Cost evaluation of an innovative outreach clinic across social insurance codes in rural Northern Germany — A routine data analysis
Abstract
A community outreach clinic was established in 2013 in a rural part of Germany to counsel and better integrate patients with mental health disorders or clients with psychosocial problems into the healthcare and complementary social assistance system. In a pilot study, we aimed to evaluate the costs of the integration assistance system after the outreach clinic was opened, the number of visits and the trend in the costs of the social assistance system of the federal state. Anonymised secondary cost data were used to evaluate the costs associated with the integration assistance receivers before (2010–2012) and after the establishment of the outreach clinic (2013–2015). Total costs were descriptively compared between the intervention group (consultation in the outreach clinic), the non-referral group, and a propensity score-matched control group for the years 2013–2015. To monitor the counselling activity, we used anonymised data on visits to the outreach clinic between 2013 and 2015. Data from 50 clients in the outreach clinic and 678 non-referral clients were analysed. The total costs of the integration assistance for the years 2013–2015 amounted to EUR 21,516 (95% CI 14,513–28,518) and EUR 28,464 (25,789–31,140) respectively. Propensity score matching of the controls resulted in equalised total costs for the years 2013 through 2015 for clients (n = 50, EUR 21,516 (14,513–28,518)) and controls (n = 250, EUR 21,725 (18,214–25,234)). The total number of integration assistance receivers in the district was lower than the average for the federal state. The number of consultations at the outpatient clinic steadily increased from 146 in 2013 to 1,090 in 2015. Counselling in the outreach clinic might help reduce the placement of clients into integration assistance, including supported housing, and slow the expected cost trend. However, counselling failed to lower total costs in the integration assistance service, possibly due to the selection of more severe cases.
What is already known about this topic?
- Navigation through the health and social care system in Germany is difficult for people with psychosocial needs because of the sector boundaries of service providers and paying authorities and different Social Code Books.
- Different forms of case management or integrated care have been shown to be effective in facilitating individually tailored demand-oriented services for clients and efficient in preventing permanent cost increases in the health and social care system.
What this paper adds
- Installing an innovative cross-sectoral psychosocial outreach clinic working within two different Social Code Books seems to slow the expected increase in cases and costs of social integration assistance in the clinic's catchment area.
- The model might help to control the excessive placement of clients with little need for social care in the form of integration assistance and thereby save resources for those more severe cases who truly need integration assistance services
1 INTRODUCTION
The German healthcare system is divided into various sectors of outpatient and inpatient acute care, rehabilitation, integration assistance and social support (Amelung, Hildebrandt, & Wolf, 2012; Busse & Blümel, 2014). Within these sectors, psychosocial and healthcare is delivered based on several social insurance codes (12 Code Books regulating healthcare, rehabilitation of disabled persons, pension schemes, unemployment compensations and welfare (Federal Ministry of Labour and Social Affairs, )). While prevention, acute and long-term medical and psychotherapeutic treatment are provided according to Statutory Health Insurance, long-term nursing care is based on Social Long-term Care Insurance. Benefits and services aiming to promote participation in education, the labour market and social activities comprise medical, occupational and social rehabilitation and are covered by Pension Insurance, Statutory Health Insurance, or Unemployment Insurance, depending on individual conditions. Finally, integration assistance is part of the welfare-oriented social assistance system. Integration assistance aims at the inclusion of persons with disabilities and comprises assistance for living in institutions, sheltered housing, assistance for employment and day structuring and measures to participate in the community.
Clients who seek any form of psychosocial help find it difficult to identify which of the various offers of care might be relevant to their individual situation and to which benefits they are entitled. Case management or outreach clinics that help clients navigate the provision of care are not implemented for the whole population but are currently only available in limited schemes, where access is restricted to a certain region or for insurants of selected insurance funds based on a pilot project (Fisher & Elnitsky, 2012; Rutz, 2001; Weinmann & Gaebel, 2005). This is especially the case in Germany because there is no formal cooperation between stakeholders and authorities of the various social insurance codes in Germany. In addition, the financing of services is the responsibility of various social insurance bodies (Schmid, Steinert, & Borbé, 2013; Weinmann & Gaebel, 2005). The overall planning of health and social care for the population in need is conducted by several authorities separately, based on the different legal bases of the Social Security Codes. This fragmentation of care ultimately leads to expensive but inadequate care for people with psychosocial needs (Organisation for Economic Co-operation and Development (OECD), 2019). Overcoming the fragmentation of prevention, acute and long-term healthcare and social care is one of the grand challenges of the German health and social care system (Brandhorst, Hildebrandt, & Luthe, 2017). While the German government is making efforts to promote integrated care in the Health Insurance System, there are no approaches to promoting care across Social Code Books (Milstein & Blankart, 2016). Low-threshold cross-sectoral services that are easily accessible for individuals with a maximum of staff continuity from the client's perspective is urgently needed as a component in Germany's routine care (Greve, 2018). Cross-sectoral service and cooperation across Social Code Books is particularly important for patients with psychosocial needs, the chronically ill and disadvantaged population groups.
Various concepts and models to integrate healthcare and social services exist; however, most of them stem from Anglo-American healthcare systems and are available only for a circumscribed group of diagnoses or insured persons or for a limited region (Fisher & Elnitsky, 2012). Particular models that integrate individual healthcare sectors and social work have shown a benefit in health and quality of life, for example, in primary care (McGregor, Mercer, & Harris, 2018) or in intensive interventions in a day care unit (Murphy et al., 2017). Existing models from outside Germany differ considerably in intensity, location, and range of integration; however, they are not easily transferable to the German healthcare system because Germany's self-governance system has no lead common control level for all health and social care services. A large population-based integrated care model in Germany promised cost savings and high quality of care; however, it does not include the different Social Code Books but operates cross-sectoral (integrating inpatient and outpatient sector) solely within the healthcare sector (Busse & Stahl, 2014). There was one attempt to establish an integrated mental healthcare model across Social Code Books in Germany that failed as a result of the different goals held by the actors involved, therefore, no evaluation is available (Peters, 2018). Beyond this, there are no published experiences of cross-sectoral cooperation for the German health and social care system to date.
Helpful approaches in the German health and social care system would first place the planning of psychosocial care in the hands of a lead institution; second, finance psychosocial care from a common budget; and third, formalise the cooperation of service providers from different institutions across the Social Code Books.
Such a model has been developed in a rural administrative district in the German Federal State of Schleswig-Holstein. In the first step, common planning of psychosocial care and formalised cooperation between service providers were established in the form of a psychosocial outreach clinic jointly operated by the legislative body of the district in cooperation with the major provider of mental healthcare. The aim was to offer any help-seeking persons individual counselling to help them avoid receiving inappropriate services from the various psychosocial and healthcare providers and particularly to prevent them from being inappropriately institutionalised in psychiatric inpatient care or supported housing. This model follows the concept of Steinhart and colleagues, who proposed a central coordinating and counselling service as the basic component of community mental healthcare (Steinhart & Wienberg, 2016, 2017). The psychosocial outreach clinic offers psychosocial counselling to the entire population of the district (approx. 130,000 inhabitants). Counselling is provided in two centrally located offices as well as at clients’ homes on request. Counselling includes support with psychosocial problems as well as the coordination of healthcare and complementary services received independently from providers. Hence, the model goes far beyond Steinhart's concept, as it addresses all clients with a need for psychosocial counselling in the district and allows for a demand-oriented low-threshold service across various social insurance codes. The outreach clinic was established by the two shareholders, namely, the municipal hospital of the district and the administrative district, which bears the cost of integration assistance and supported housing, financed by a different social insurance code. The setup is embedded in a policy aiming at the long-term transformation of care in the district's community. Within this strategy, mental healthcare in the district has been financed since 2008 using a capitation principle (Regional Psychiatry Budget and pilot programme (Modellvorhaben) according to §64b Social Insurance Code Book V, (König et al., 2010)). The capitation principle covers inpatient, day care, outpatient psychiatric care and home care (Berghöfer, Hubmann, Birker, Hejnal, & Fischer, 2016; Deister, 2011; Schröder & Fleßa, 2017). The providers of integration assistance and supported housing, however, are still reimbursed by the administrative district based on a fee for service principle. Because the supply of these services is not budgeted and the market is not regulated by political planning, private providers have gradually widened their share of the market throughout Germany, but particularly in the area surrounding the outreach clinic, by offering a steadily increasing supply of care (Benchmarkingkreis Eingliederungshilfe für Menschen mit Behinderung in Schleswig-Holstein, 2013; Mir, Priebe, & Mundt, 2013; Priebe et al., 2008). Therefore, a second aim of the outreach clinic was to contain the costs incurred by public authorities resulting from excessive placement in the integration assistance sector.
- Provide primary and secondary prevention for clients with psychosocial problems and at risk for mental health disorders by offering individual case support and custom-fit assignment to psychosocial care and
- Control placement into integration assistance and supported housing and the associated costs.
The subsequently reported study was performed within a multi-part pilot project consisting of (a) secondary data analyses of routine administrative data, which will be the focus of this paper, (b) a prospective cost-effectiveness study, and (c) a qualitative study on consumer and provider satisfaction. As the establishment of such a model of coordinated and co-financed psychosocial care across Social Code Books is unique in Germany, the multi-part project was initiated to evaluate the effects of the outreach clinic from different perspectives using a mixed method approach. The results can serve as the basis for further development and revision of the model.
The prospective cost-effectiveness study (b) analysed the resource utilisation of health and social services of clients referred to the outreach clinic and evaluated the change in their quality of life over the 12 months after consultation. The results indicate the high cost effectiveness of the intervention (Berghöfer et al., submitted). The qualitative study revealed that on-call telephone service, sufficient consultation time, the availability of outreach counselling and the quality of the relationship with the counsellor created high consumer satisfaction. (Schwarz, Berghöfer, Brückner, Birker, & Stöckigt, 2019; Schwarz, Stöckigt, Berghöfer, von Peter, & Brückner, online first). The model made it possible to provide more tailored assistance and strengthened stakeholders’ cooperation in the region around a common orientation for care provision (Schwarz et al., online first).
The aim of study part (a) was to analyse whether costs incurred by public authorities for integration assistance and supported housing could be lowered by offering individual counselling to the subgroup of integration assistance receivers among the clients in the outreach clinic. The second aim was to analyse the development of the number of integration assistance clients in the district compared to the development of numbers in the German population.
2 METHODS
2.1 Study design
Anonymised, aggregated data of integration assistance receivers of a rural administrative district in the federal state Schleswig-Holstein, Germany, were analysed. The integration assistance service bureau provided routinely collected anonymous individual cost data for clients of the outreach clinic and non-clients for the years 2010–2015. The outreach clinic provided the annual number of consultations for each year from its opening in 2013 through 2015. Data were retrospectively analysed for the years 2010–2015.
The primary endpoint of the study was the total yearly costs of the integration assistance service bureau of the administrative district. A secondary endpoint was the number of clients in the integration assistance scheme in relation to the number of clients who sought advice from the outreach clinic. Additionally, the number of cases and consultations in the outreach clinic between 2013 and 2015 were monitored.
Cost development was analysed by comparing those integration assistance receivers who presented in the outreach clinic to non-referral clients and matched controls. Moreover the cost progression of integration assistance receivers was compared given the number of clients and consultations in the outreach clinic to that for the total number of clients in the federal state.
Anonymised data were transferred to the Institute for Social Medicine, Epidemiology and Health Economics electronically in a password protected file.
Data were analysed according to the guidelines for secondary data analysis (Swart et al., 2005). Data processing was continuously documented, with a primary data set and a data analysis set saved separately.
2.2 Study probands
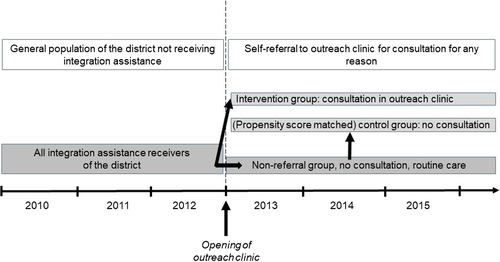
The anonymised, aggregated cost data included all clients who received services at the expense of the welfare-oriented social assistance system in the district. These clients receive follow-up wholly within the integration assistance service bureau of the administrative district. A subgroup of these clients self-referred to the outreach clinic for psychosocial counselling needs regarding medical or social issues beyond the provision of integration services (intervention group). Out of all the remaining clients without referral to the outreach clinic in the relevant period (non-referral group), a subgroup of controls was formed by propensity score matching (control group) (Figure 1).
2.3 Propensity score matching
As the outreach clinic is a voluntary offer for all residents of the specific rural area, a randomised controlled study design was not feasible. All clients self-referred to the outreach clinic. To minimise selection bias and differences at baseline between the intervention and the control group, they were matched using propensity scores. Propensity scores for the outcome ‘client of the outreach clinic’ were calculated for each client and control using age, sex and cost before the opening of the outreach clinic as covariates. The matching algorithm is based on the so called optimal matching algorithm with the goal of minimising the average absolute distance between the matched pairs. Optimal matching on the propensity scores was performed with a 1–5 ratio using the R MatchIt Package (Ho, Imai, King, & Stuart, 2011). This matching algorithm finds the matched samples with the smallest average absolute distance across all the matched pairs.
2.4 Economic analysis
- Assistance for living in institutions (cash amount), outpatient, day care or fully inpatient
- Benefits for self-determined living in sheltered housing opportunities, outpatient, day care or fully inpatient
- Assistance for work, training, employment, day structuring (accredited workplaces for disabled or mentally ill people, similar employment facilities)
- Ensuring the effectiveness of medical measures
- Helping clients to participate in community and cultural life
Mean total costs were calculated for each three-month interval from 2010 to 2012 (before the opening of the outreach clinic) and from 2013 to 2015 (after the opening of the outreach clinic). Moreover yearly costs were aggregated from the respective costs for 3-month intervals. All cost analyses were performed for the intervention group, the non-referral group and the control group.
2.5 Statistical analysis
The sociodemographic and economic data were analysed descriptively. Mean costs and 95% confidence intervals were displayed. Mean total costs were analysed between the groups for each year: first, for the intervention group and non-referral group and second, for the intervention group and propensity score-matched control group who induced costs in the respective year. The costs of the clients receiving integration assistance who did not utilise the integration assistance every year were set to zero for the years of non-utilisation. We used R Version 3.3.2 for all analyses (R Core Team, 2016).
2.6 Ethical considerations
Ethics approval for all study components was obtained from the responsible ethics committee (Ref. no.131/14, Landesärztekammer Schleswig-Holstein). Permission to use the claims data and to publish the results was obtained from the integration assistance service bureau.
3 RESULTS
Fifty receivers of integration assistance were counselled at the outreach clinic between 2013 and 2015. This number is in contrast with 678 integration assistance receivers who were not counselled at the outreach clinic. The clients at the outreach clinic were, on average, slightly younger than those in the non-referral group. Propensity score matching resulted in a subsample with 250 matched controls for the 50 clients in the intervention group. Age and the costs per person before the opening of the outreach clinic were comparable between the groups after the matching (Table 1).
| Clients receiving integration assistance | Intervention group (n = 50) | Non-referral group (n = 678) | Propensity score-matched control group (n = 250) |
|---|---|---|---|
| Female (n) | 25 (50.0%) | 271 (40.0%) | 119 (47.6%) |
| Age (years) | 34.0 (12.7) | 39.1 (14.9) | 33.6 (14.6) |
| Cost before (EUR) | 18,075 (23,446) | 30,321 (34,269) | 18,278 (26,144) |
| Propensity score | 0.08 (0.03) | 0.07 (0.03) | 0.08 (0.03) |
The distribution of costs in the total client group was left skewed because there are years where some clients did not incur any costs. When comparing only the clients with costs, the distribution is only slightly left skewed.
Over the total observation period, yearly costs were consistently lower for the outreach clinic clients than for the non-referral group. Total costs after the opening of the outreach clinic over the years 2013–2015 differed largely between the groups. Analysis of the cost data of only clients and non-referral clients who incurred costs over the years 2013–2015 revealed that 92% (n = 46) of the outreach clinic clients incurred costs. However, only 70% (n = 469) of the non-referral clients incurred costs (Table 2).
| Year |
All clients (mean costs (95% CI) EUR) |
All clients who incurred costs (mean costs (95% CI) EUR) |
|||
|---|---|---|---|---|---|
| Intervention group (n = 50) | Non-referral group (n = 678) | N intervention/ n non-referral | Intervention group | Non-referral group | |
| 2010 |
5,888 (3,342–8,434) |
10,461 (9,528–11,395) |
23/432 |
12,800 (8,783–16,816) |
16,419 (15,288–17,549) |
| 2011 |
6,119 (3,735–8,503) |
10,218 (9,282–11,155) |
24/421 |
12,748 (9,430–16,065) |
16,456 (15,299–17,613) |
| 2012 |
6,068 (3,729–8,407) |
9,642 (8,708–10,577) |
25/402 |
12,136 (8,897–15,376) |
16,262 (15,056–17,468) |
| 2013 |
5,803 (3,499–8,108) |
9,194 (8,265–10,123) |
26/371 |
11,160 (7,861–14,460) |
16,802 (15,554–18,050) |
| 2014 |
6,782 (4,148–9,416) |
9,220 (8,261–10,179) |
31/352 |
10,939 (7,395–14,483) |
17,759 (16,434–19,084) |
| 2015 |
8,930 (5,474–12,386) |
10,050 (9,057–11,044) |
35/373 |
12,757 (8,374–17,141) |
18,268 (16,959–19,577) |
|
Total (2013–2015) |
21,516 (14,513–28,518) |
28,464 (25,789–31,140) |
46/469 |
23,387 (16,014–30,759) |
41,149 (37,878–44,419) |
Propensity score matching resulted in similar cost distributions between the intervention and control groups over the entire observational period. Total costs for the years 2013–2015 were assimilated between the groups (Table 3). In the control group, the number of clients who incurred costs was unaltered at 70% (n = 177).
| Year | All clients, Propensity score matched (mean (95% CI)) | All clients who incurred costs, Propensity score matched (mean (95% CI)) | |||
|---|---|---|---|---|---|
| Intervention group (n = 50) | Control group (n = 250) | N intervention/ N control | Intervention group | Control group | |
| 2010 |
5,888 (3,342–8,434) |
5,822 (4,581–7,062) |
23/101 |
12,800 (8,783–16,816) |
14,411 (12,231–16,591) |
| 2011 |
6,119 (3,735–8,503) |
6,454 (5,195–7,712) |
24/113 |
12,748 (9,430–16,065) |
14,278 (12,286–16,271) |
| 2012 |
6,068 (3,729–8,407) |
6,002 (4,851–7,154) |
25/123 |
12,136 (8,897–15,376) |
12,200 (10,431–13,968) |
| 2013 |
5,803 (3,499–8,108) |
6,005 (4,831–7,178) |
26/114 |
11,160 (7,861–14,460) |
13,168 (11,309–15,027) |
| 2014 |
6,782 (4,148–9,416) |
6,915 (5,566–8,264) |
31/116 |
10,939 (7,395–14,483) |
14,903 (12,776–17,031) |
| 2015 |
8,930 (5,474–12,386) |
8,805 (7,357–10,252) |
35/135 |
12,757 (8,374–17,141) |
16,305 (14,381–18,229) |
|
Total (2013–2015) |
21,516 (14,513–28,518) |
21,725 (18,214–25,234) |
46/177 |
23,387 (16,014–30,759) |
30,684 (26,368–30,001) |
Clients in the intervention group had lower costs conditional on incurring any cost than clients in the non-referral group, but with a higher proportion of clients having actually incurred a cost (92% vs. 70%).
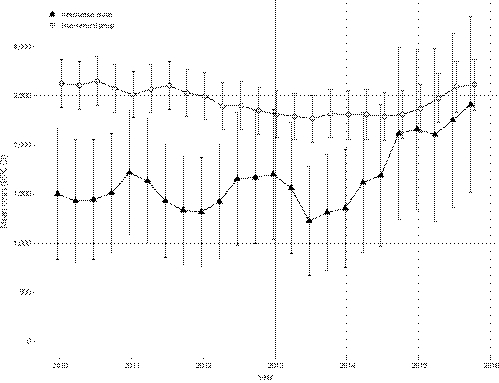
The costs of the non-referral group were relatively stable over the observational period. The costs of the intervention group were relatively steady until 2013, the opening of the outreach clinic, and began to rise from 2013 until 2015. Overall, the intervention group consistently had lower costs than the non-referral group over the observational period, although the differences diminished at the end of the observation period (Figure 2). The greatest cost difference between the groups before the opening of the outreach clinic could be observed for the year 2010 (mean difference EUR −4,573 (95% CI −6,989 to −2,159)). After the opening of the outreach clinic, 2013 denoted the greatest mean cost difference: EUR −3,390 (95% CI −5,636 to −1,145). In 2015, the last year of observation, the cost difference dropped to EUR −1,120 (95% CI −4,205 to 1,965).
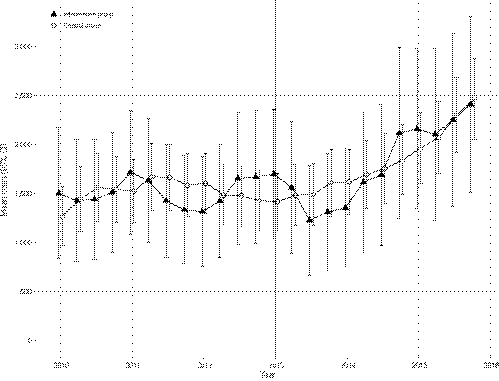
Differences between the intervention group and control group were approximately consistent over the entire observational period (Figure 3). For the year 2010, the cost difference between the groups amounted to EUR 66 (95% CI −2,563 to 2,695). In 2013, the intervention group had lower costs than the control group (mean difference EUR −201 (95% CI −2,616 to 2,214)). Cost differences between the groups for the last year of the observation accounted for EUR 125 (95% CI −3,277 to 3,527).
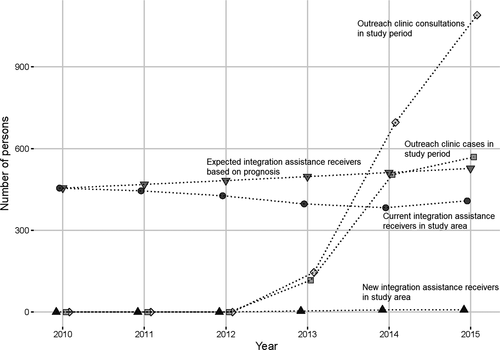
The number of consultations and cases in the outreach clinic who were referred from the general population rose steadily after the opening of the outreach clinic, from 117 clients with 146 consultations in 2013 to 569 clients with a total of 1,090 consultations in 2015. At the same time, a reduction in the overall number of integration assistance receivers in the administrative district was noted. This is in contrast with an increase in integration assistance receivers in all districts of Schleswig-Holstein and in Germany as a whole (based on data from the Federal Ministry of Labour and Social Affairs (Bundesministerium für Arbeit und Soziales, 2014)) (Figure 4).
4 DISCUSSION
The study analysed the yearly total costs of the integration assistance service bureau of an administrative district in rural northern Germany after establishing an outreach clinic for counselling clients with psychosocial problems or mental health disorders. Costs for integration assistance gradually increased during the study period. Costs for clients who were counselled did not differ from the costs incurred by propensity score-matched controls without counselling. However, the number of clients in integration assistance in the study area decreased during the study period and even dropped below the expected numbers based on developments outside the study area in the Federal State of Schleswig-Holstein.
The validity of the results is limited due to many influencing factors at the regulatory policy level. These factors are absent in the routine administrative data and thus cannot be adjusted for in the propensity score model. Among these factors are regular negotiations of a new budget for integration assistance providers in the administrative district due to rising staffing and operating costs. This partially explains an increase in costs in the integration assistance sector even without increasing numbers of clients.
A further confounding factor is a demographic change in the population of the district, with an increase in the mean age and, consecutively, in multi-morbid clients who require integration assistance services, in addition to clients with mental health and psychosocial problems. Additionally, fluctuations in employment status and other surrounding conditions, such as changes in the provision of health services and in the social environment, cannot be controlled by the selected study method.
The number of clients who utilised counselling in the outreach clinic was smaller than originally expected. In light of the high variance in cost between individuals, the analysis might not have sufficient statistical power for a valid comparison between the intervention group and the control group. Using propensity score matching, the comparability of both groups was optimised as far as possible.
The study uses routine data from the public authorities on integration assistance and supported housing for the first time in a scientific context. These data are not explicitly documented for scientific purposes but for settlement with providers. Therefore, details may be omitted if they lack administrative importance.
Based on the data source, the costing perspective is limited because of the paying authority and the short time horizon of the available data. An alternative costing perspective (e.g., a societal perspective) or time horizon may generate alternative cost differentials than those reported (e.g., productivity gains/losses, informal care givers costs, travel costs to rural community offices, etc.). This limited perspective is due to the pilot character of the study, which needs to be extended with more comprehensive data.
Due to these limitations, the study must be considered as a pilot study, and the results should encourage further research with controlled confounders and a larger study sample. At best, the results can be interpreted as indicative. However, there is no previous evaluation of a comparable model in the German health and social care system that might help to interpret findings or compare the results.
It could be speculated that clients after counselling did not return to integration assistance services and therefore did not show up again as cases in the routine administrative data. Due to the aggregated anonymised format of the data, individual cases could not be followed. Due to the methods of this study, it cannot be clarified whether these clients show up in other sectors of psychosocial or healthcare or whether their service demand is simply postponed. Positively, the decreasing number of clients could be the effect of a more custom-fit assignment of care. Consequently, the cases that remain in the integration assistance sector are the more severe cases. Less severe cases could be assigned to other forms of psychosocial care outside the integration assistance service.
In addition, the data indicate that the consultation received by the integration assistance receivers might contain extreme costs in those clients that used services.
The work of the outreach clinic is associated with a moderate and steady reduction in the number of cases in the integration assistance sector that is most likely due to the avoidance of placement of the cases with a lower need for assistance. This contrasts with the development of numbers in the surrounding administrative districts in the Federal State of Schleswig-Holstein as well as in other federal states within Germany. A shift of clients into the integration assistance services of the surrounding administrative districts can be excluded because the competences of authorities are strictly regionally organised.
Clients who receive integration assistance but no counselling in the outreach clinic until the end of the study period might be stable long-term receivers of care, with numbers ranging from 432 to 352 per year. While the total numbers per year are decreasing, the costs for this group are steadily increasing. This might be a net effect of rising staffing and operating costs on the providers’ side.
The decreasing numbers of clients in the integration assistance sector are associated with the increased counselling activity of the outreach clinic. This could be interpreted as a preventive effect of the outreach clinic that is thwarting the efforts of private providers to further widen their share of the market and secure profitable funding for an increased supply of institutionalised and outpatient receivers of care. However, a major confounder cannot be ruled out: the positive effect of steady efforts by the district to create a capped budget for providers.
The development of cases and contacts in the outreach clinic shows a slight stagnation towards the end of the study period. This effect could be due to saturation in the administrative district as the comprehensive coverage of clients in need of counselling is reached. In contrast, further publicity in the district might be needed. In addition, it could be prospectively reasonable to assign regular and long-term clients to counselling in the outreach clinic. This might potentially induce a revision of their model of care and remove them from institutionalised integration assistance. However, this is not the primary aim of the outreach clinic, which does not work in competition with regular consultations in the integration assistance system (the so-called ‘help plan review’). The primary aim of the outreach clinic is the early detection of psychosocial help-seeking behaviour achieved by working at the front end or pre-field of the professional system.
The results from other areas of the project support the potential of the outreach clinic. In the prospective cohort study, the cost effectiveness of the outreach clinic counselling was shown (Berghöfer et al., submitted), and the qualitative study depicted the high satisfaction of clients with the counselling offer (Schwarz, Berghöfer, Brückner, Birker, & Stöckigt, 2018) and of professionals working in the network (Schwarz et al., online first). However, the methodology of this study and of the project as a whole is pragmatically oriented towards the reality of care. The various effects of the outreach clinic on health, quality of life, care costs and effectiveness need to be examined in more detail in further studies and other regions.
The finding that fewer integration assistance receivers visited the outreach clinic during the study period cannot be interpreted with certainty. The workforce was sufficiently strong and was also heavily used by persons from the general population (see Figure 4). It seems to be more of an organisational problem that clients were not sent consistently enough to the outreach clinic. Ultimately, this is still a pilot project, that is, integration assistance receivers cannot be obliged to attend the outreach clinic. The potential of scaling is more likely to be that new integration cases can be prevented than that existing integration cases can be redirected.
The outreach clinic currently only integrates the healthcare and integration assistance sector on a population level in a circumscribed geographical region. Future development of the model could also include the rehabilitation and long-term care sector and engage the regional Association of Statutory Health Insurance Physicians as a third stakeholder of the outreach clinic. Thus, cross-sectoral navigation of clients would also include the outpatient primary care sector.
The concept of integrating healthcare and social care in the counselling service of the outreach clinic is relatively unique in the German healthcare system. Another regional model that included health and social care failed due to administrative and regulatory barriers and could not be evaluated (Peters, 2018). While the promotion of cross-sectoral care within the healthcare system in Germany has strongly increased in recent years and has political backing, overcoming the division of sectors caused by the various Social Code Books has not yet been the focus of policy. The actors engaged in self-administration in the German healthcare system find it difficult to take action; innovations are mainly driven by regional individual actors.
5 CONCLUSIONS
The innovative outreach clinic model might have the potential to efficiently provide individually required support measures across the relevant social insurance codes for people with psychosocial needs regionally and on a population-related basis. In a non-regulated market of integration assistance providers, the results of this pilot study indicate that the model might help to control the excessive placement of clients with little need for integration assistance and instead save resources for those more severe cases who truly need these services. Subject to confirmation of the effects in other regions and with larger case numbers, the model might in the long run stabilise expenditures in the social insurance code of individual case support below the expected nationwide trend.
ACKNOWLEDGEMENTS
This multi-part project was funded by the Ministry of Social Affairs, Health, Youth, Family and Senior Citizens of the federal state Schleswig-Holstein (Az. 234 - 455.5.004-005/02). We are grateful to Holger Banasch, administrative district of Dithmarschen, for his support in the data management. The manuscript was edited for proper English language by American Journal Experts.