table 1. Furthermore, the reference lists for the included trials have been revised in order to complement the related literature.
| No. | Query |
|---|---|
| #1 | Glaucoma[Title/Abstract] OR Trabeculectom*[Title/Abstract] OR Filter*[Title/Abstract] OR Filtrat*[Title/Abstract] OR Drain*[Title/Abstract] |
| #2 | Endothelial growth factor[Title/Abstract] OR VEGF[Title/Abstract] OR Angiogenesis inhibitors[Title/Abstract] OR Angiogenesis inducing agents[Title/Abstract] OR Macugen[Title/Abstract] OR Lucentis[Title/Abstract] OR Rhufab[Title/Abstract] OR Avastin[Title/Abstract] OR Aflibercept[Title/Abstract] OR Bevacizumab[Title/Abstract] OR Ranibizumab[Title/Abstract] OR Pegaptanib[Title/Abstract] OR Brolucizumab[Title/Abstract] OR Conbercept[Title/Abstract] |
| #3 | Mitomycin*[All Fields] OR Mytomycin*[All Fields] OR Mitomicin*[All Fields] OR Mytomicin*[All Fields] OR MMC[All Fields] |
| #4 | #1 AND #2 AND #3 |
2.2 Data collection
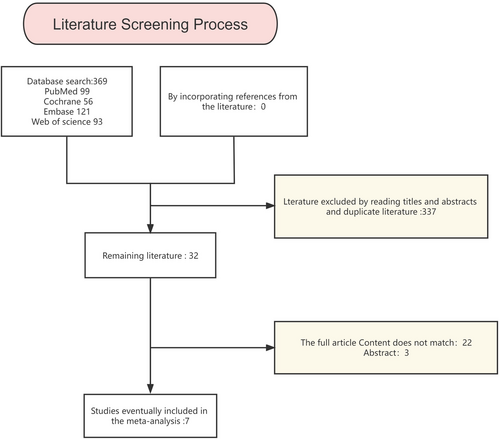
Due to the widespread use of trabeculectomy for glaucoma and the fact that anti-VEGF drugs are believed to delay the development of postoperative scar tissue, we compared the efficacy of drugs that were routinely administered with trabeculectomy. Linguistic constraints have not been taken into account during the screening and selection of tests. There was no limitation on the possible sample size of the exams recruited. The selection process is shown in Figure 1.
2.3 Criteria
Inclusion Criteria: Patients who have been treated with trabeculectomy; and anti-VEGF and MMC are compared during the operation.
Exclusion Criteria: Non-trabeculectomy studies. No clinical trials have been conducted to compare anti-VEGF or MMC injury results. Studies published in conferences and for which the complete text was not available were also excluded.
2.4 Data extraction and quality assessment
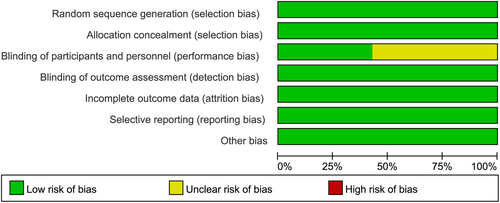
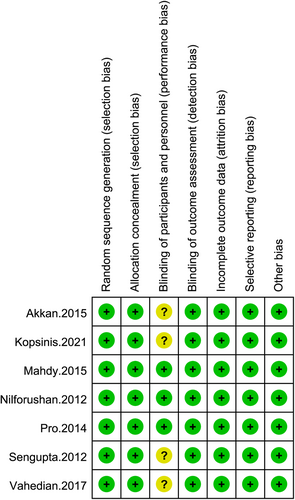
Both investigators carried out independent review of the documents and extracted the data with strict cross-validation of the inclusion and exclusion criteria. The disagreement was settled by discussion. Data were obtained for each trial: the first author, the date of release and the age. The study was evaluated for its methodology by means of the RONINS-I risk-of-error evaluation instrument. The results of each of these trials were rated as ‘Low Risk’, ‘Moderate Risk’, ‘Serious Risk’, ‘Critical Risk’ or ‘No Information’.
2.5 Statistical analyses
A meta-analysis was conducted with Revman 5.3, and a ratio (OR) with 95% confidence limits (CI) was employed as an effect measure. Heterogeneity was evaluated with I2. When I2 is <50% or p > 0.1, this suggests that there is little diversity and the fixed effect model is applied. A random-effect model is employed if I2 >50% or p < 0.1, suggesting highly heterogeneous. The publication bias was assessed using the Egger test and funnel plots. Statistical significance was found to be p < 0.05.
3 RESULTS
3.1 Study characteristics
Following a survey, we found 369 related papers and selected seven qualified ones to be analysed according to the eligibility criteria. From 2012 to 2021, 326 patients were treated with trabeculectomy, of whom 166 received anti-VEGF and 160 received MMC. The features of glaucoma are presented in Table 2. A qualitative evaluation of the seven enrolled trials is shown in Figures 2 and 3.
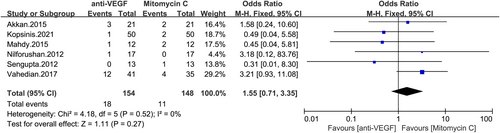
3.2 Wound leakage
The impact of anti-VEGF or MMC on postoperative wound leakage was investigated in six trials. A fixed effect model was used to analyse the data, and as shown in Figure 4, there were no statistically significant differences in the rate of wound leakage after surgery (OR, 1.55; 95% CI, 0.71–3.35 p = 0.27).
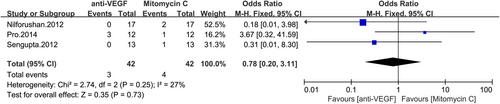
3.3 Hypotony
The effectiveness of anti-VEGF and MMC in the treatment of postoperative hypotony was investigated in three trials. Figure 5 shows no significant difference in the postoperative hypotony of the anti-VEGF group compared to the MMC group (OR, 0.78; 95% CI, 0.20–3.11 p = 0.73).
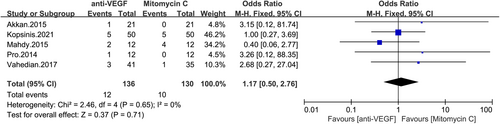
3.4 Shallow anterior chamber
Five studies demonstrated that anti-VEGF and MMC were associated with incidence of shallow anterior chamber in postsurgical trabeculectomy patients. Figure 6 shows that the anti-VEGF and MMC groups did not differ significantly in the risk of formation of a shallow anterior chamber after surgery.
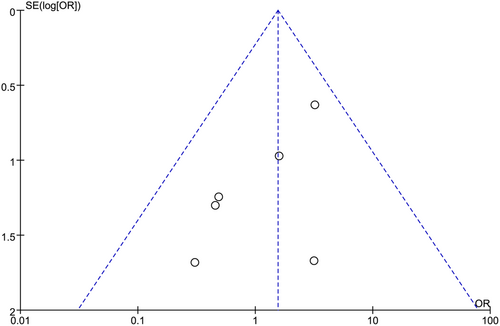
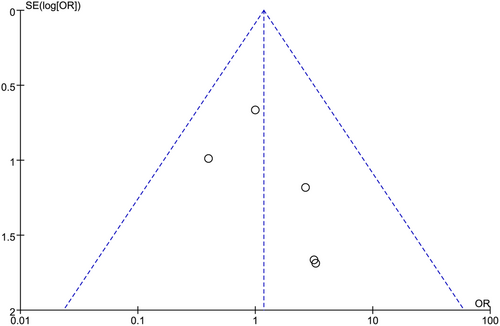
3.5 Publication bias
The publication bias has been analysed in clinical trials regarding the incidence of wound leak and shallow anterior chamber following anti-VEGF or MMC administration in trabeculectomy patients, as illustrated in Figures 7 and 8.
4 DISCUSSION
The main barrier to successful surgery after trabeculectomy is the formation of scar tissue in the conjunctiva, the Tenon capsule and the interocular membrane due to the natural wound healing reaction in surgery. Excessive scarring after surgery results in a bubble collapse that hinders the development of the condition because of inadequate IOP control. Existing anti-scarring drugs like 5-FU and MMC have been shown to decrease the occurrence of scar tissue following surgical operations and to enhance the outcome of cataract operations. Currently, the majority of glaucoma surgeons are applying anti-fibrosis drugs to patients who have been treated with trabeculectomy, which is based on the fact that they have improved IOP control, thereby reducing the incidence of postoperative injuries.
The results of this study were compared between anti-VEGF and MMC injections after the operation. The evaluation and comparison of postoperative complications were carried out with a generally agreed methodology. We have shown that the use of anti-VEGF in addition to trabeculectomy offers at least the same level of postoperative complications as MMC in comparison with traditional MMC use.
In this trial, a total of 369 related scientific publications were found, and seven qualifying trials were selected to be analysed according to the classification criteria. Three hundred and twenty-six subjects received trabeculectomy, 166 of whom received anti-VEGF and 160 received MMC under conjunctiva. In six trials, anti-VEGF and MMC were not significantly different from those treated with trabeculectomy. No statistical difference was found in the absence of a leak in the skin, and the results of the three trials showed that there was no difference in anti-VEGF or MMC in the treatment of postoperatively hypotonicity of the patients with trabeculectomy. Five trials demonstrated that anti-VEGF or MMC was not associated with the risk of superficial anterior chamber in the postoperation phase of trabeculectomy.
The limitations of this research are the comparatively small number of the published papers, as well as the absence of any hidden data from the group allocation. That is because it would be hard to finish. A larger sample size is required to reduce the variance due to other factors. In addition, there are individual factors that influence the wound healing and hence the surgery results. Moreover, the majority of these trials did not cover up the fact that physicians had nothing to do with surgery. This may have contributed to bias. We compared the efficacy of anti-VEGF agents to MMC trabeculectomy as described above. Our findings offer a few indications for the efficacy of anti-VEGF agents in trabeculectomy. In order to learn more about these issues, research is required to look at how anti-VEGF agents work as wound modification agents in a larger sample.
5 CONCLUSION
In this meta-analysis, anti-VEGF and MMC were used to evaluate the impact of postoperative treatment on the postoperative recovery of patients with trabeculectomy. No significant differences were found in anti-VEGF versus MMC in the incidence of wound leak after surgery, hypotony and shallow anterior chamber in trabeculectomy patients. Clinically, there seems to be no significant difference between anti-VEGF injection and MMC in postoperative wound healing in trabeculectomy patients.
ACKNOWLEDGEMENT
We thank Prof. Liu for his review of this study and suggestions for revisions.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request from the authors.




