RETRACTED: A meta-analysis evaluating wound infections and other complications following distal versus complete gastrectomy for gastric cancer
Abstract
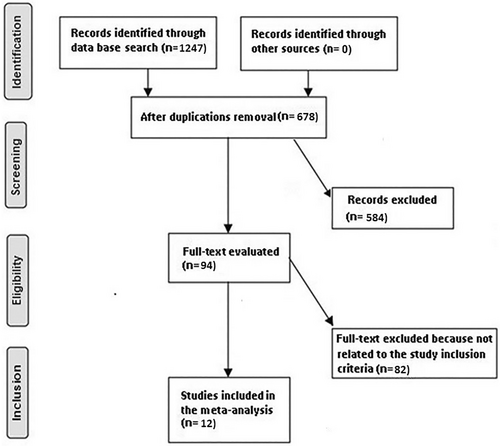
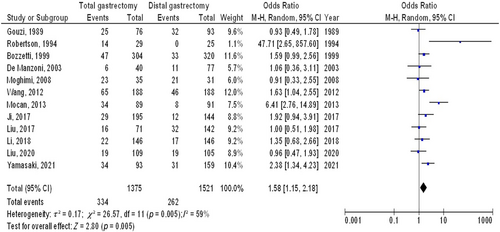
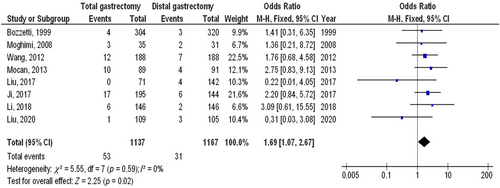
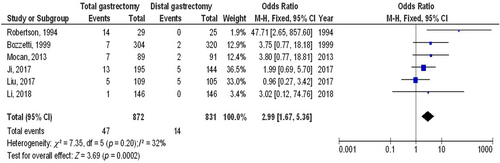
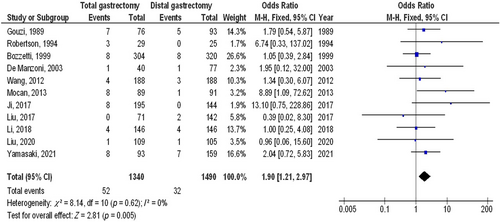
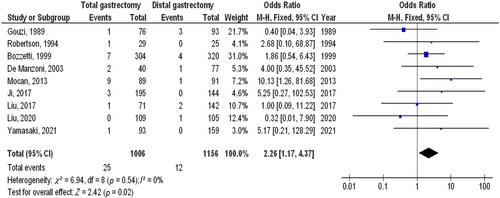
A meta-analysis investigation was carried out to measure the wound infections (WIs) and other postoperative problems (PPs) of distal gastrectomy (DG) compared with total gastrectomy (TG) for gastric cancer (GC). A comprehensive literature investigation till February 2023 was used and 1247 interrelated investigations were reviewed. The 12 chosen investigations enclosed 2896 individuals with GC in the chosen investigations' starting point, 1375 of them were TG, and 1521 were DG. Odds ratio (OR) in addition to 95% confidence intervals (CIs) were utilized to compute the value of the WIs and other PPs of DG compared with TG for GC by the dichotomous approaches and a fixed or random model. TG had significantly higher overall PP (OR, 1.58; 95% CI, 1.15–2.18, p = 0.005), WIs (OR, 1.69; 95% CI, 1.07–2.67, p = 0.02), peritoneal abscess (PA) (OR, 2.99; 95% CI, 1.67–5.36, p < 0.001), anastomotic leakage (AL) (OR, 1.90; 95% CI, 1.21–2.97, p = 0.005) and death (OR, 2.26; 95% CI, 1.17–4.37, p = 0.02) compared to those with DG in individuals with GC. TG had significantly higher overall PP, WIs, PA, AL and death compared to those with DG in individuals with GC. However, care must be exercised when dealing with its values because of the low sample size of some of the nominated investigations for the meta-analysis.
1 INTRODUCTION
The second biggest cause of cancer-related fatalities in China is gastric cancer (GC), which is a global health problem.1 The cornerstone of radical resection of possibly curable GC is still surgical resection with appropriate peri-gastric lymphadenectomy.2 The degree of gastrectomy required for the curative management of GC is based on a careful evaluation of the tumour's location, size and the surgeon's training.3 The best degree of resection for GC that has spread to the middle or lower third of the stomach is still up for debate. Because it may increase long-term survival and reduce the occurrence of gastric residual cancer, total gastrectomy (TG) has been suggested as the standard surgery in some investigations.4 When intraoperative, short-term and quality-of-life outcomes are taken into account, some investigations found that distal gastrectomy (DG) is preferable to whole gastrectomy.5 A meta-analysis comparing the viability and safety of whole gastrectomy against DG for distal GC was published in recent years, although there were discrepancies between the findings for postoperative problems (PP) and survival outcomes in these investigations.6 While this is going on, several investigations that were included in the earlier meta-analysis did not explicitly identify where the tumour was located, and some instances with tumours in the upper third of the stomach might also be included in these meta-analyses. The aforementioned issues could make their article less persuasive. Additionally, a number of investigations comparing TG with DG for the management of GC have been published this year. In order to pool information from all currently available investigations, a thorough systematic review and meta-analysis must be conducted using more logical inclusion criteria. In order to compare the safety and long-term prognosis of DG with TG for GC, this investigation revised a previous meta-analysis with more evidence. In order to compare TG with DG, a meta-analysis was carried out with the aim to compare the wound infections (WIs) and other PPs of DG compared with TG for GC.
2 METHODS
2.1 Eligibility criteria
For the purpose of creating a summary, the investigations demonstrating the WIs and other PPs of DG compared with TG for GC were chosen.7
2.2 Information sources
- The research was an observational, prospective, retrospective or randomized controlled trial (RCT) investigation.
- Individuals with GC were the investigated chosen individuals.
- The intervention incorporated gastrectomy.
- The investigation distinguished the effect of TG and DG in the management of GC on WI and other PPs.
The research was excluded if the significance of the comparison was not emphasized in it, investigations that did not check the characteristics of the WIs and other PPs of DG compared with TG for GC, and research on overall PPs in individuals without TG and DG.10-12
2.3 Search strategy
Search protocol operations were recognized depending on the PICOS opinion, and we characterized it as next: ‘population’ for individuals with GC, P; gastrectomy is the ‘intervention’ or ‘exposure’, while the ‘comparison’ was between TG and DG; PP, WIs, peritoneal abscess (PA), anastomotic leakage (AL) and death was the ‘outcome’ and last of all, ‘investigation design’ the proposed investigation had no restrictions.13
We searched Google Scholar, Embase, the Cochrane Library, PubMed and OVID databases exhaustively till February 2023 utilizing an organization of keywords and accompanying terms for gastric cancer; total gastrectomy; distal gastrectomy; overall postoperative problem; and wound infection as shown in Table 1. To avoid research that failed to establish a link between the consequences of WIs and other PPs of DG compared with TG for GC, paper replications were removed, they were grouped into an EndNote file and the titles and abstracts were reevaluated.14
| Database | Search strategy |
|---|---|
| Pubmed | #1 ‘gastric cancer’[MeSH Terms] OR ‘wound infection’[MeSH Terms] OR ‘distal gastrectomy’[All Fields] [All Fields] |
| #2 ‘overall postoperative problem’[MeSH Terms] OR ‘total gastrectomy’[MeSH Terms] [All Fields] | |
| #3 #1 AND #2 | |
| Embase | ‘gastric cancer’/exp OR ‘wound infection’/exp OR ‘distal gastrectomy’ |
| #2 ‘overall postoperative problem’/exp OR ‘total gastrectomy’ | |
| #3 #1 AND #2 | |
| Cochrane Library | (gastric cancer): ti,ab,kw (wound infection):ti,ab,kw (distal gastrectomy):ti,ab,kw (Word variations have been searched) |
| #2 (overall postoperative problem):ti,ab,kw OR (total gastrectomy):ti,ab,kw (Word variations have been searched) | |
| #3 #1 AND #2 |
2.4 Selection process
Following the epidemiological declaration, a process was formed, which was then organized and analysed in the procedure of a meta-analysis.
2.5 Data collection process
Among the criteria utilized to collect data were the name of the first author, the investigation date, the year of the investigation, the country or area, the population type, the medical and therapy physiognomies, categories, the quantitative and qualitative estimate process, the data source, the consequence estimate and statistical analysis.15
2.6 Data items
Whenever an investigation had variable values, we separately acquired the data based on an evaluation of the WIs and other PPs of DG compared with TG for GC.
2.7 Investigation risk of bias assessment
Two authors independently estimated the procedure of the selected publications to see whether there was a possibility that each investigation may have been biased. The procedural quality was estimated utilizing the ‘risk of bias instrument’ from the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. After being categorized by the appraisal criteria, each investigation was allocated one of the next bias risks: low—An investigation was categorized as having a low bias risk if all of the quality criteria were met; an investigation was categorized as having a medium bias risk if one or more requirements were not met or were not encompassed. The investigation was deemed to have a significant bias risk if one or more quality needs were either completely or just partially not met.
2.8 Effect measures
Sensitivity analyses were only carried out on research that assessed and documented the WIs and other PPs of DG compared with TG for GC. To compare TG to DG GC individuals' sensitivity, a subclass analysis was utilized.
2.9 Synthesis methods
A random- or fixed-effect model was utilized to generate the odds ratio (OR) and a 95% confidence interval (CI) utilizing dichotomous or continuous approaches. Between 0 and 100%, the I2 index was determined. The values at 0%, 25%, 50% and 75%, respectively, presented no, low, moderate and high heterogeneity.16 Other features that show a strong degree of alikeness amongst the related research were also analysed to make sure the correct model was being utilized. The random effect was used if I2 was 50% or above; if I2 was <50%, the possibility of utilizing fixed-effect rose.16 A subclass analysis was done by stratifying the initial estimation by the aforementioned consequence groups. A p-value of <0.05 was utilized in the analysis to specify the statistical significance of differences between subcategories.
2.10 Reporting bias assessment
Investigations bias was measured statistically and qualitatively utilizing the Egger regression test and funnel plots that exhibit the logarithm of the ORs versus their standard errors (investigations bias was deemed existing if p ≥ 0.05).17
2.11 Certainty assessment
Two-tailed testing was utilized to investigate each p-value. The graphs and statistical evaluations were generated utilizing Reviewer Manager Version 5.3. (The Nordic Cochrane Centre, the Cochrane Collaboration, Copenhagen, Denmark).
3 RESULTS
Twelve publications, published between 1989 and 2021, from a total of 1247 connected investigations that met the inclusion criteria were chosen for the investigation.18-29 The results of these researches are presented in Table 2. A total of 2896 individuals with GC were in the chosen investigations' starting point, 1375 of them were TG, and 1521 were DG. The sample size was between 54 and 624 individuals.
| Investigation | Country | Total | TG | DG |
|---|---|---|---|---|
| Gouzi, 198918 | France | 169 | 76 | 93 |
| Robertson, 199419 | China | 54 | 29 | 25 |
| Bozzetti, 199920 | Italy | 624 | 304 | 320 |
| De Manzoni, 200321 | Iran | 117 | 40 | 77 |
| Moghimi, 200822 | Iran | 66 | 35 | 31 |
| Wang, 201223 | China | 376 | 188 | 188 |
| Mocan, 201324 | Romania | 180 | 89 | 91 |
| Ji, 201725 | China | 339 | 195 | 144 |
| Liu, 201726 | China | 213 | 71 | 142 |
| Li, 201827 | China | 292 | 146 | 146 |
| Liu, 202028 | China | 214 | 109 | 105 |
| Yamasaki, 202129 | Japan | 252 | 93 | 159 |
| Total | 2896 | 1375 | 1521 |
TG had significantly higher overall PP (OR, 1.58; 95% CI, 1.15–2.18, p = 0.005) with moderate heterogeneity (I2 = 59%), WIs (OR, 1.69; 95% CI, 1.07–2.67, p = 0.02) with no heterogeneity (I2 = 0%), PA (OR, 2.99; 95% CI, 1.67–5.36, p < 0.001) with low heterogeneity (I2 = 32%), AL (OR, 1.90; 95% CI, 1.21–2.97, p = 0.005) with no heterogeneity (I2 = 0%) and death (OR, 2.26; 95% CI, 1.17–4.37, p = 0.02) with no heterogeneity (I2 = 0%) compared to those with DG in individuals with GC as shown in Figures 2-6.
The lack of data prevented stratified models from being utilized to inspect the effects of particular factors, for example, age, gender and ethnicity, on comparison outcomes. No evidence of investigation bias was found (p = 0.84) operating the quantitative Egger regression test and the visual interpretation of the funnel plot. The mainstream of the implicated RCTs, though, were found to have poor procedural quality and no bias in selective reporting.
4 DISCUSSION
In investigations that were considered for the meta-analysis, 2896 individuals with GC were in the chosen investigations' starting point, 1375 of them were TG, and 1521 were DG.18-29 TG had significantly higher overall PP, WIs, PA, AL and death compared to those with DG in individuals with GC. However, care must be exercised when dealing with its values caused by the low sample size of some of the nominated investigations (2 out of 12 ≤ 100 individuals) for the meta-analysis. That would affect the level of significance of the evaluations studied.
The cornerstone of curative therapy for possibly curable GC is surgical resection with appropriate peri-gastric lymph node dissection. The best surgical approach should focus on the curative resection of the tumour with a low risk of problems and death, giving the individual a better long-term outlook and excellent quality of life.25 The acknowledged standard at this time is D2 lymph node dissection.3 Regarding the optimal gastrectomy extent for middle and lower third GC, there is still disagreement. An essential consideration when assessing the safety and technical viability of surgical treatment is PPs. PPs often led to lengthier hospital stays and higher hospital costs.30 The comparison results for PPs in this meta-analysis are not uniform across all trials. According to Ji et al., the whole gastrectomy group experienced more PPs than the DG group.25 Recently, a well-matched investigation to assess the PPs using the Clavien-Dindo classification system discovered no statistically significant differences between the whole and DG groups in terms of overall and major problem rates.27 Regarding lymph node dissection and reconstruction following gastrectomy, whole gastrectomy is thought to be more challenging and technically demanding than DG.31 Our meta-analysis showed that the whole gastrectomy group had a greater rate of overall PPs and death than the DG group. Furthermore, Lee et al.'s investigation revealed that TG was a substantial independent risk factor for general and severe problems.32 Anastomotic leaking continues to be one of the most significant and occasionally fatal problems despite advancements in surgical technique and postoperative care, with a reported prevalence of 0%–15%.33 When it comes to a specific consequence, earlier research has shown that whole gastrectomy is linked to a larger AL rate than DG.25, 34 The rate of AL, WIs and PA is higher in the whole gastrectomy group than in the DG group, according to assessments of specific problems in the current investigation. The use of minimally invasive surgery to treat early-stage and locally progressed GC has been demonstrated in an increasing number of trials in recent years.35 Laparoscopy-assisted entire gastrectomy is still more technically difficult than laparoscopy-assisted DG (laparoscopy-assisted TG) because of the need for an esophagojejunostomy.36 Additionally, because of the small operating room and the deep anastomosis position, intracorporeal esophagojejunostomy is more challenging to perform, particularly on obese individuals.37 According to Kim et al., when compared to laparoscopically assisted TG, the incidence of AL was considerably greater with TG.34 Anastomotic leaking was discovered to be more frequent, but not significantly so, in cases of LA complete gastrectomy by Lin et al. and Li et al.27, 38 Two important metrics for determining an individual's prognosis are long-term survival and the likelihood of cancer recurrence. Based on the information at hand, our findings indicated that the DG group's 5-year overall survival rate was higher than that of the whole gastrectomy group for all individuals. In a recent meta-analysis, when the 5-year overall survival rate was evaluated, a tendency in favour of DG was found.39 But the included research does not all support this outcome. DG and complete gastrectomy both had comparable long-term survival results, according to Gouzi et al.18 and Bozzetti et al.20 However, Lee et al.40 and Mocan et al.24 discovered that the DG had considerably greater 5-year overall survival rates than the entire gastrectomy. In a large-scale case–control investigation, Liu et al. discovered that the 5-year overall survival rate of the whole gastrectomy was lower than that of DG.26
This meta-analysis confirmed the impact of TG and DG on the management of GC on WI and other PPs.41-44 More investigation is still desirable to clarify these feasible influences. This was also emphasized in former investigations that utilized a related meta-analysis procedure and originated equivalent values of the impact.45-48 Although the meta-analysis was incapable to discover if differences in these characteristics are related to the outcomes being researched, properly led RCTs are vital to consider these aspects as well as the mixture of different ages, gender and ethnicities of individuals. In conclusion, TG had significantly higher overall PP, WIs, PA, AL and death compared to those with DG in individuals with GC.
5 LIMITATIONS
Since some of the investigations involved in the meta-analysis were not included, there might have been selection bias. The omitted publications, however, did not fulfil the necessities for inclusion in the meta-analysis. Also, we lacked the expertise to determine whether factors like age and ethnicity influenced results. The drive of the investigation was to measure the effect of TG and DG on the management of GC on overall PP and WI. Bias may have grown because incomplete or incorrect data from earlier research were included. Possible sources of bias involved the individuals' nutritional status in addition to their race, gender and age. Unwantedly, incomplete data and certain unpublished work may distort the value that is being examined.
6 CONCLUSIONS
TG had significantly higher overall PP, WIs, PA, AL and death compared to those with DG in individuals with GC. However, care must be exercised when dealing with its values caused by the low sample size of some of the nominated investigations (2 out of 12 ≤ 100 individuals) for the meta-analysis. That would affect the level of significance of the evaluations studied.
ACKNOWLEDGEMENTS
The authors would like to thank the Deanship of Scientific Research at Shaqra University for supporting this work.
FUNDING INFORMATION
Deanship of Scientific Research at Shaqra University.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
On request, the corresponding author is required to provide access to the meta-analysis database.




