Comparative evaluation of the clinical success of 3D-printed space maintainers and band–loop space maintainers
Abstract
Background
Exploring the integration of 3D-printing technology in space maintainer (SM) manufacturing could offer innovative solutions and insights for enhancing SMs.
Aim
To compare the clinical success, retention, and periodontal effect of traditional band–loop (TBL) SMs with 3D-printed SMs.
Design
Seventy children (mean age: 6.99 ± 1.18) were divided into two groups. Laser sintering (LS) group (n = 34): Patients were scanned with an intraoral scanner. SMs were produced with LS 3D-printing method from a titanium-based metal powder. T group (n = 36): Impressions were taken with alginate. SMs were produced by adjusting the bands and soldering the wires on the model. The retention and effects on oral hygiene of the SMs were evaluated at the sixth month. Preference for impression technique was assessed by a five-question survey.
Results
Thirty-eight percent of T SMs and 66% of LS SMs failed (p = .007). The mean survival time was significantly higher in the T group (p = .035). No difference was found between the initial and control full-mouth Gingival Index (GI) and Plaque Index (PI) values of the two groups. Both groups had increased GI/PI values in abutment teeth. Patients in the LS group interpreted their impression experience more positively.
Conclusion
It is important to provide oral hygiene education before applying fixed SMs and utilize more digital workflow in paediatric dentistry.
Why this paper is important to paediatric dentists
- This paper demonstrates that children prefer digital impression techniques, highlighting the benefits of digital dentistry in paediatric dentistry, particularly in improving the comfort of young patients.
- Paediatric dentists aim to provide the best possible care for their young patients. This paper helps understanding the comparative effectiveness, advantages, and potential drawbacks of 3D space maintainers versus traditional space maintainers and can guide practitioners in selecting the most appropriate treatment option for their young patients.
- This paper draws attention to the importance of comprehensive oral hygiene education before applying space maintainers to paediatric patients.
1 INTRODUCTION
Early loss of primary teeth can lead to a decrease in arch length, crowding, midline deviation, impaction of permanent teeth, malocclusions, and degenerative and inflammatory problems in periodontal tissues due to tipping of adjacent teeth. Furthermore, this can also result in speech disorders, psychosocial changes, aesthetic problems, and temporomandibular disorders.1 Space maintainers (SMs) should be used to prevent the loss of space that may be encountered because of the early loss of the primary teeth and to protect the spaces that serve to obtain a functional and correct occlusion in permanent dentition.2
SMs can be designed as (i) fixed unilateral (band–loop [BL], crown–loop, and distal extension), (ii) fixed bilateral (lingual arch, Nance appliance, and transpalatal arch), or (iii) removable (partial dentures and Hawley appliance).2 Applications, however, are not limited to these today. Researchers have developed various techniques to overcome the limitations of traditional SMs such as multiple visits, metal allergies, solder breakage, band breakage, and appearance concerns. These methods aim to complete the SMs in one session, eliminating the need for laboratory processes. Some examples of these techniques include prefabricated SM kits, direct-bonded SMs, fiber-reinforced composite resin SMs, and SMs produced using computer-aided design/computer-aided manufacturing (CAD/CAM) technology with materials such as zircon, metal, polyetheretherketone, and resin.3-9 In dentistry, the use of CAD/CAM started with milling methods and later began to include the use of 3D printers. Laser sintering (LS) technologies are widely applied in dental practices today. Dentists employ this technology for both surgical and prosthetic purposes in adults, including custom-made implants, surgical templates, customized titanium meshes, scanbodies, and metal frameworks for removable prostheses and overdentures, where cobalt–chrome alloys can be replaced with titanium.10
CAD/CAM and 3D printing methods allow the production of SMs as a single piece, thereby eliminating solder breakage issues and enabling the use of more biocompatible materials such as zirconium and titanium.6-9 In addition, digital workflow simplifies the process of taking impressions from children. Moreover, transferring the scan to the laboratory as data helps prevent distortion.
It is imperative to note that a gap exists in the literature concerning comprehensive studies on SMs that are produced using digital workflow. Even though researchers have been utilizing CAD/CAM and 3D printing systems to create SMs and overcome the limitations of traditional SMs, accessible sources addressing this issue usually are case reports and comprehensive clinical studies on this matter are lacking.
This study aimed to compare the retention of and effects on periodontal health of SMs produced by digital workflow using the LS 3D-printing method (LS SMs) versus traditional BL SMs (T SMs) produced by traditional methods. For this study, T SMs were chosen for one group as they are the most commonly used SM type. For the other group, LS SMs were selected as they closely resemble T SMs in terms of form, and they offer advantages like the elimination of solder breakage and band breakage since they are produced as a single piece. Furthermore, LS SMs can be produced from more biocompatible material.
2 MATERIALS AND METHODS
A total of 70 patients aged 5–10 years (mean: 6.99 ± 1.18) who applied to the Akdeniz University Department of Pediatric Dentistry Clinic between January 2022 and January 2023 with the need for SM due to tooth loss were included in the study. The following criteria were sought for the patients to be included in the study: (i) between 5 and 10 years old, (ii) no previous experience with either alginate impressions or intraoral scanners (to accurately compare impression methods), (iii) no previous experience with SMs (to accurately compare impression methods), (iv) primary molar loss in the last 1 week due to caries, infection, and resorption (to eliminate possible space loss), (v) presence of the successor tooth germ (to justify the use of SM), (vi) presence of teeth in the mesial and distal end of the extraction cavity (to be able to install SM), (vii) no symptoms of pulpal pathology in the abutment teeth that will support SM (to prevent possible abutment tooth loss), (viii) class 1 occlusion (to prevent abnormal occlusal forces), (ix) no skeletal anomaly (to prevent abnormal occlusal forces), (x) presence of the antagonist tooth of the extracted tooth (to ensure there is an occlusal contact), (xi) at least 1 year to successor tooth to erupt (to ensure that the SM remains in the mouth until the end of the study), (xii) only one tooth loss in the same quadrant (to confirm the indication for a fixed SM), (xiii) no systemic disease (to guarantee the follow-up of the participants), and (xiv) no use of systemic antibiotics or any medication in the last 3 months (antidepressants, psychiatric drugs, etc.). Patients were excluded from the study: if (i) it has been a long time since tooth loss (to eliminate possible space loss), (ii) there was less than one year left for the permanent tooth to erupt(to prevent possible abutment toot loss), (iii) the primary second molar is lost early, but the permanent first molar has not erupted yet (due to the need for a distal shoe); (iv) cooperation was not achieved; (v) the patient's oral hygiene is not sufficient and has periodontal problems (to accurately asses the periodontal effects), and (vi) they did not meet the inclusion criteria.
2.1 Study groups
The sample size for our study was determined using the results presented in the study by Arıkan et al.11 In the phase of establishing an adequate sample size in the study, the GPOWER 3.1.9.4 program was utilized. The power analysis indicated that a sample size of 28 for each group, totaling 56, was anticipated for an effect size of 0.574, sensitivity of 0.05, and a power of 0.80. Considering the possibility of potential drawbacks, including the inability to conduct follow-up assessments with patients, it has been decided that each group should have a minimum of 40 SMs. Eighty-five SMs were placed in a total of 70 patients, 33 females and 37 males, who met the inclusion criteria and agreed to participate in the study. Participants were selected randomly in a balanced distribution according to the age and location of the abutment teeth, and two separate groups were formed, LS group and T group. In both groups, SMs were produced by an external laboratory. SM prototypes with different designs were prepared and tested on different models produced by the laboratory to reach a standard SM design as a pilot study preliminarily.
In the LS group, 40 SMs were performed on 34 patients (19 girls and 15 boys) with a mean age of 7.03 ± 1.41 years (Figure 1). Patients in this group were scanned under standard conditions by the same researcher (AC) with 3Shape TRIOS® 3 MOVE (Copenhagen, Denmark). Scanning was performed only in the quadrant with tooth loss. The scan data of the patients were sent to the laboratory via email in STL (.stl [The name STL is an acronym for stereolithography, a popular 3D printing technology. It is also called Standard Triangle Language or Standard Tessellation Language.]) format for SM design immediately after being recorded on the device. Scans were repeated if data loss or poor scan quality was encountered. The design of SMs was carried out on the DentalCAD 2.2 Valletta (Exocad GmbH, Darmstadt, Germany) program, and the production was made by the 3D LS (SLM Solutions, Germany) method using titanium-based metal powder (Ti64 Gd23; LPW Technology Ltd., Cheshire, UK). The production of LS SMs started after an ideal prototype was obtained in accordance with the T SM design in many points, such as the fit of the part surrounding the abutment tooth, thickness, and the position of the loop of LS SM. The band and loop thickness of LS SMs was set between 0.8 and 1 mm (due to the consideration that a thinner loop might have lower fracture resistance).

Forty-five SMs were performed on 36 patients (14 girls and 22 boys) with a mean age of 6.95 ± 0.91 years in the T group (Figure 2). Impressions were taken from the patients with sterilized plastic pedodontic impression trays (DuraLock, Turkey) and alginate (Orthoprint, Zhermack, Italy) under standard conditions by the same researcher (AC). Alginate was prepared with an alginate mixing device (Nova-Mix, President, Germany) in accordance with the manufacturer's instructions. After the impressions, plaster study casts (Elite Ortho, Zhermack, Italy) were produced and sent to the laboratory. SMs were produced by soldering the 0.7-mm bent orthodontic wires (Dentaurum, Germany) onto previously selected prefabricated molar bands. Prefabricated molar bands (Dentaurum, Germany) in the patient's mouth were chosen by the physician and then sent to the laboratory with the casts.

In order to fully assess clinical effectiveness, SMs were applied to both the maxilla and mandible, and for both the absence of the first and second primary molars. The distribution of SMs applied in the LS group according to missing teeth was as follows: 5 for tooth #54, 6 for tooth #64, 1 for tooth #55, 0 for tooth #65, 7 for tooth #74, 6 for tooth #75, 7 for tooth #84, and 8 for tooth #85. The distribution of SMs applied in the T group was as follows: 5 for tooth #54, 5 for tooth #64, 1 for tooth #55, 2 for tooth #65, 9 for tooth #74, 5 for tooth #84, 8 for tooth #75, and 8 for tooth #85.
All SMs were cemented by the same investigator (AC) under standard conditions using a glass-ionomer luting cement (Nova Glass-L, Imicryl, Konya, Turkey). Before cementation, isolation was achieved using cotton rolls and suction. Occlusal contacts and the adaptation of the SMs to the abutment tooth, the space and the adjacent tooth, and the gingiva were checked, and necessary arrangements were made. If any arrangement was made, SMs were polished with polishing rubbers. SMs were placed on the abutment tooth with the help of finger pressure after the luting cement was mixed by adjusting the powder/liquid ratio recommended by the manufacturer and applied to the inner surface of the part surrounding the abutment tooth. Occlusal contacts and the adaptation were checked again. After cementation, following approximately 2 min of waiting under isolation, any cement residues were removed with the aid of a probe. After the removal of cement residues, an additional waiting period of approximately 5 min was observed to allow for the cement to set. The patients and their parents were informed that the patients should not eat and drink for half an hour after the cementation procedure and not consume hard foods, such as hazelnuts and peanuts, and sticky foods, such as gum and jellybeans, on the SM. In addition, the patients were warned not to force the SM to remove with the help of objects such as toothpicks.
2.2 Clinical parameters
The clinical success of SMs was evaluated according to retention loss, and SMs were recorded as “Failed” if retention loss occurred in 6 months. Gingival Index (GI) and Plaque Index (PI) scores of the patients were recorded by a single investigator (AC) at the initial appointment and sixth-month controls based on the Silness–Löe12 values. The GI scores, ranging from 0 to 3, for each tooth were calculated by summing of the scores obtained from the buccal, lingual, mesial, and distal surfaces of the tooth and dividing it by four, with 0 representing healthy gums and 3 indicating very inflamed gums with spontaneous bleeding. The patient's overall GI was calculated by dividing the sum of scores from all teeth by the number of teeth. The PI scores, ranging from 0 to 3, for each tooth were calculated by summing the scores obtained from the buccal, lingual, mesial, and distal surfaces of the tooth, with 0 representing no visible plaque and 3 representing severe plaque accumulation with visible plaque present at the gingival margin and interdental spaces. The total score was then divided by four. The patient's overall PI was calculated by dividing the sum of scores from all teeth by the number of teeth. To determine the reliability, the first GI and PI measurements (before the impressions) and the second GI and PI measurements (before the cementation of SMs) made by the researcher on data from 10 randomly selected patients were evaluated. The rationale behind selecting GI and PI scores as criteria for evaluating clinical success is based on the findings, suggesting that fixed SMs negatively impact the periodontal health of abutment teeth.11, 13
- “Was the impression easy and fun?”
- “Did you have nausea during impression?”
- “Did you feel any discomfort during the impression (taste, odor, foreign body)?”
- “Did the impression take a short time?”
- “Would you like to have this impression experience again?”
2.3 Statistical analyses
Statistical analysis of the data was performed using the SPSS package program (SPSS 17.00 for Windows, Chicago, IL, USA) with descriptive statistics, reliability analysis (ICC), correlation analysis, and comparison tests. After the homogeneity of variance and normal distribution had been verified by Levene's test, for the evaluation of the quantitative data, “Student's t-test” and the Pearson correlation analysis were used. For nonparametric qualitative data, the Mann–Whitney U and chi-squared tests were used. Survival times were evaluated with the Kaplan–Meier test, and the difference was tested with the log-rank (Mantel–Cox) analysis. The results were evaluated at the 95% confidence interval, at the p < .05 significance level.
3 RESULTS
ICC values for the intra-observer agreements on GI and PI scores were found to be 0.946. There was no statistically significant difference between the first and second measurements.
This study was completed with 32 patients (17 girls and 15 boys) in the LS group and 33 patients (11 girls and 22 boys) in the T group since two patients from the LS group and three patients from the T group were lost to follow-up due to various reasons (changing phone numbers, moving to different locations, etc.). There was no significant difference in the distribution of SMs among the groups after excluding patients. No statistically significant difference was found in terms of the age and gender of the patients in the groups. There was no significant difference between the groups according to the distribution of SMs by missing teeth. In the LS group, 38 SMs were performed on 32 patients; in the T group, 42 SMs were performed on 33 patients.
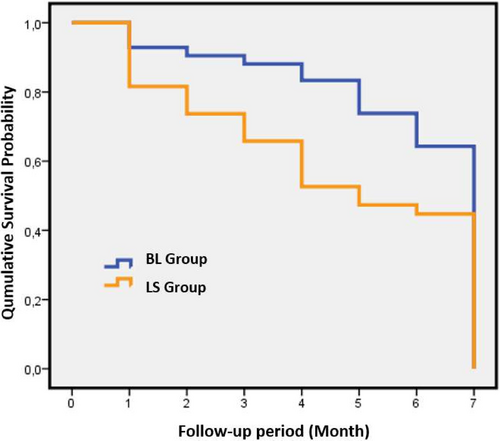
3.1 Evaluation of the retention
Sixteen (38%) SMs from the T group and 25 (66%) SMs from the LS group were recorded as failed due to retention loss. Problems such as solder breakage, band breakage, and soft tissue lesions were not observed in the failed SMs, and it was observed that the reason for the failure of all SMs was decementation. Failure rates were statistically higher in the LS group than in the T group. When clinical success was evaluated based on the type of abutment tooth, no significant difference was found in both groups. Age and gender did not have a statistically significant effect on clinical success. According to the Kaplan–Meier test results, the survival of SMs within the 6-month follow-up period was determined as 5.929 ± 0.284 months for T SMs and 4.658 ± 0.396 months for LS SMs (Figure 3). When the survival times of the T and LS group SMs were compared, a significant difference was found according to the log-rank (Mantel–Cox) test.
3.2 Evaluation of the effect on periodontal health
No significant difference has been observed between the groups when comparing the GI and PI values obtained from the abutment teeth and from the full mouth, initially and at the sixth month (Table 1).
| Abutment teeth | Full mouth | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T group | LS group | p | T group | LS group | p | |||||
| N | Mean ± SD | N | Mean ± SD | N | Mean ± SD | N | Mean ± SD | |||
| Initial GI | 42 | 1.12 ± 0.300 | 38 | 1.12 ± 0.300 | .925 | 33 | 1.01 ± 0.137 | 32 | 0.99 ± 0.130 | .549 |
| Sixth-month GI | 42 | 1.36 ± 0.316 | 38 | 1.36 ± 0.316 | .129 | 33 | 0.99 ± 0.100 | 32 | 0.96 ± 0.100 | .236 |
| Initial PI | 42 | 1.19 ± 0.339 | 38 | 1.19 ± 0.339 | .433 | 33 | 1.04 ± 0.167 | 32 | 1.01 ± 0.156 | .573 |
| Sixth-month PI | 42 | 1.43 ± 0.401 | 38 | 1.43 ± 0.401 | .631 | 33 | 1.00 ± 0.106 | 32 | 0.99 ± 0.133 | .572 |
- Abbreviations: LS group, laser sintering group; T group, traditional group.
Full-mouth GI and PI values at the sixth month were lower in both the LS and T groups than initial values. The decrease in all values, except for the decrease in the GI values of the T group, was found to be statistically significant (Table 2). In both groups, GI and PI values of the abutment teeth were significantly increased at the sixth month compared with initial records (Table 3).
| LS group | T group | |||||||
|---|---|---|---|---|---|---|---|---|
| Initial | Sixth month | p | Initial | Sixth month | p | |||
| N | Mean ± SD | Mean ± SD | N | Mean ± SD | Mean ± SD | |||
| GI | 32 | 0.99 ± 0.130 | 0.96 ± 0.100 | .001 | 33 | 1.01 ± 0.137 | 0.99 ± 0.100 | .001 |
| PI | 32 | 1.01 ± 0.156 | 0.99 ± 0.133 | .008 | 33 | 1.04 ± 0.167 | 1.00 ± 0.106 | .064 |
- Bold characters stand for the significant findings.
- Abbreviations: LS group, laser sintering group; T group, traditional group.
| LS group | T group | |||||||
|---|---|---|---|---|---|---|---|---|
| Initial | Sixth month | p | Initial | Sixth month | p | |||
| N | Mean ± SD | Mean ± SD | N | Mean ± SD | Mean ± SD | |||
| GI | 38 | 1.12 ± 0.300 | 1.36 ± 0.316 | .002 | 42 | 1.11 ± 0.260 | 1.47 ± 0.311 | .021 |
| PI | 38 | 1.19 ± 0.339 | 1.43 ± 0.401 | .001 | 42 | 1.13 ± 0.345 | 1.47 ± 0.377 | .049 |
- Bold characters stand for the significant findings.
- Abbreviations: LS group, laser sintering group; T group, traditional group.
3.3 Evaluation of the survey results
Considering the survey results in which the impression technique was evaluated, it was observed that the number of patients who answered “Yes” to the questions 1, 4, and 5, for which the “Yes” answer was accepted as positive, was quite high in the LS group compared with the T group; and the number of patients who answered “Yes” to the questions 2 and 3, in which the “Yes” answer was accepted as negative, was higher in the T group than in the LS group. To the first question of the survey, translated as “Was the impression easy and fun?”, 22% (8/36) of the patients in the T group answered “Yes,” while 97% (33/34) of the patients in the LS group answered “Yes.” To the second question, translated as “Did you have nausea during impression?”, while 70% (25/36) of the patients in the T group answered “Yes” to the question, only 2.9% (1/34) of the patients in the LS group answered “Yes.” While 91.6% (33/36) of the patients in the T group answered “Yes” to the third question translated as “Did you feel any discomfort during the impression (taste, odor, foreign body)?”, only 8.8% (3/34) of the patients in the LS group answered “Yes.” Only 16.6% (6/36) of the patients in the T group answered “Yes” to the fourth question, translated as “Did the impression take a short time?”, while 100% (34/34) of the patients in the LS group answered “Yes.” To the fifth and last question of the survey translated as “Would you like to have this impression experience again?”, only 5.5% (2/36) of the patients in the T group answered “Yes,” while 100% (34/34) of the patients in the LS group answered “Yes.”
4 DISCUSSION
Researchers have been investigating the clinical effectiveness of different types of SMs, as well as how design and construction factors affect their survival time.5, 14-19 Studies have shown that the success rate of SMs can range from as high as 92%14 to as low as 27%.18 We have noticed that there has not been a thorough clinical study conducted on the effectiveness of SMs made through 3D printing. This study will be the first of its kind in this field. Among the SMs used to protect the space caused by premature loss of primary teeth, BL SMs are the most commonly used and have been chosen for their high success rates over a long period of time.2, 16, 17 Therefore, we compared LS SMs with BL SMs in terms of clinical success and oral hygiene effects.
According to a study conducted by Tahririan et al.,14 the success rate of BL SMs was found to be 92%. The study compared SMs produced with prefabricated bands and traditional methods, and there was no significant difference between the two groups. Reported success rates from other studies for BL SMs were 90% by Tunc et al.,17 86.7% by Mittal et al.,19 and 84.6% by Setia et al.,20 and these success rates were quite close to each other. On the contrary, Sasa et al.15 reported a success rate of 42.5% in the study in which they followed BL SMs in the long term. In our study, the success rate of T SMs was 62%, and the success rate of LS SMs was 34%. It is thought that the biggest reason for the inconsistency in the success of T SMs between the previous studies14, 17, 19, 20 and this study may be the luting cement used. In order to evaluate this situation, there is a need for more comprehensive studies investigating different luting cements.
Due to the absence of comprehensive clinical studies on LS SMs, it is not possible to compare the success rates of LS SMs in our study with the aforementioned studies. To the best of our knowledge, the first academic publication on LS SMs, presented as a case report, was authored by Pawar.7 The researcher placed a 3D-printed SM in a 7-year-old patient due to the early loss of the mandibular left first primary molar and reported that no problems were encountered with SM in clinical observations at the third-month follow-up. Subsequently, Khanna et al.21 and Rana et al.22 also published case reports with short-term follow-ups on LS SMs and reported that they found the SMs satisfactory.
An in vitro study by Tokuc and Yilmaz23 examined the fit accuracy of SMs to abutment teeth in a computer environment, comparing 3D printed (LS) SMs to BL SMs. The researchers found no significant difference between the two groups. They, however, noted that 3D printing requires the removal of undercut areas that provide retention on the abutment tooth to create an entry route to the SM. They also mentioned that 3D-printed SMs can be thicker and harder than prefabricated molar bands. It has been found in our study that LS SMs have a high failure rate of 66% within 6 months and that there was a significant difference between LS SMs and T SMs in terms of retention and survival time. This may be due to the removal of undercut areas during the design process, as noted by Tokuc and Yilmaz,23 or leaving excess cement space. Nevertheless, according to Baroni et al.,16 it is essential to consider occlusal stresses rather than design when evaluating the long-term use of SMs. The inflexibility of LS SMs under occlusal forces may also contribute to their high failure rate, as they are less flexible than T SMs. Moreover, the fact that elastic orthodontic separators were not used before the application of LS SMs in the study may have contributed to the failure rate. The authors of the study believe that further research on LS SMs is necessary, and they have recommendations to prevent high rates of retention loss in LS SMs. One of these recommendations is the application of elastic orthodontic separators before scanning, and the other is to maintain communication with the laboratory during the manufacturing process to create SMs as thin as possible with minimal cement space to allow for entry.
When we compared the effects of SMs on oral hygiene, no significant difference was found between the two groups; our study, however, showed that the GI and PI values of the abutment tooth increased regardless of the type of fixed SM. In line with our research, Arıkan et al.11 found that the PI and GI values of teeth adjacent to SM increased significantly in the first and third months compared with the initial records. Likewise, the study conducted by Hosseinipour et al.,13 which investigated the impact of removable and fixed SMs on oral hygiene, revealed a considerable increase in pocket depth, GI, and bleeding-on-probing scores in areas with fixed SMs at the sixth month. Furthermore, in this study, we observed a decrease in the general PI and GI scores of the patients. One possible explanation for this could be the Hawthorne effect,24 which refers to the phenomenon where subjects alter their behavior positively when they are aware that they are being monitored. To reduce the adverse effects of fixed SMs on the periodontal health of abutment teeth, oral hygiene motivation can be provided to patients at control appointments by visualizing the plaque on the abutment teeth using the plaque disclosing method.
It is known that children interpret the impression experience as an unpleasant situation.25-28 Taking impressions from children is difficult as it can cause a gag reflex. A gagging sensation is especially common during maxillary impressions because the impression material is in contact with the soft palate. In addition, it has been pointed out that the feeling of drowning during a dental impression is one of the most common fears of children.28 While research with adults has yielded varying results in terms of preference for impression technique and time required for impression-taking,29-31 studies involving children have shown that they tend to prefer digital impressions over alginate-based impressions.25-27 Burhardt25 reported that although alginate impressions could be obtained quickly, children still preferred digital impressions. Mangano et al.26 and Yılmaz et al.,27 however, found no significant difference in impression time between the digital and conventional methods, and children showed a preference for digital impressions. The findings of this study suggest that children perceive digital impressions as a more positive and shorter experience.
The importance of space maintenance procedures in paediatric dentistry is undeniable. The disadvantages of traditional SMs have been previously discussed in the article, and to overcome these drawbacks, it is necessary to work with SMs produced using different methods in a clinical setting. This study is the first comprehensive resource, based on the information obtained from accessible sources that can shed light on paediatric dentists regarding SMs produced with 3D printing-LS technique. Based on the findings of this study, considering the positive perceptions of children about the procedure and the fact that the effects of LS SMs on periodontal health are similar to T SMs, it is thought that LS SMs can be used routinely in paediatric dentistry. It would be beneficial to utilize digital workflow more frequently. Further comprehensive research focusing on the design of LS SMs that overcome the limitations of our study is necessary for their widespread use in paediatric dentistry.
If we discuss the limitations of our study, despite efforts to ensure equal distribution of SMs among groups based on tooth numbers, it was not exactly equal. Due to variations in patients' tooth sizes and different stages of development, extraction spaces varied in length. Even though patients with Class 1 occlusion were selected for the study, due to minor misalignments, patients' occlusions were not entirely identical. Differences in patients' dietary habits may have had varying effects on the SMs. In this study, only a single luting cement was used, and it is necessary to explore the use of different cements.
AUTHOR CONTRIBUTIONS
Hüseyin Karayilmaz and Ayşe Cengiz determined the concept and design of the study, gave their final approval on the version that will be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ayşe Cengiz collected the data. Hüseyin Karayilmaz analyzed the data. While Ayşe Cengiz was drafting the work, Hüseyin Karayilmaz critically reviewed the work for important intellectual content.
ACKNOWLEDGMENTS
The financial support for this study was provided by the Akdeniz University Scientific Research Projects Coordination Unit (Project ID: TDH-2022-6140).
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest between the authors or any organization.
ETHICS STATEMENT
This study was ethically approved by the Akdeniz University Clinical Research and Ethics Committee (Date: March 30, 2022, No.: 205) and conforms to the recognized required standards of the Declaration of Helsinki. The parents of the patients who agreed to participate in the study were informed about the study in detail, and their consent was obtained.
Open Research
DATA AVAILABILITY STATEMENT
The data supporting this study's findings are available upon request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.