Laparoscopic off-clamp partial nephrectomy using soft coagulation
Abstract
Objectives
To assess the effectiveness of soft coagulation in off-clamp laparoscopic partial nephrectomy.
Methods
A total of 32 patients with renal tumors underwent laparoscopic partial nephrectomy with off-clamp using soft coagulation between May 2012 and September 2013. Tumor resection was carried out using a combination of bipolar forceps and a ball electrode using the soft coagulation system without hilar clamping. The outcomes of these patients were compared with those of 30 patients treated with hilar clamping.
Results
This off-clamp procedure was successfully completed in 31 cases. No significant differences were observed in the mean age (60 vs 61 years), sex (male/female; 25/7 vs 20/10), mean RENAL nephrometry score (5.7 vs 5.8), mean body mass index (24.4 vs 23) or tumor size (15 mm vs 16 mm) between the two groups. No significant differences were noted in positive surgical margins (0 vs 0) or blood loss (104 vs 115 cc) as well. In contrast, a significant difference was noted in the total operative time (278 vs 238 min). Serum creatinine percentage changes at 3 months were 6.4 versus 7.3% in the off-clamp and hilum-clamp groups, respectively, which were not significantly different.
Conclusions
Off-clamp laparoscopic partial nephrectomy can be safely carried out by using a soft coagulation technique.
Abbreviations & Acronyms
-
- LPN
-
- laparoscopic partial nephrectomy
-
- PN
-
- partial nephrectomy
-
- RPN
-
- robot-assisted laparoscopic partial nephrectomy
Introduction
The usefulness of PN in avoiding the risk of chronic kidney disease and other cardiovascular diseases as a result of radical nephrectomy has already been reported.1
Nephron-sparing surgery is the standard treatment for small renal masses.2-4 Radical nephrectomy was previously indicated for the surgical treatment of small renal cancer; however, the importance of functional conservation has recently been shown, has widely promoted the recognition of PN and has been recommended in recent guidelines.5-7 Although LPN is recommended, the necessity of carrying it out in limited facilities has been emphasized, because it requires specialized resection and suture techniques.6
The main difficulty associated with partial nephrectomy under ischemia is that accurate resection and suturing have to be carried out within a limited time. Furthermore, the suture needle itself has occasionally been reported to transect or puncture the artery, leading to renal artery pseudoaneurysm.8
In contrast, shortening the warm ischemia time and avoiding volume losses are important for conserving renal function in PN, and various modifications have been made to achieve this. Zero ischemic PN9, 10 and robotic surgery11, 12 have been applied for PN. Renorrhaphy, which is typically carried out during this surgery, was avoided in order to minimalize volume losses.
A modern electrosurgical generator, the VIO300D (ERBE Electro “SOFT COAG”; ERBE Elektromedizin GmbH, Germany), has a unique coagulation output mode called “SOFT COAG” that automatically regulates its output voltage to be maintained below 190 V, which generates Joule heating alone and no tissue carbonization. Proteins within the target tissue are effectively coagulated at temperatures between 70 and 80°C as a result of Joule heating generated in the tissue.13 In addition, the monopolar and bipolar (cut and soft coagulation) modes were also used in the present study. Thus, we herein carried out off-clamp PN by soft coagulation using a monopolar electrode and bipolar forceps, and sutures were not applied if possible.
Methods
A total of 32 patients underwent LPN with off-clamp using the SOFT COAG output of the VIO 300D system at our hospital between May 2012 and September 2013. Patients with T1, who were regarded as technically appropriate for LPN by the Tumor Board and consented to undergo this procedure without hilum clamping were examined. Generally, our indications for LPN with off-clamp were T1 cancer of non-hilar and nearness of the tumor to the collecting system over 4 mm. Exclusion criteria were severe cardiovascular or pulmonary risks that were considered unendurable for general anesthesia by anesthesiologists.
The outcomes of these patients were compared with those of 30 patients treated with LPN with conventional hilum clamping between September 2010 and March 2012. The procedure was carried out by two surgeons (FH and AK).
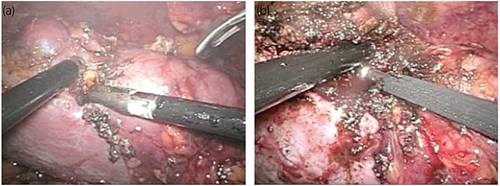
After the standard preparation of laparoscopic partial resection, the hilum of the kidney was confirmed and treated to prepare for the rapid application of clamps with forceps. Intraoperative ultrasound was used to confirm the margins of the mass. Tumor resection was then carried out using the combination of bipolar forceps (Olympus Corporation, Tokyo, Japan) and a ball electrode (IO electrode) with a tip diameter of 4 mm (Slimline hand switch). Bipolar forceps were set to Effect 2 and 40 W in auto-cut and set to the SOFT COAG mode at Effect 5 and 40 W connected to VIO300D. Bipolar forceps were inserted into the kidney parenchyma along the incision line, and soft coagulation was applied to the held tissue, followed by a bipolar cut to transect the tissue. The kidney parenchyma was then bluntly dissected using forceps, and soft coagulation and a bipolar cut were similarly applied to the funiculus (Fig. 1a). After the temporary control of bleeding, the ball electrode connected to VIO300D was placed against the bleeding point (Fig. 1b). SOFT COAG was set at Effect 7 and 80 W. After tumor resection, soft coagulation was applied to the resected bed. Indigo carmine was dripped through a urethral catheter inserted beforehand to confirm opening of the urinary tract. In the case of opening of the urinary tract, the pelvicalyceal entry was suture-repaired in a watertight manner. A fibrin glue (Bolheal; Kaketsuken, Kumamoto, Japan) with polyglactin acid sheet (Neoveil; Gunze Limited, Kyoto, Japan) were applied to the resected bed, and this was followed by the placement of a drainage tube. Hemostatic suture repair of the PN bed was not typically carried out during this surgery. A surgical bolster was not used for the tumor-resected bed.
Information was reviewed from the imaging, operative, anesthesiology and pathology reports, as well as from the discharge and laboratory records. The RENAL nephrometry score14 was used to grade the complexity of the kidney tumor and define its hilar location. The Clavien Classification of Surgical Complications was used for surgically related complications.15 The chi square χ2-test and t-test were used for statistical analyses, which were carried out using JMP 10.0.2 (SAS Institute Japan Ltd, Tokyo, Japan).
Results
This procedure was carried out on 32 patients with renal tumors between September 2012 and November 2013, and surgery was successfully completed in 31 cases. There were 30 cases of RCC and two cases of angiomyolipoma. The control of bleeding in one case was considered difficult during tumor resection under partial ischemia; therefore, the procedure was switched to renal artery clamping using bulldog forceps.
Baseline patient demographics, tumor characteristics, operative outcomes and pathological results are listed in Table 1. Renorrhaphy or repair of the collecting system was not carried out in 25 patients. No significant differences were observed in the mean age (60 vs 61 years), sex (male/female; 25/7 vs 20/10), mean RENAL nephrometry score (5.7 vs 5.8), mean body mass index (24.4 vs 23) or tumor size (15 vs 16 mm) of the off-clamp and hilum-clamp groups. Peri- and postoperative parameters are shown in Table 2. No significant differences were noted in positive surgical margins (0 vs 0), or mean blood loss (104 vs 115 cc) of these two groups. In contrast, a significant difference was detected in the mean total operative time (278 vs 238 min). No high-grade complications were noted postoperatively in either group. One patient in the off-clamp group developed urinoma (grade 3).
| Off-clamp | Hilum-clamp | P-value | |
|---|---|---|---|
| 32 | 30 | ||
| Mean age (range) | 60 (30–74) | 61 (47–74) | 0.4438 |
| Sex (male/female) | 25/7 | 20/10 | 0.3122 |
| Mean body mass index (range) | 24.4 (18–31) | 23 (19.2–27.3) | 0.1941 |
| Mean RENAL nephrometry score (range) | 5.7 (4–10) | 5.8 (4–9) | 0.7740 |
| Mean tumor size, mm (range) | 15 (9–59) | 16 (9–40) | 0.9905 |
| Histology (RCC/benign) | 30/2 | 29/1 | 0.9543 |
| Off-clamp | Hilum-clamp | P-value | |
|---|---|---|---|
| Blood loss (mean) | 104 | 115 | 0.662 |
| Operative time (mean) | 278 | 238 | <0.05 |
| Clamping time (mean) | 0 | 31.8 (21–57) | <0.001 |
| Positive margins | 0 | 0 | |
| Mean change in serum creatinine to 3 months (%) | 6.4 (–2–35) | 7.3 (0–43) | 0.9508 |
No significant changes were observed in serum creatinine levels before and 3 months after surgery in the off-clamp group (0.833 before and 0.931 3 months after surgery) and hilum-clamp group (0.816 and 0.900, respectively). Serum creatinine percentage changes at 3 months were 6.4 vs 7.3% in the off-clamp and hilum-clamp groups, respectively, which were not significantly different.
Discussion
PN for small renal masses is well established and achieves excellent functional and oncological outcomes. More urologists need to undertake the technical challenges associated with this procedure, especially in laparoscopic surgery.
Various energy devices have been investigated in an attempt to overcome these issues, including an ultrasonically activated bending scalpel,16 water-jet dissector,17 diode laser,18 floating-ball radiofrequency dissector,19 microwaves20 and radiofrequency coagulation.21 These devices are very useful for intraoperative hemostasis and can control bleeding. However, the margin cannot be readily decided, because differentiating between normal renal tissue and the tumor is difficult. Thus, heat damage to the surrounding tissue, such as arteries, veins and the calix, is a matter of concern. Unexpected collateral thermal damage to the surrounding structures, especially the collecting system, can cause urinoma, pelvicalyceal stenosis and renal arteriovenous fistula.20-23 Therefore, the indication of LPN might be limited to small protruding tumors.
Open partial nephrectomy using soft coagulation without renorrhaphy was recently carried out on 39 patients, and appeared to be safe and feasible in previous study.24 In this study, the renal artery was clamped in the initial 23 cases (59%). The remaining 16 surgeries (41%) were carried out without clamping.
SOFT COAG is a type of electrical scalpel that differs from conventional electrical scalpels. It is regulated to produce less than 190 V, thereby causing Joule heating only without any electrical discharge. Joule heating degenerates proteins and stops bleeding without any carbonization. This electrical mechanism is considered to achieve the reliable hemostasis of SOFT COAG. Furthermore, SOFT COAG was shown to degenerate proteins to a depth of less than 2 mm from the resected surface.25 In a previous study using the porcine kidney, the temperature of the surface using the 80 W Effect 7 was reported to be 88.3°C.26 The temperatures of the kidney at depths of 5 mm and 7 mm were 58.0°C and 31.5°C, respectively, under the same condition.27 Damage to renal function might be limited, because the heat produced by SOFT COAG is localized. SOFT COAG is similarly useful for laparoscopic surgery. Modifications (soft coagulation using bipolar forceps, incision by a bipolar cut using bipolar forceps in the resection procedure and hemostasis applied to the bleeding point using an IO electrode) to the procedure used in open surgery enabled the use of SOFT COAG for LPN. Furthermore, the volume of blood loss was small.
We avoid suturing and used Neoveil, a hemostatic sheet, except when it was necessary to close an opening in the renal pelvis, because arterial puncture with a suture needle is one of the causes of false aneurysm, a complication of partial nephrectomy.8 Therefore, the risk of arterial puncture was reduced in the present procedure as long as the renal calyx was not opened. As parenchymal sutures cause renal hypofunction (volume loss), the suture-less procedure is advantageous, as it prevents this.
A follow up of postoperative renal function was carried out 3 months after surgery. Changes in serum creatinine levels were similar to those after conventional non-ischemic or robot-assisted approaches; Rais-Bahrami et al.27 examined 126 cases and % creatinine was 9.5%, Gill et al.9 examined 58 cases, and % creatinine was 20%, whereas Rizkala et al.10 examined 14 cases, and % creatinine was 7.3% (Table 3). Volume loss might have the greatest influence on postoperative renal hypofunction. Hung et al.28 carried out a sophisticated analysis that normalized functional loss by parenchymal loss; however, parenchymal loss was estimated subjectively, leaving valid concerns about potential bias. Although no marked difference was noted, this non-ischemic procedure without suture-induced volume loss could be promising.
| Method/ischemic time | n | Tumor size (mm) | Estimated bleeding | Change of serum creatinine (%) | |
|---|---|---|---|---|---|
| Rais-Bahrami, 2011 | Off-clamping | 126 | 24 | 334 | 9.5 |
| Gill, 2012 | Off-clamping | 58 | 32 | 206 | 20 |
| Rizkala, 2013 | Off-clamping | 14 | 22 | 193 | 7.3 |
| Present series | Off-clamping | 30 | 21 | 104 | 6.4 |
| Scoll, 2010 | RPN 25 min | 100 | 28 | NA | 7.6 |
| Naeem, 2011 | RPN 24 min | 97 | 24 | NA | 7.4 |
Urinoma developed in one patient, and might have been as a result of the application of sutures to only a single layer without parenchymal sutures.
Although the advantages associated with robot-assisted surgery for the ischemia time and incidence of complications has frequently been reported, its cost might be a challenge. The new technique is applicable wherever soft coagulation systems are available, including facilities that cannot use costly robots. Furthermore, it could contribute to warm ischemia time shortening, which is of particular importance when carrying out laparoscopic surgery. The advantage of this procedure is its lower cost than that of robot-assisted surgery, a shorter ischemia time than that of laparoscopic surgery and the absence of a time limit for sutures, which might enable inexperienced operators to carry out this surgery.
There were several limitations to the present study. The total number of surgical cases was too small to reach definite conclusions. Furthermore, this was a retrospective study. Therefore, controlled randomized trials need to be designed that compare SOFT COAG with conventional hilum clamping in laparoscopic PN.
This new technique using soft coagulation is considered to be safe and feasible for LPN.
Conflict of interest
None declared.


