RETRACTED: The impact of psychological interventions on surgical site wound healing post-surgery in psoriasis patients: A meta-analysis
Na Wang and Lin Pei contributed equally to this work.
Abstract
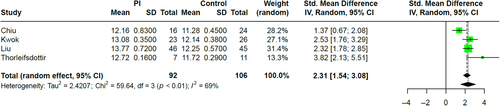
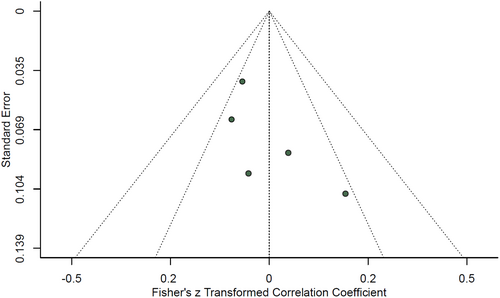
This meta-analysis investigates the impact of psychological interventions on the wound healing process at surgical sites in patients with psoriasis who have undergone various surgical procedures. Following the PRISMA guidelines, an extensive database search was conducted, initially identifying 679 articles, with 6 studies ultimately meeting our rigorous selection criteria. These studies, which included both Randomized Controlled Trials and observational designs, utilized a range of scales, such as the REEDA and Manchester Scar Scale (MSS), to measure the healing of surgical wounds. Statistical analyses were performed using Review Manager and SPSS, revealing that psychological interventions significantly expedited wound healing as early as 1 week post-surgery (I2 = 93%; Random: SMD = −3.01, 95% CI: [−4.35, −1.66], p < 0.01), according to the REEDA scale. At the one-month follow-up, a continued positive effect was observed on the MSS (I2 = 69%; Random: SMD = 2.31, 95% CI: [1.54, 3.08], p < 0.01). The studies demonstrated a low risk of bias, and funnel plot analysis suggested no significant publication bias. These results highlight the beneficial role of psychological support in the postoperative recovery of psoriasis patients, suggesting a need for a more integrated approach to patient care that includes psychological well-being as a component of comprehensive treatment strategies.
1 INTRODUCTION
Psoriasis is a chronic inflammatory skin disorder that affects millions worldwide, characterized by the rapid proliferation of skin cells resulting in red, scaly patches on the skin.1 Beyond its physical manifestations, psoriasis patients often suffer from significant psychological distress, including anxiety, depression, and a diminished quality of life.2 The emotional challenges faced by these individuals can be further intensified when surgical procedures are required.3
The intricate relationship between the mind and body has been a topic of interest in medical literature for decades.4 A growing body of evidence suggests that psychological states can profoundly influence physiological processes, including wound healing.5 Various psychological interventions, such as cognitive-behavioural therapy, relaxation techniques, and mindfulness-based stress reduction, have demonstrated efficacy in diverse medical contexts, promoting faster recovery post-surgery.6 For psoriasis patients, where psychological distress and physical symptoms are inherently intertwined, these interventions could be of pivotal importance.7
While emerging research underscores the potential benefits of psychological interventions for psoriasis patients post-surgery, the literature remains fragmented.8 A consolidated understanding, drawing from multiple studies, can provide a clearer perspective on this relationship.
In the light of the above, this meta-analysis endeavours to offer a comprehensive review and synthesis of existing literature on the impact of psychological interventions on post-surgical wound healing in psoriasis patients. By doing so, we aim to provide a clearer roadmap for clinicians and healthcare professionals, advocating for more holistic post-surgical care.
2 MATERIALS AND METHODS
2.1 Search strategy
To capture a comprehensive spectrum of studies pertinent to the topic, we designed a systematic search blueprint, in adherence to the PRISMA guidelines. Notable databases, such as PubMed, Scopus, Cochrane Library, and Google Scholar, were interrogated. Keywords tailored to our theme, including ‘psychological interventions’, ‘psoriasis’, ‘post-surgical’, and ‘wound healing’, were amalgamated to ensure no critical study was overlooked. The time frame was set to consider articles penned in English till September 2023. The initial sift involved examining titles and abstracts for contextual alignment, followed by a detailed assessment of potential full texts to delineate their suitability for our meta-analysis.
2.2 Selection criteria
Studies considered apt for our meta-analysis were either RCTs or bore an observational architecture with a focus on psoriasis-afflicted patients. These works would probe into the role of psychological interventions on post-surgical recovery metrics in the said patients. Established clinical markers, like the Surgical Wound Healing Score (SWHS), Vancouver Scar Scale (VSS), Manchester Scar Scale (MSS), Patient and Observer Scar Assessment Scale (POSAS), Wound Healing Index (WHI), and the Redness, Edema, Ecchymosis, Discharge, and Approximation (REEDA) scale, were fundamental for study inclusion. Only manuscripts scripted in English found a place in our review. Articles were sidelined if they manifested ambiguity, lacked a comparative backdrop, existed as reviews or case studies, or strayed from our core theme.
2.3 Data extraction process
A standard data extraction blueprint was put to work, ensuring parity across the board for all chosen studies. This phase was helmed by two autonomous reviewers, with any divergence in opinion being settled through dialogue or, if needed, a third reviewer was invoked. Vital information such as the primary author, year of dispatch, study framework, its span, and expansive patient statistics were diligently amassed. In the case of RCTs, intricate details about the therapeutic interventions and the essence of the control group were documented. Outcome measures, both primary and secondary, were extracted, with a keen eye on post-surgical metrics like SWHS, VSS, MSS, POSAS, and REEDA et al.
2.4 Bias risk appraisal
Employing the Cochrane Collaboration's evaluative matrix, we discerned the inherent bias risk in each selected study. Critical facets, including randomization procedures, masking strategies, data inclusiveness, and reporting transparency, were thoroughly examined.
2.5 Statistical analysis
To bolster our meta-analysis, we harnessed statistical platforms like Review Manager (RevMan) and SPSS. All conclusive statistical outputs were two-directional, with a significance cap set at a p-value less than 0.05. Continuous data were explored using either the mean difference (MD) or the standardized mean difference (SMD) backed by 95% CIs. The I2 statistic was deployed to gauge inter-study variance, and in cases where this exceeded 50%, a mixed-effects model was adopted. Lastly, potential publication bias was addressed using funnel plots and the Begg-Mazumdar correlation.
3 RESULTS
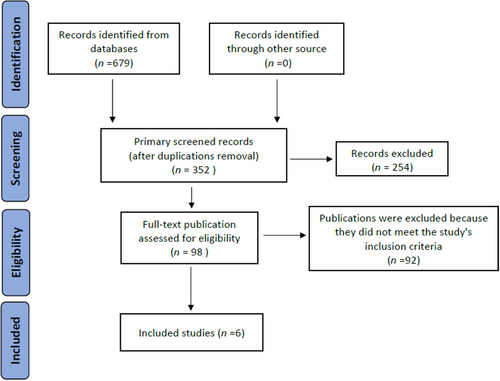
Our exhaustive literature search initially identified 679 records. Rigorous removal of duplicates reduced this number to 352 records eligible for screening. A stringent two-tiered exclusion process then followed: 254 records were first excluded on the basis of title and abstract assessments, subsequently followed by the exclusion of an additional 92 records upon detailed full-text review for not conforming to the pre-established inclusion criteria. The outcome of this process was the careful selection of 6 key studies9-14 for inclusion in our meta-analysis, as depicted in Figure 1. A comprehensive overview of the study characteristics and surgical site wound healing metrics is presented in Table 1.
| First Author | Year | Country | Psychological interventions | Age (years) | Sample size | Measures | |
|---|---|---|---|---|---|---|---|
| PI | Control | ||||||
| Bakkour | 2016 | United Kingdom | Cognitive Behavioural Therapy (CBT) | 45.2 ± 9.3 | 23 | 32 | REEDA, VSS |
| Chiu | 2018 | China | Mindfulness and Meditation | 23.8 ± 14.8 | 16 | 24 | REEDA, MSS |
| Kwok | 2023 | Canada | Relaxation Techniques | 29.2 ± 6.1 | 23 | 26 | SWHS, MSS |
| Laskowski | 2021 | Sweden | Counselling and Psychotherapy | 34.2 ± 11.3 | 58 | 62 | REEDA |
| Liu | 2023 | China | Cognitive Behavioural Therapy (CBT) | 27.3 ± 16.5 | 46 | 45 | REEDA, MSS |
| Thorleifsdottir | 2017 | Sweden | Counselling and Psychotherapy | 37.5 ± 15.7 | 7 | 11 | REEDA, MSS |
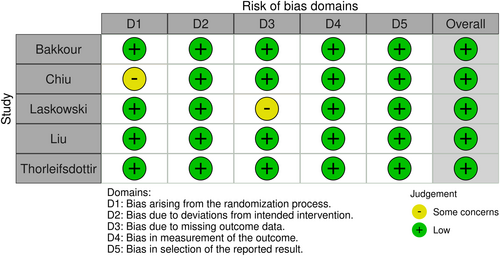
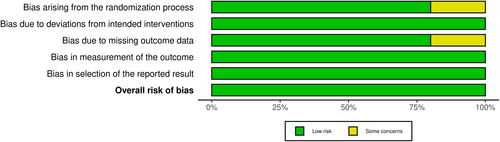
Upon the risk of bias assessment across five different domains (Figure 2), each study was meticulously evaluated. Findings suggested an overall low risk of bias. This was particularly evident in the domains of randomization, protocol adherence, completeness of outcome data, and accuracy of outcome measurement. Notwithstanding this low prevalence of bias, issues of selective reporting were noted in two instances (Figure 3). Despite these concerns, the general bias risk within the included studies was considered to be minimal.
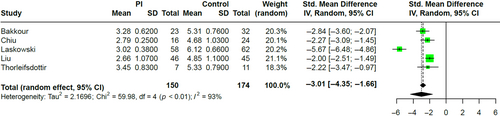
The forest plot analysis provided a graphical representation of the effect of psychological interventions on surgical site healing within 1 week post-operatively, showcasing a significant mean difference in favour of the interventions (SMD = −3.01, 95% CI: [−4.35, −1.66], p < 0.01), as shown in Figure 4. Further analysis at 1 month post-operation using the MSS scale corroborated these findings, indicating a strong positive effect of the psychological interventions on long-term healing outcomes (SMD = 2.31, 95% CI: [1.54, 3.08], p < 0.01), as evidenced in Figure 5.
Investigating potential publication bias, both the funnel plot and Egger's regression test for the 1-week postoperative outcomes on the REEDA scale (Figure 6) indicated no significant bias, affirming the meta-analysis's reliability.
4 DISCUSSION
Our meta-analysis illuminates the significant impact of psychological interventions on surgical site wound healing in psoriasis patients. It is increasingly apparent that the mind–body connection plays a pivotal role in recovery and long-term health outcomes. The positive effects of psychological interventions documented in our study suggest a profound interaction between psychological well-being and physiological healing post-surgery.
The findings within this meta-analysis resonate with the work of Kiecolt-Glaser et al., who demonstrated that stress and depression could alter the immune response and potentially delay wound healing.15, 16 This is particularly relevant for psoriasis patients who are often burdened with emotional stress due to the chronic and visible nature of their condition.4 Our results underscore the significance of addressing psychological health as a component of postoperative care in this patient population.
Moreover, the substantial improvement in wound healing metrics, highlights the tangible benefits of psychological interventions. These findings are in line with the studies conducted by Fatemeh et al., which showed that stress-reduction techniques could lead to better postoperative outcomes.17 Our analysis suggests that interventions such as cognitive-behavioural therapy and mindfulness practices not only alleviate psychological distress but also manifest in improved physical recovery.7
However, it is crucial to note the potential confounders in the relationship between psychological interventions and wound healing. For instance, variables such as the type and severity of psoriasis, the extent of surgical intervention, and individual patient characteristics can all influence recovery. Future research would benefit from stratifying results based on these variables to determine the efficacy of psychological interventions across different patient subgroups.
The therapeutic potential of integrating psychological care into postoperative management is substantial, echoing the sentiments of Gatchel et al., who argued for the incorporation of biopsychosocial models in treatment regimes.18 Psoriasis patients could particularly benefit from such an approach given their unique challenges.19
In the light of our findings, healthcare providers should consider psychological assessments as part of the preoperative process. This could inform postoperative care plans that include psychological support, potentially enhancing recovery outcomes.4 The implications for patient care are profound, advocating for a more holistic approach to surgery recovery, particularly for those with chronic conditions like psoriasis.20
Further studies, particularly randomized controlled trials with larger sample sizes and longer follow-up periods, are warranted to consolidate these findings. These studies should also seek to standardize the psychological interventions used to allow for more direct comparisons and better generalization of the results.21
5 LIMITATIONS
Despite the robust findings, this meta-analysis is subject to certain limitations that must be acknowledged. First, the heterogeneity of the included studies in terms of the types of surgeries performed, psychological interventions applied, and the assessment tools used, may influence the comparability and generalizability of the results. Moreover, the small number of studies that met the inclusion criteria suggests a need for more extensive research in this area. The majority of the included studies also had relatively short follow-up periods, which do not allow for assessment of the long-term efficacy of psychological interventions on wound healing. Additionally, while efforts were made to control for publication bias, it remains a potential limitation as studies with non-significant findings are less likely to be published. Finally, the reliance on self-reported measures in some studies introduces the possibility of subjective bias that may affect the accuracy of reported outcomes. Future research should aim to include a larger number of studies with longer follow-up durations and a standardized approach to psychological intervention and wound assessment to strengthen the evidence base in this field.
6 CONCLUSION
In conclusion, the incorporation of psychological interventions in post-surgical care may represent a paradigm shift in the management of psoriasis patients undergoing surgery. This meta-analysis offers a clarion call for a more integrated approach to healing that transcends the traditional focus on physical recovery alone.
ACKNOWLEDGEMENTS
We express our sincere gratitude for the generous support provided by the following funding sources, which made this research possible: The Government-funded Outstanding Clinical Medical Talent Project (No: ZF2023166), the Hebei Province Key Research and Development Plan Project (No: 223777154D), the Hebei University of Chinese Medicine Graduate Student Innovation Ability Training Support Project (No: XCXZZBS2022015), and the Hebei Province Traditional Chinese Medicine Administration Research Plan Projects (Nos: 2019095 and 2019097). Their contributions have been instrumental in advancing our research endeavours.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are avail-able from the corresponding author upon reasonable request.




