Implementation of clinical guidelines for secondary prevention of stroke
Secondary stroke prevention involves more than the avoidance of recurrent stroke; it also aims to prevent other serious vascular events and maintain physical and mental functioning in patients 1. Yet, the biannual Australian National Stroke audit 2 has shown little change in use of secondary prevention strategies since 2009, despite several guidelines including the NHMRC Clinical Stroke Guidelines in 2010 3. Clinical practice guidelines need to be supplemented by other activities for effective changes or improvements in care 4.
We evaluated a low-cost implementation package driven by two local champions involving education (all medical, nursing and allied health staff and local GP networks), a checklist in patient files, and postcards for GPs, to close an identified gap for secondary stroke prevention in a tertiary and regional hospital. Senior clinicians agreed to change their practice after being made aware of the NHMRC guideline, and junior doctors were motivated to complete the checklist during the patient's stay.
Ninety patients were enrolled in the study at the tertiary hospital over six-months and of these, 99% of patients were discharged on an antithrombotic agent, 94% on antihypertensive(s), and 97% on a statin. For the 68 patients at the regional hospital, the figures were 100%, 92% and 97%, respectively. Patient follow-up was at three- and six- to nine-months and showed a sustained improvement in secondary prevention. The intervention was still effective at the hospitals one-year later (Fig. 1).
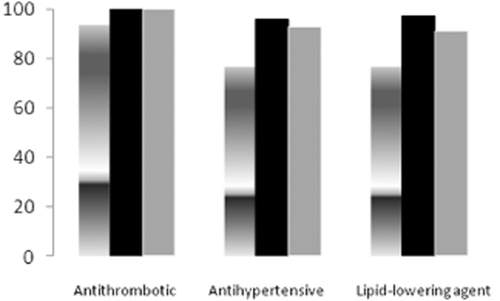
Data for tertiary referral hospital: shaded column represents discharge data prior to intervention, black column represents discharge data at time of intervention, and gray column represents data at discharge in the year after the intervention.
Reasons for the lack of implementation of guidelines are multiple and complex: lack of knowledge, poor access to information, and organizational and financial factors 4. This study demonstrates that a simple intervention in conjunction with an enthusiastic stroke unit coordinator, who can sustain practice in the context of junior medical staff turnover, is effective in bridging an evidence-practice gap.