The free chimeric medial sural artery perforator flap for individualised and three-dimensional reconstruction of complex soft-tissue defects in extremities
Xinlei Sui and Umar Zeb Khan contributed equally to this work.
Abstract
Trauma or lesion resection often causes complex wounds with deep soft tissue defects in extremities. Simply covering with a skin flap will leave a deep dead space resulting in infection, non-healing wounds, and poor long-term outcomes. Thus, effectively reconstructing complex wounds with dead space leaves a clinical challenge. This manuscript presents our experience using chimeric medial sural artery perforator (cMSAP) flap, to reconstruct complex soft tissue defects of the extremities, thereby exploring broader analysis and indications for future reference. Between March 2016 and May 11, 2022, patients (8 males and 3 females) with a mean age of 41 years (range from 26 to 55 years) underwent reconstructive surgery with the cMSAP flap. The cMSAP flap consists of an MSAP skin paddle and a medial sural muscle paddle. The size of the MSAP skin paddle ranged between 9 × 5 cm and 20 × 6 cm, and the size of the medial sural muscle paddle ranged between 2 × 2 cm and 14 × 4 cm. Primary closure of the donor site was achieved in all cases. Of the 11 patients, the cMSAP flap survived in 10 cases. The vascular compromise occurred in one special case and was treated with surgical procedures. The mean follow-up duration was 16.5 months (range of 5–25 months). Most patients present satisfactory cosmetic and functional results. The free cMSAP flap is a good option for reconstructing complex soft tissue defects with deep dead space in extremities. The skin flap can cover the skin defect, and the muscle flap can fill the dead space against infection. In addition, three types of cMSAP flaps can be used in a broader range of complex wounds. This procedure can achieve an individualised and three-dimensional reconstruction of the defects and minimise the donor site morbidities.
1 BACKGROUND
Trauma or lesion resection often causes complex wounds with deep soft tissue defects in extremities.1 Simply covering with a skin flap will leave a deep dead space resulting in infection, non-healing wounds, and long-term poor outcomes. Thus, effective reconstruction of complex wounds with dead space leaves a clinical challenge.
The feasible method to repair such defects is using myocutaneous flap transplantation like the vastus lateralis myocutaneous or latissimus dorsi flap, whose advantages are reliable blood supply, constant anatomy, concealed donor site, and large resection area.2, 3 Pedicled myocutaneous flap such as the gastrocnemius myocuteneous flaps are appropriate for repairing large soft tissues defects because of the large dimension, survival reliability, and the easy and quick surgical procedure in the lower leg. These types of flaps involve harvesting part of the skin, subcutaneous fat and muscle of the calf and transplanting to the affected area.4 However, the major problem of the myocutaneous flap is the unseparated skin and muscle flaps with limited mobility between the skin and muscle.5 As a result, the appearance of the recipient site is usually bulky and the donor site is damaged greatly. Another available method is combined free skin flaps and muscle flaps transplantation for repairing wounds with deep dead space.6, 7 The method requires the separate harvest of the skin and muscle flap and anastomose of the two groups of blood vessels, prolonging the operation time and increasing the operation risk.8
In recent years, the chimeric perforator flap has been considered the appropriate option for three-dimensional reconstructive surgeries for wounds with deep dead space.9, 10 For the recipient area, the chimeric perforator flap can realise the relative separation of the skin flap and the muscle flap so that the muscle flap can be accurately embedded in the deep dead space, and the flap can cover the skin defect, achieving precise repair and avoiding a bloated shape. For the donor site, the volume of the skin flap and muscle flap can be precisely designed to reduce damage to the donor site. At the same time, only one group of blood vessels needs to be anastomosed during the operation, which can reduce the operation time and risk.
The medial sural artery perforator (MSAP) flap is known to be a typical flap for repairing soft tissue defects of extremities. By carrying part of the medial gastrocnemius muscle, a chimeric MSAP (cMSAP) flap can be made to three-dimensionally reconstruct complex soft tissue defects of extremities with deep dead space.11, 12 At present, there are few literature reports on cMSAP flap. This article reports our 11 cases of complex extremity wounds with deep dead space repaired by cMSAP flap in our hospital from March 2016 to May 2022 were retrospectively analysed.
2 METHODS
This retrospective study enrolled 11 patients aged between 26 and 55 (8 males and three females) who underwent reconstructive surgery in extremities with the cMSAP flap. There were three wounds on the hand and forearm and eight on the foot and ankle. They were characterised by a moderate-sized skin defect combined with deep dead space. The detailed patient data are listed in Table 1.
| Case | Gender | Age | Site of defects | Cause | Size of skin flap (cm) | Size of muscle flap (cm) | Type of chimeric flap | Recipient vessels | Complications | Donor site | Follow-up months |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 37 | R. Medial malleolus | Traffic injury | 10 × 4 | 5 × 3 | Type III | PTA | None | Primary | 25 |
| 2 | M | 46 | L. Foot dorsum | Traffic injury | 14 × 5.5 | 8 × 4.5 | Type I | DPA | None | Primary | 16 |
| 3 | M | 46 | R. Volar forearm | Machine injury | 15 × 5 | 5 × 4 | Type II | BA | None | Primary | 5 |
| 4 | M | 26 | L. Heel | Chronic osteomyelitis | 11 × 4 | 9 × 3 | Type II | PTA | None | Primary | 13 |
| 5 | M | 32 | L. Medial foot | Machine injury | 20 × 6 | 8 × 3 | Type I | PTA | None | Primary | 6 |
| 6 | F | 55 | R. Foot dorsum | Chronic ulcer | 11 × 5.5 | 5 × 3.5 | Type I | DPA | Venous crisis | Primary | 24 |
| 7 | M | 36 | R. Hand dorsum | Machine injury | 10 × 4.5 | 3.5 × 3 | Type II | UA | None | Primary | 25 |
| 8 | F | 53 | R. Heel | Traffic injury | 13 × 4.5 | 2 × 2 | Type I | PTA | None | Primary | 24 |
| 9 | M | 23 | R. Volar forearm | Crush injury | 20 × 6 | 6 × 5 | Type II | BA | None | Primary | 6 |
| 10 | M | 42 | R. Heel | Chronic osteomyelitis | 9 × 5 | 6 × 2 | Type II | PTA | None | Primary | 23 |
| 11 | F | 54 | L. Pelma | Chronic ulcer | 14 × 4 | 14 × 4 | Type II | PTA | None | Primary | 15 |
- Abbreviations: BA, brachial artery; DPA, dorsalis pedis artery; F, female; L, left; M, male; PTA, posterior tibia artery; R, right; UA, ulnar artery.
The same surgical team performed all operations. Written informed consent was obtained from the patients. Ethical approval was acquired from the local ethical committee.
2.1 Surgical procedures
Preoperatively, a computed tomography angiography (CTA) of the lower extremities was carried out in all patients to map the perforators. A handheld Doppler was applied to locate the perforators. After radical debridement, fracture fixation, or finger replantation, a paper template was tailored according to the shape of the skin defects. Notably, the skin pinch test was performed on the lower leg to ensure the donor site's direct closure. The dimension of the muscle flap was assessed according to the size of the dead space.
A reference line was drawn from the popliteal crease's midpoint to the medial malleolus's midpoint. Outline the flap on the medial lower leg according to the paper template, with the main perforator as the centre and the reference line as the axis. The flap was harvested from the posterior border. The perforator was defined during the dissection in the superficial fascia. Retrace the perforator back to the main trunk of the medial sural artery and dissect it at the proper position according to the required pedicle length. The cMSAP flap consists of an MSAP skin paddle and a medial sural muscle paddle. The diagram illustration of the free chimeric medial sural artery perforator flap for the reconstruction of complex extremities defects is shown in Figure 1.
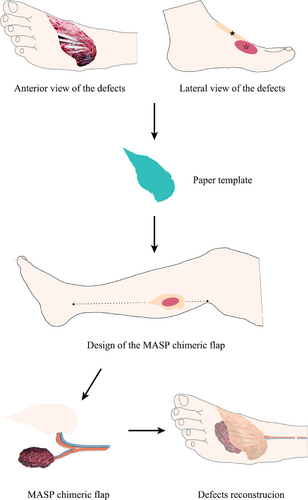
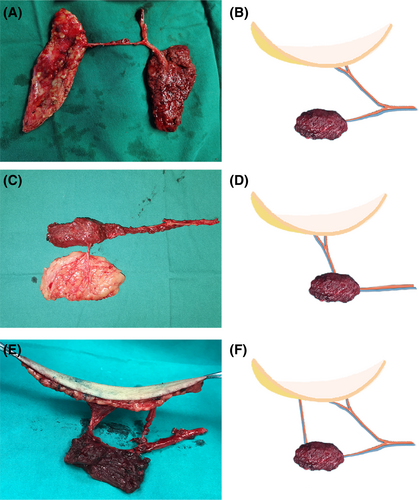
- Type I: The skin and muscle paddles are separated and nourished by the independent branches of the medial sural artery (MSA). The pedicle of each paddle requires intramuscular dissection in this type of design (Figure 2A,B).
- Type II: The skin and muscle paddle have only the direct perforator vessels connected, and the branches of the MSA nourish the muscle paddle. This design reduces intramuscular dissection and, thus, surgical time and minimises the donor site morbidities (Figure 2C,D).
- Type III: The skin and muscle paddle have both direct perforator vessels connected and branches of the MSA connected. Although this design is relatively time-consuming, it increases the reliability of the blood supply in the chimeric flap when the wound is large (Figure 2E,F).
After the harvest of a particular type of cMSAP flap, transfer the flap to the recipient site by inserting the muscle paddle into the dead space and covering the skin defects with the skin paddle. Carefully rationalise and anatomize the medial sural artery and the proper recipient vessels. The wound of the recipient site was interrupted and sutured, and the donor site was closed directly, layer by layer.
3 RESULTS
Of the 11 cases, the cMSAP flaps were successfully harvested for individualised and three-dimensional reconstruction of complex defects in extremities. Among them, Type I chimeric flap was applied in 4 cases, Type II in 6 cases, and Type III in 1 case. The size of the skin flap ranged between 9 × 5 cm and 20 × 6 cm, and the size of the medial sural muscle flap ranged between 2 × 2 cm and 14 × 4 cm. All the donor sites were closed primarily.
Ten out of eleven cMSAP flaps survived uneventfully. The venous crisis occurred in one case 16 h after the surgery (Case 6). Emergency surgery was performed for vascular exploration. Intraoperatively, there was no venous reflux at the anastomosis, and a free anterolateral thigh perforator flap was then harvested to reconstruct the defects.
The mean follow-up duration was 16.5 months (range of 5–25 months). Most patients present satisfactory cosmetic and functional results.
4 CASE REPORT
4.1 Case 4
A 26-year-old male suffered from heel osteomyelitis on his left foot (Figure 3A). After thorough debridement, there was a moderate-sized skin defect and a subcutaneous dead space (Figure 3B). A Type II cMSAP flap was designed and harvested to reconstruct the defects (Figure 3C,D). The size of the skin paddle was 11 × 4 cm. The size of the muscle paddle was 9 × 3 cm. The MSAP skin paddle covered the heel, and the chimeric medial sural muscle paddle filled the dead space (Figure 3E). Vascular anastomosis was performed between the MSA and the posterior tibia artery. The donor site was closed directly. The cMSAP flap survived successfully without any complications (Figure 3F).
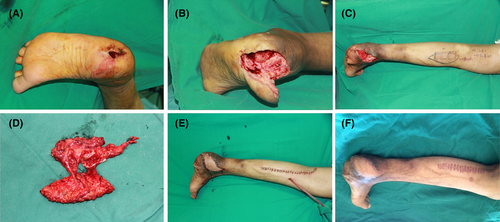
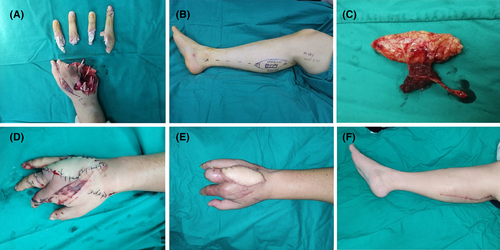
4.2 Case 7
A 36-year-old male suffered a machine injury on his right hand. After radical debridement and fingers replantation, the moderate-sized skin defects and a subcutaneous dead space were left on the hand dorsum (Figure 4A). A Type II cMSAP flap was designed and harvested to reconstruct the defects (Figure 4B,C). The size of the skin paddle was 10 × 4.5 cm. The size of the muscle paddle was 3.5 × 3 cm. The MSAP skin paddle repaired the skin defects of the hand, and the chimeric medial sural muscle paddle eliminated the dead space (Figure 4D). Vascular anastomosis was performed between the MSA and the ulnar artery. The donor site was closed directly. The cMSAP flap survived successfully without any complications (Figure 4E,F).
5 DISCUSSION
There has been rising concern over the problems associated with the reconstruction of complex wounds with deep dead space.13 Because of the presence of deep soft tissue defects, simple flaps can only cover the surface of the skin, but cannot solve the deep tissue defects and the complications of infection.14
These wounds are usually treated by musculocutaneous flap transplantation such as anterolateral thigh musculocutaneous flap and latissimus dorsi flap.15, 16 They have several advantages including constant anatomy, reliable blood supply, large area, and concealed donor site.17, 18 However, the major problem of the musculocutaneous flap is that the muscle part of the flap is not separated from the skin part under the traditional harvesting method.19-21 This results in greater muscle damage at the donor site and a bloated appearance at the recipient site, especially for the small- to medium-sized defects.
Recently, the chimeric perforator flap provides a good solution to reconstruct three-dimensional defects with deep dead space in extremities, such as chimeric anterolateral thigh perforator flaps and chimeric DIEP flaps. Although the application of cMSAP flap in extremities reconstruction has rarely been reported. In this study, we reported a cMSAP flap design in reconstructing small to medium-sized complex defects with deep dead space in extremities. The relatively separated skin paddle and muscle paddle supplied by MSA are harvested through reasonable design.22, 23 The muscle paddle fills the dead space with good blood and oxygen supply and can fight infections,17 while the skin paddle covers the wound. Thus, individualised and three-dimensional reconstruction of the defects was achieved with aesthetic appearance.
Similar to the traditional MSAP flap, the cMSAP flap has the following advantages. The soft and hairless calf flap is suitable for repairing soft tissue defects of the extremities The anatomy of the perforators of the MSV is relatively constant, and a long vascular pedicle can be harvested.24, 25 Furthermore, the medial sural cutaneous nerve can be carried in the flap to restore the sensation in the flap.26 Meanwhile, after selecting the supine or prone position according to the recipient area, the surgery can be performed in one position without change.27
In addition, the three designs of cMSAP flaps have their own characteristics. The choice needs to consider the location of the dead space, the size of the flap, and the donor site injury.28 Type II cMSAP flap was suitable for small to medium-sized defects where the location of the dead space is close or under the wound, and the short vascular pedicle is sufficient. This dissection is time-saving with less donor site morbidity. When a longer pedicle is required, Type I serves the wound with the dead space situated a distance away from the edge of the wound. This dissection is often time-consuming but offers great skin and muscle flap flexibility. Marsh and Chana (2010) recommend that large wounds require Type III flaps, with the two perforator vessels having adequate blood and oxygen supply.29
Venous reflux disorder is a common reason for the failure of MSAP because of the mismatch in the width of the usually smaller receiver and larger donor vein of the medial sural artery. We usually choose large superficial veins or venous bifurcations in the recipient area for anastomosis and two venous drainage pathways will be reconstructed whenever possible.
Preoperatively, the pinch method is often used to estimate the flap width to achieve primary closure of the donor site and avoid undesired scars caused by a skin graft. Besides, we use this cMSAP flap with caution in young women and paediatric patients because linear scars can also destroy the appearance of the lower leg.
This manuscript presents our experience using cMSAP to reconstruct complex soft tissue defects of the extremities, thereby exploring broader analysis and indications for future reference. Much of the attention has been concentrated on the classification and the application of cMSAP for the three-dimensional reconstruction of wounds with deep dead space in a more customised way,30, 31 giving minimal donor morbidity and aesthetic appearance after surgery.
This article has limitations because of the small number of patients although this is the largest case series using cMSAP to reconstruct complex soft tissue defects of the extremities to our knowledge. Another limitation is the absence of a control set of patients. For instance, no instance presented a case where two or more flaps were used to reconstruct a defect with deep dead space. In addition, there is a lack of standardised postoperative assessment of extremity function.
6 CONCLUSION
The free cMSAP flap is a good option for reconstructing complex soft tissue defects with deep dead space in extremities. The skin paddle can cover the surface skin defects, and the muscle paddle can fill the dead space against infection. In addition, three types of cMSAP flaps can be used in a broader range of complex wounds. This procedure can achieve an individualised and three-dimensional reconstruction of the defects and minimise the donor site morbidities.
AUTHOR CONTRIBUTIONS
Xinlei Sui and Umar Zeb Khan wrote the manuscript, Juyu Tang supervised the study, and Liming Qing, Fang Yu, Panfeng Wu revised the manuscript. All authors contributed to the article and approved the submitted version.
ACKNOWLEDGEMENTS
During the study the contribution of following doctors are very appreciated. We would like to thank Dr. Nianzhe Sun and Hafsa Iqbal, Department of Hand & Microsurgery, The Xiangya Hospital, Central South University, for his help in clinical work.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICAL APPROVAL
Ethical approval was obtained from the Institutional Review Board of the Xiangya Hospital of Central South University.
Open Research
DATA AVAILABILITY STATEMENT
The raw data supporting the preparation and conclusion of this article will be available by the authors without undue reservation.