Post-burn scar malignancy: 5-year management review and experience
Abstract
The study spotlights a severe uncommon post-burn complication, Marjolin's ulcer, in upper Egypt plastic and wound care centres. This problem is mainly related to inadequate medical care and awareness. No community or race is immune. The underlying malignant transformation mechanism remains unclear. The study aims, according to our experience, to review the prognostic factors through the management protocol of Marjolin's ulcers. This prospective study was conducted in the Aswan University Plastic & Burn surgery department in South Egypt between 2013 and 2020 and investigated 226 patients with chronic post-burn ulceration. Nineteen cases were proved to have Marjolin's ulcer, and the other cases that had been excluded from being malignant went for reconstruction with split-thickness skin graft with/without flap after adequate ulcer debridement. The surgical, oncologic, radiologic indications, and prognostic factors were reviewed according to our management outcome—the assessment with follow-up period extended over 5 years. Histopathology of ulcers ranged among mild, moderate, and poorly differentiated squamous cell carcinoma. One scalp ulcer case showed basosquamous pathology. Most cases presented at age above 50, but no age was immune. The mean latent period was 29 years on average. The lesions' sites varied in their anatomic location where they involved the upper extremity, the scalp, and the lower extremity that had a predilection. Although surgical excision is the primary management line for tumour ablation, other factors may change the management course. During the follow-up period, neoplasm recurrence in the form of lymph node enlargement and/or locoregional metastasis was detected in eight cases. Within 1 year after the intervention, six recurrent cases died, and two were saved. In addition to the case study, this paper reviewed the literature and provided our team a good experience in light of the NCCN protocol for non-melanotic cutaneous carcinoma, although we suffered limited medical resources. It is concluded that early accurate diagnosis, low-grade malignancy, and well-planned individualised surgery with adjuvant radiotherapy were the best prognostic factors. The close follow-up for an early sign of disease recurrence is paramount.
1 INTRODUCTION
The term Marjolin's ulcer refers to any aggressive malignant ulcer presenting in an area of previously burned, traumatised, chronically inflamed, scarred skin, or post-radiotherapy scars. The incidence of chronic ulcers to be transformed into malignancy is 2% to 6% after a long-term inflammatory or traumatic insult to the skin.1-3 Incidence of occurrence was higher in Asians and Africans than other races where skin complexion and genetic factors may play a role, with low socio-economic status.4, 5 Various skin cancer histopathologic findings may arise in scar tissue, most commonly squamous cell carcinoma. Other less frequent types of wound cancers are basal cell carcinomas, sarcomas, or melanomas. The risk of metastasis is highly correlated with the degree of differentiation of the tumour.6-8
Prevention of aetiologic factors and prophylaxis was known to be the best management. When a burn or a skin trauma has occurred, medical care must ensure appropriate and stable healing by various reconstructive modalities, for example, skin graft or flap. Once the diagnosis of malignant ulcer is established, surgical excision with a safety margin not less than 2 cm is considered the primary management plane.6, 9-11 There is a considerable debate on the efficacy of only chemotherapy or radiotherapy in Marjolin's ulcer. Radiotherapy can only be used as a primary treatment in inoperable cases and as a palliative choice if the patient refuses limb amputation.6, 11-14 The controversy extends in the literature to the indications of lymph node dissection. Some authors recommended prophylactic regional lymph node dissection because of a high incidence of metastasis after Marjolin's ulcer excision, especially in the lower extremity.15-18
On the other hand, many other authors recommended dissection only in clinical positive enlarged nodes. Here, the lymphadenectomy should be followed by radiotherapy at the nodal basin.19-21 The sentinel lymph node assessment role in Marjolin's ulcer management is still not established.22-24
The study aimed at reviewing and evaluating post-burn Marjolin's ulcer through the management process and outcome results. We discussed prognostic factors, management indications, and contraindications.
2 PATIENT AND METHODS
This prospective study was conducted in Aswan University Plastic & Burn surgery department in South Egypt between 2013 and 2020. Two hundred twenty-six patients with suspicious chronic ulcers on top of an old burn at any part of the body were assessed. Inclusion criteria involved medically stable adult patients who had malignant post-burn scar lesions. We excluded patients with the non-burn scar, benign lesions, or debilitating medical conditions.
The ‘interdisciplinary tumor board’ comprised reconstructive burn surgeons, oncosurgeons, clinical pathologists, radiotherapists, and social workers. During investigations and intervention, we considered the Ethics of Declaration of Helsinki and the approval of the Aswan University medical school ethical committee with obtained informed written consent.
Clinical examination of suspicious ulcer included documenting its size, dimension, size, shape, margin, edge, discharge, tenderness, ulcer base, and draining lymph nodes. We correlated previous burn surgery(s) at the ulcer region with the incidence of malignant transformation in the same scar area.
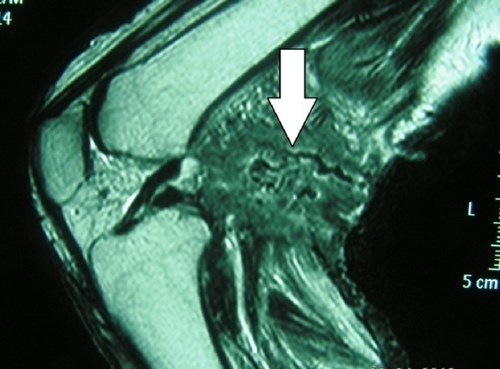
The radiodiagnostic assessment for malignant ulcer patients included magnetic resonance imaging (MRI) and ultrasonography. Ultrasonography (U/S) was used as a primary assessment for ulcer base and catchment area's draining lymph nodes. Furthermore, MRI using axial T1 and T2 weighted images with administered gadopentate dimeglumine was used to delineate soft tissue details of the locoregional area and draining lymph nodes.
Histopathologist assessed tumour character and grade after taking out four-quadrant incisional biopsies or the whole ulcer as a specimen. The malignancy grade was categorised according to the percent of tumour cells differentiation into three grades: grade I (well-differentiated) with more than 75% of the cells differentiated, grade II (moderately differentiated) with 25% to 75% of the cells differentiated, and grade III (poorly differentiated) with less than 25% of cells differentiated. The malignancy extension was categorised as either lymphatic or venous invasion.25, 26 We used the tumour staging protocol of the American Joint Committee on Cancer (AJCC) TNM staging system 7th edition for nonmelanoma skin cancer (NMSC). The staging is based on tumour diameter, lymph node metastatic invasion, and distant metastasis grading.25-28
The surgical intervention was decided according to tumour characters, staging, and ulcer depth. The ulcer was excised with a safety margin not less than 3 cm. The superficial ulcer not exceeding the subcutaneous layer was excised down to the fascia, and a deep ulcer invading down to the fascia was excised with underlying fascia and muscle. The amputation was indicated for a deep ulcer that breached the periosteum or invaded the underlying bone. The enlarged lymph node(s) were excised in the same session. After tumour ablation or amputation, the reconstructive modalities were as follows: skin grafting, local flap, or free flap according to the defect site, size, and depth.
The regional adjuvant radiotherapy was indicated in the following conditions: after regional lymphadenectomy, tumour recurrence and/or lymphatic metastasis, or low-grade differentiation type. Management protocol followed the National Comprehensive Cancer Network (NCCN) recommendation, 2008, modified in 2016. Total radiation dose ranged between 5000 and 6000 cGy in 250 cGy fractions in ulcers more than 20 mm in size.28
The patients were followed up in the out-patient clinic after stabilised intervention every 2 weeks for 2 months, every 2 months for 6 months, and then every 6 months for 5 years. In case of locoregional or lymphatic recurrence suspicion, we did a complete body survey that included pelviabdominal ultrasound, chest X-ray, MRI, and lab investigation.
2.1 Statistical analysis of the data
Data were subjected to analysis using IBM SPSS software package version 20.0. Comparisons between groups for variables were assessed using the Chi-square test (Fisher or Monte Carlo). Wilcoxon signed ranks test was used for abnormally distributed quantitative variables in different periods. The significance of the results was assessed at the 5% level.
3 RESULTS
A cohort group of 226 patients in series with chronic post-burn ulceration without previous history of cancer had been assessed. This study extended for 5 years for each patient through conduction in Aswan University hospital at South Egypt, Plastic & Burn reconstructive department between 2013 and 2020.
In this study, the incidence of proved transformed malignancy on top of post-burn chronic ulcer scar, that is, more than 1 month, was 8.4%, i.e., 19 patients. There were 15 males (79%) and four females (21%). Twelve of them (63%) were above 55 years old. The predilection of ulcer site was in the lower extremity in 13 patients (68.4%), 3 cases at upper limb (15.8%), 2 cases (10.6%) at the trunk (pectoral and lateral chest wall), and 1 case in the scalp (5.2%). The average ulcer size at the time of examination was 86.8 cm2 (±29). The latency period between burn insult and malignant transformation was 29.68 years (±5.4), as summarised in Tables 1 and 2. All cases were diagnosed with squamous cell carcinoma except one with basosquamous cancer in the scalp. The remaining 207 cases had been excluded from being malignant ulcers were managed with ulcer debridement and reconstructed with either split-thickness skin graft or proper flap coverage over a period of the study without recorded tumour appearance nor mortality.
| Case No./age | Sex | Previous surgery and number | Ulcer site/Periosteal invasion | Ulcer size (cm2) | Latency (years) | Tumour/grade | Preo-p. lymph node | staging | Operative surgery | Post-op. lymph node (6 months) | Locoregional recurrence | RTX | Follow-up (years)/mortality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1-65 | M | — | Lower limb, (+) | 35 | 20 | SCC/well | — | Stage II | BKA | — | — | No | 7/(tumour free) |
| 2-68 | F | — | Lower limb | 42 | 65 | SCC/moderate | — | Stage II | Excision -flap/skin graft | Inguinal | — | Yes | 5/(tumour free) |
| 3-53 | M | — | Lower limb (+) | 50 | 35 | SCC/well | — | Stage II | BKA | Inguinal | — | Yes | 4.5/(tumour free) |
| 4-65 | F | — | Upper limb (+) | 150 | 45 | SCC/poor | Axillary | Stage III | BEA | Axillary | + | Yes | 0.5/(died) |
| 5-42 | M | Skin graft (2) | Lower limb | 162 | 30 | SCC/well | — | Stage II | Excision -flap/skin graft | — | — | No | 5/(tumour free) |
| 6-52 | M | — | Trunk | 255 | 15 | SCC/poor | — | Stage II | Excision, skin graft | Inguinal and paraaortic | + | Yes | 1/(died) |
| 7-32 | M | Skin graft – flap (1) | Upper limb | 35 | 20 | SCC/well | — | Stage II | Excision, Skin graft | — | — | No | 5.5/(tumour free) |
| 8-55 | M | — | Lower limb, (+) | 156 | 34 | SCC/poor | Stage II | AKA | Inguinal | — | Yes | 0.75/(died) | |
| 9-44 | M | — | Lower limb | 180 | 35 | SCC/poor | Stage II | Excision Skin graft | Inguinal | — | Yes | 1.16/(died) | |
| 10-82 | M | — | Lower limb, (+) | 80 | 25 | SCC/moderate | Inguinal | Stage III | BKA | — | — | No | 5/(tumour free) |
| 11-75 | M | — | Scalp, (+) | 84 | 31 | Basosquam. | Cervical | Stage III | Excision -flap/skin graft | cervical | + | Yes | 1/(died) |
| 12-50 | M | Skin graft (2) | Lower limb | 24 | 35 | SCC/well | — | Stage II | Excision -flap/skin graft | — | — | No | 4/(tumour free) |
| 13-52 | M | — | Lower limb | 25 | 30 | SCC/well | — | Stage II | Excision, skin graft | — | — | No | 5/(tumour free) |
| 14-39 | M | Lower limb | 24 | 22 | SCC/well | — | Stage II | Excision -flap/skin graft | — | — | No | 4.5/(tumour free) | |
| 15-45 | F | — | Upper limb | 168 | 30 | SCC/poor | — | Stage II | Excision -flap/skin graft | axillary | — | Yes | 1.2/(died) |
| 16-44 | M | — | Lower limb | 40 | 28 | SCC/well | — | Stage II | Excision, free flap | — | — | No | 5/(tumour free) |
| 17-48 | M | — | Trunk | 54 | 10 | SCC/moderate | — | Stage II | Excision, skin graft | — | — | No | 5/(tumour free) |
| 18-55 | F | Skin graft (1) | Upper limb | 63 | 30 | SCC/well | — | Stage II | Excision, free flap | — | — | No | 4.5/(tumour free) |
| 19-58 | M | — | Lower limb | 120 | 24 | SCC/moderate | — | Stage II | Excision -flap/skin graft | — | — | No | 5/(tumour free) |
- Abbreviations: AKA, above-knee amputation; BEA, below elbow amputation; BKA, below-knee amputation; L.L., lower limb; RXT, radiotherapy; SCC, squamous cell carcinoma; UL, upper limb.
| No. (%) | |
|---|---|
| Sex | |
| Male | 15 (79%) |
| Female | 4 (21%) |
| Age (years) | 55.4 ± 15 |
| <55 | 12 (63%) |
| ≥55 | 7 (37%) |
| Ulcer site | |
| Lower limb | 13 (68.4%) |
| Upper limb | 3 (15.8%) |
| Forehead | 1 (5.2%) |
| Trunk | 2 (10.6%) |
| Ulcer size | 86.8 ± 29 (cm2) |
| Latency (years) | 29.68 ± 5.4 |
| Follow-upa (years) | 5 ± 0.31 |
| Mortality | 6 cases (31.6%) |
- Note: Qualitative data were described using numbers and percent, while typically quantitative data were expressed in mean ± SD, abnormally distributed data were expressed in median (Min.–Max.).
- a Average follow-up period for survivals.
The follow-up protocol guide was applied in regular intervals by the interdisciplinary tumour board for 5 ± 0.31 years.
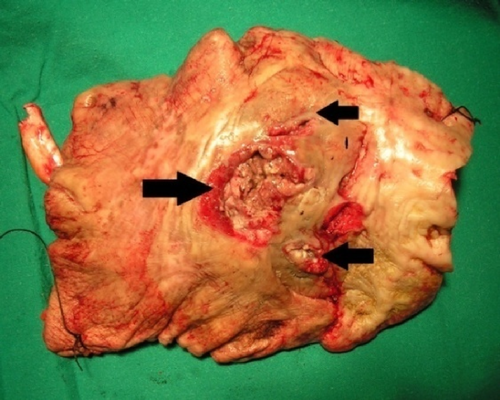
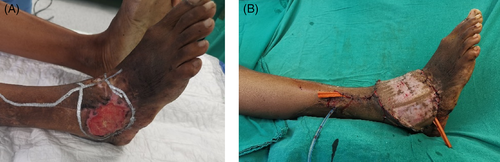
Although most ulcers were painless, two patients complained of severe, intractable pain at lower limb lesions. Macroscopic pictures of the malignant squamous cell ulcers appeared in many forms as a shallow indurated lesion with a raised active edge, unhealthy necrotic granulation at ulcer flour, or deep destructive crater with foul smelly discharge and multiple sinus openings (Figures 1-5).



Regarding the correlation of Marjolin's ulcer incidence with the previous reconstructive procedure at the ulcer region, it showed that the incidence of malignancy of the non-reconstructed cases (80% of cases) was 4-fold more than those who were previously reconstructed—4 (20% of cases). The average number of previous reconstructive procedures was 1.2.
Surgical excision ensured no less than a 3 cm safety margin width and down to the deep fascia. The reconstruction of a defect after a non-invading malignant ulcer was performed for 13 cases (68.4%). The reconstructive options included five patients with a skin graft, six local flap and skin grafts (Figure 6A-D), and two cases with free anterolateral thigh (ALT) flaps (Figure 7A,B). The invading malignancy underneath bone was operated by limb amputation in five patients (31.6% of cases); three below the knee, one above the knee, and one below elbow amputation. The invading scalp ulcer was excised with the outer skull cortex then covered with local scalp flaps.

No significant difference had been seen between various reconstructive procedures as regard tumour recurrence or survival rates. Also, no significant difference between excision procedure and limb amputation. Here, the depth of tumour invasion was a cut point indication for choosing the type of intervention (Tables 3 and 4):
| Periosteal tumour invasion | Surgery | Postoperative recurrence | Mortality |
|---|---|---|---|
| Negative | Excision 13 cases (68.4%) |
5 (38.5%) | 4 (30.7% of excision surgery patients) |
| Positive | Amputation 6 cases (31.6%) |
3 (50%) | 2 (33.3% of the amputated patient) |
| Surgery excision (n = 14) | χ2 | P | ||
|---|---|---|---|---|
| Postoperative finding | Amputation (n = 5) | |||
| lymph node metastasis | ||||
| Negative | 9 (64.2%) | 3 (60%) | 0.029 | 1.000 |
| Positive | 5 (35.7%) | 2 (40%) | ||
| Ulcer recurrence | ||||
| Negative | 10 (71.4%) | 3(60%) | 0.223 | 1.000 |
| Positive | 4 (28.6%) | 2(40%) | ||
| Mortality | ||||
| Survived | 10 (71.4%) | 3 (60%) | 0.223 | 1.000 |
| Died | 4 (28.6%) | 2 (40%) |
- Note: Qualitative data were described using number and percent and were compared using the Chi-square test or Fisher's exact test.
No significant statistical correlation between malignancy staging and prognosis. No case was diagnosed as stage I. Sixteen patients were diagnosed with stage II and three patients with stage III. The recurrence rates of stage II and III cases were 37.5% and 66.6%, respectively (P = 0.278). The mortality rate for patients with stage II was 31.25% and 66.6% for cases with stage III (P = 0.046).
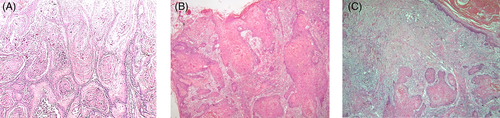
It was shown that histopathologic tumour grade is the most significant prognostic factor correlated with the incidence of lymphatic metastasis ulcer recurrence and mortality rate (Figure 8A-C) and Table 5. Tumour recurrence occurred in eight cases (42%) after the surgical intervention—three of them were associated with locoregional recurrence.
| Tumour grade | χ2 | P | ||||
|---|---|---|---|---|---|---|
| Grade I (well) (n = 9) | Grade II (moderate) (n = 5)** | Grade III (poor) (n = 5) | Total 19 | |||
| Lymph node postoperative | ||||||
| Negative | 8 (88.8%) | 3 (60%) | 0 (0%) | 11 cases | 10.142* | 0.007* |
| Positive*** | 1 (11.2%) | 2 (40%) | 5 (100%) | 8 cases | ||
| Ulcer recurrence | ||||||
| Negative | 9 (100%) | 4 (80%) | 2 (40%) | 15 cases | 6.143* | 0.026* |
| Positive*** | 0 (0%) | 1 (20%) | 3 (60%) | 4 cases | ||
| Mortality | ||||||
| Survived | 9 (100%) | 4 (80%) | 0 (0%) | 13 cases | 14.115* | <0.001* |
| Died | 0 (0%) | 1 (20%) | 5 (100%) | 6 cases | ||
- Note: Qualitative data were described using number and percent and were compared using the Chi-square test or Fisher's exact test.
- * Statistically significant at P ≤ 0.05.
- ** Basosquamous lesion was graded with moderate SCC differentiation.
- *** Patient received radiotherapy according to protocol.
The incidence of tumour recurrence in grade I (well-differentiated) was as follows: 11.2% lymphatic metastasis with no ulcer recurrence or mortality. Grade II (moderate differentiation) incidence was 40% lymphatic metastasis, with 20% incidence of locoregional ulcer recurrence, and 20% mortality rate. The incidence in grade III (poor differentiation) was 100% lymphatic metastasis, and 60% incidence of ulcer recurrence, followed by 100% mortality rate.
The 5-year mortality rate for all cases was 31.6% (six cases). It should be noted that those poor patients had an aggressive postoperative lymphatic invasion with rapid deterioration of their general condition as early as 2 months after surgical intervention. All mortalities occurred within 12 to 18 months after intervention, although they received palliative and adjuvant radiotherapy treatment.
4 DISCUSSION
4.1 Demography
The cutaneous squamous cell carcinoma is the second most common cutaneous malignancy with increasing incidence every year. The burn scar is one of the risk factors that may transform into an aggressive type of cutaneous malignancy called Marjolin's ulcer. It accounts for 0.05% of all squamous cell carcinomas of the lower limb and about 2% of burn scars undergoing malignant transformation.2, 3, 10, 29
Treves and Pack evaluated 2000 patients with skin cancer and reported 2.5% of squamous cell carcinomas and 0.3% of basal cell carcinomas resulted from burn scar conversion.1 This study showed that the incidence of malignancy was 8.4% of 226 cases. This relatively higher incidence than other reports may be explained by the detailed specification of a cohort group of patients with old burn scars who had suspicious lesions rather than including any old scar lesions. Also, medical awareness with early reconstructive procedures lacked in upper Egypt that increased their numbers and complications.
The male-to-female ratio was 4:1; the male gender was 15 cases; 79%. Approximately 63% of patients were above 55 years. The latency period, which is the time from burn incidence to malignant changes, was about 29 years on average. Esther et al,6 Gul and Kilic reported a male-to-female ratio of 3:1 with an average age of patients above 50 years.7 In the literature, the latency period ranged between 30 and 35 years.30, 31 Here, the patient's age at the time of injury influenced this latency time, which is inversely proportional to the patient's age at the burn time. Lawrence reported that the period could widely range from 32 up to 85 years (average of 55.4 years). This long period could be divided into pre- and post-ulceration periods that vary from one case to another. Even though Sharma and co-workers reported that there is a possibility of acute evolution, with a maximal time of 1 year, especially in cases with burn scars.8, 32
The predilection site of Marjolin's ulcer was found to be at lower extremities at 68.4% of our cases, although it can be anywhere. Copcu reported incidence in lower extremity as 58% in 31 studied patients. They explained this most probably because of the high vulnerability of the lower extremity to trauma and burn.20, 34
4.2 Etiologic features
The delayed wound healing, scar instability because of repetitive irritation, especially at joint flexion, and bony prominences with chronic inflammation played critical factors in the development of scar cancer, although still, no area of the burn is immune.35 During the pre-ulceration period, the post-burn scar surface remained intact with a silent course. Later, symptoms and signs like itching, burning pain, and blistering started to pronounce. This should draw the attention of the primary health care providers for the early manifestation of malignant transformation. The duration of this pre-ulceration period is vital for the prognosis. The longer the period, the higher the incidence of malignant change, mainly if scar occurred at a young age with cycles of breakdown and healing.36
4.3 Pathogenesis
The pathogenesis of malignant transformation of chronic wounds remains controversial and poorly understood. This was noticed as some suspicious lesions showed malignancy and others were not, although they had almost the same histories. Nevertheless, Virchow proposed it to be because of chronic irritation. This was explained by continuous mitotic activity as the epidermal cells attempt to resurface the open defect. Cellular mutations by burn exudates, which contain endogenous growth-promoting factors, may act as a co-carcinogen. Infection might serve as a co-carcinogen, especially in inherent local wound immune deficiency patients.3, 31 Hereditary may play a role, as evidenced by recent findings that HLA-DR4 could be associated with the development of cancer.37 Harland et al37 and Hayashi et al38 independently reported abnormalities in the p53 gene in patients with scar cancer. Recent work by Tavares et al,15 Hill et al,39 and Lee et al40 showed that the breakdown of ‘Fas’ ligand, a protein induced by ultraviolet light damage, which regulates skin homeostasis, might play a role in cellular mutation and nuclear changes. A ‘double insult’ concept had been explained by Hahn et al42 that cancer is not triggered by burn or injury alone but also develop by increased susceptibility to other carcinogens such as ultraviolet light or radiation.
4.4 Pathology
It is agreed that the most significant predicting factor for the outcome is the grade of the tumour. Because multiple four-quadrant biopsies remain the gold standard for diagnosing Marjolin's ulcer, it should be performed for all suspicious lesions and shared with an expert histopathologist.26-28, 43 The picture of pseudo-epitheliomatous hyperplasia pathology most resembled well and moderately differentiated squamous cell carcinoma. It is considered in most literature as the benign type that is characterised by an increase in epidermal thickness, with proliferation of irregular strings of squamous cells, minimal or absent cytological atypia, associated with mononuclear inflammatory infiltrate. Other pathologists considered pseudo-epitheliomatous hyperplasia an early stage of squamous cell carcinoma.12, 13, 44 Here, in this study, this picture added misleading delay of early accurate Marjolin's ulcer diagnosis in few cases, which necessitated repeated biopsy examination before confirming the pathology. The basosquamous carcinoma is a rare malignancy with specific histopathological features of the basal cell (BCC) and squamous cell carcinoma (SCC). It has a high risk of metastasis with a close behaviour to SCC. That is why its management protocol followed the same as in the squamous cell.
4.5 Prognostic factors
The lymphatic invasion was predominantly the way of tumour spread rather than venous metastasis (Figure 9). The regional disease sometimes preceded distant metastasis.6, 10, 11, 45 Most ulcers were surrounded by dense reactive fibrovascular tissue that can form a mechanical or immunological barrier preventing early tumour spread. This may explain the rapid, aggressive lymphatic spread after surgical excision in six cases. Theoretically, this may guide the researchers for better ablation techniques that secure afferent lymphatics at wound edges from the systemic micro malignant spread. Bostwick et al46 suggested that cancers that develop within chronic scars may do so within the immunologically privileged site. Harland et al37 and Chalya et al41 discussed the importance of such dense surrounding scars that may play a role in preventing the antigen-specific tumour from being recognised by usual immune surveillance mechanisms.

The TNM grading by AJCC cancer staging manual 7th edition as a single parameter showed no significant correlation with prognosis. On the other hand, the disease prognosis significantly correlated with tumour cell degree of differentiation (ie, grade). The higher the grade, the worst the prognosis.28
4.6 Surgical treatment of Marjolin's ulcer
Prevention of Marjolin's ulcer is the best management. This is mainly achieved by proper wound care with early stable reconstruction at the acute stage, especially over joints and bony prominences.47 This study showed a significant difference between cases primarily reconstructed at an early burn stage and those cases that were not. The malignant transformation incidence was 4-fold more in non-reconstructed cases, which healed by secondary intention. This highlights the importance of early wound care and proper coverage in deep burns lesions.
Proper eradication of the malignancy is the priority as locoregional recurrence carried a poor prognosis. The oncoplastic team should consider clinical evaluation that impacts prognosis as the type of pathology, ulcer location, size, nodal depth assessment, and whether primary or recurrent. Here, surgical excision is the leading choice of treatment that should be individualised carefully with no less than a 3 cm safety margin. It has a significantly favourable outcome regarding tumour ablation with less incidence of tumour recurrence. Many literature reviews agreed with this approach.4, 10, 17, 24, 35, 44
Frozen section by an expert pathologist was a valuable tool to exclude tumour-free margins.5, 48
However, different reconstructive procedures reflected on patient safety, limb functions, and aesthetics outcomes. It is recommended to go for amputation above the first nodal basin for an ulcer that invades deep, important structures as neurovascular bundles, bone, or joint. This is also indicated when extensive local wound infection, chronic osteomyelitis, or severe limb functional impairment. No significant statistical difference in management prognosis or mortality between surgical excision with reconstruction and amputation. Indications for each surgical procedure were different. Ogawa et al49 recommend amputation of the periphery in grade II or III lesions and wide local excision for very small or grade I lesions.
Other surgical modalities like Moh's surgery, curettage, or cryosurgery are not recommended for Marjolin's ulcer by many reports because of the high incidence of deep tumour invasion.15, 50, 51 On the other hand, Copcu's study for small lesions, less than 2 cm, presented 31 cases managed by Moh's micrographic surgery that showed a 92% cure rate.20, 34 However, Moh's surgery has drawbacks of relatively prolonged surgical time, and unfeasibility of its facilities or experts in every centre.
4.7 Lymph nodes management
Marjolin's ulcer draining lymph node management is still debatable. Many authors advised a separate nodal staging system for cutaneous SCC, including Marjolin's ulcer.26, 27 The authors recommended lymphadenectomy either as prophylaxis, selective lymphadenectomy, sentinel lymph node examination, or total lymphadenectomy. The reviews could not weigh one approach as there was no significant difference between prophylactic lymph node dissection types. Some authors go for irradiation and/or selective dissection of enlarged cancerous nodes, especially when the node shows core biopsy poor cellular differentiation.4, 11, 13 Others suggested routine lymph node core biopsy with adjuvant irradiation in all cases of Marjolin's ulceration based on aggressive metastatic behaviour of such cancer.10, 35, 44
This study recommends selective lymphadenectomy and postoperative radiotherapy for enlarged lymph nodes. Many reports agreed that negative node biopsy examination should be closely followed up, otherwise to proceed for prophylactic radiation therapy.44, 50, 52-54
4.8 Adjuvant radiotherapy
The efficacy of radiotherapy, its proper doses, and timing on Marjolin's ulcer is still unclear. Most literature supported the use of adjuvant radiation when resection is precluded in poor surgical candidates, wide metastatic spread, or when a patient refuses the surgery.17, 21 Ozek et al52 stated that ‘radiation is indicated in inoperable lymph node metastasis, grade III lesions with positive lymph nodes after node dissection, greater than 10 cm tumour diameter with positive node involvement following dissection, or lesions of the head and neck with positive nodes after dissection’. Others reported that radiation as a treatment alone is ineffective.16, 18 Radiotherapy in this study was used as an adjuvant therapy with surgical excision when detected enlarged lymph nodes clinically or by MRI findings. The adjuvant radiotherapy courses had a role in two of the cases to keep 5 years tumour-free after ulcer excision and lymphadenectomy. Six cases failed to be controlled with the same management after an aggressive metastatic spread.
4.9 Chemotherapy in Marjolin's ulcer
No role of chemotherapy as adjuvant therapy could be confirmed in the literature for Marjolin's ulcer. Intra-arterial infusions of methotrexate for SCC and topical 5-fluorouracil in small in situ lesions need to be further assessed with variable outcome role.28, 53, 55
4.10 Recurrence and mortality rate
The literature reported that recurrence incidence of SCC on top of burn is higher than de novo SCC, which may reach 11 up to 37%.35 Novick et al4 correlated 46 cases from M.D. Anderson Hospital's location of the malignant ulcer with the incidence of metastasis was twice a higher rate in lower extremities than other sites.
In this study, the recurrence rate overall was 42%. All of those patients showed lymphatic invasion type. Only three cases (15.7%) had locoregional recurrence associated with lymph node enlargement. Here, we can confirm that the higher the grade, that is, poor differentiation with more ulcer depth, the higher the incidence of recurrence and poor prognosis. Well-differentiated pathology cases had the best prognosis. Distant metastasis was mainly to central lymph nodes as paraaortic and spinal and femoral bones. The mortality rate reached 31% of all cases within a 5-year follow-up; two-thirds of them within the first postoperative year and one-third within the 6 months after. This alarms for meticulous close follow-up during this critical period.
In literature, the 5-year survival rate of Marjolin's ulcer was reported to be between 40% and 69%. Exactly 60% for those who underwent a wide excision, and 69% for the amputation group. After excision, the overall recurrence rate was 20% to 50%, with 98% of the ulcers recurring within 3 years.11, 54 Following amputation, the rate of metastasis was 20% up to 35%. As long as the wound margins are clean following a wide excision, there is no significant difference in recurrence between wide local excision and amputation. The overall 3-year survival rate was 65% to 75%, and 10-year survival was 34%.6, 26 However, the 3-year survival rate significantly drops to 35% to 50% for those with metastasis to the lymph nodes. If a patient survives the past 3 years, there is a good prognosis because 95% of patients with metastases present in the first 12 months.13, 35
5 CONCLUSION
- Early reconstruction of burn injuries at the acute stage shall participate as effective prophylactic management to avoid malignant transformation, especially over joint or bony prominences.
- Any changes in an old post-burn scar should draw the attention of primary medical care providers, especially when it stands for more than 10 years.
- The interdisciplinary oncoplastic team highly recommends early diagnosis and individualised management.
- Surgical excision remains the primary treatment line and should not be less than a 3 cm safety margin. After excision or amputation, the defect should be reconstructed with well-padded, stable coverage. Although proximal amputation of the affected limb may be a hard decision for the patient and her/his family, it provided a safe surgical eradication choice.
- Innovative management approach for Marjolin's ulcer is still needed for better functional and survival outcomes. Further histological and immunologic studies are needed for ulcer base surroundings that may act as a barrier that prevent aggressive lymphatic and distant spread that was breached by iatrogenic intervention. Some patients survived with their ulcers for a relatively long period without manifestation of metastasis.
- Controversy on radiotherapy effectiveness on Marjolin's ulcer does not roll out its adjuvant role to decrease possible micrometastases.
- This study confirms reliable prognostic factors of the tumour grade and wide tumour resection, which—both—were the only two independent factors that significantly dictated patients' survival.
- Close follow-up after surgery in the first year is paramount. After that, quarter-year visits are recommended regularly for 5 years.
6 LIMITATIONS
This study was limited to a specific patient subgroup at a tertiary care centre, needs to be based on consensus expert opinion, and requires validation in extensive cohort studies and specific patient sub-populations.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.