‘Nobody Has Ever Spoken to Me About PCD and Fertility Issues’: Fertility Experiences of People With Primary Ciliary Dyskinesia and Their Family Caregivers
ABSTRACT
Background
Primary ciliary dyskinesia (PCD) affects fertility in both females and males. To understand the impact and concerns among people with PCD and parents of affected children (family caregivers), we explored how they report their experiences with fertility.
Methods
We used qualitative data from a questionnaire on fertility from Living with PCD, an international participatory study. In optional open-ended comment fields, participants shared their thoughts and experiences related to fertility. We adopted conventional content analysis and analysed the data inductively.
Results
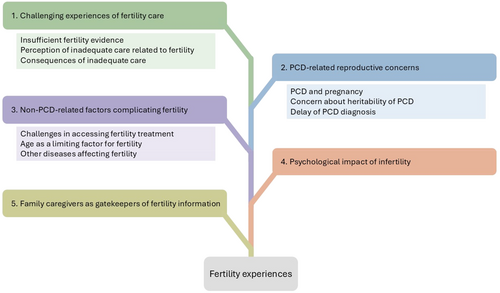
Out of 384 survey respondents, 206 (54%) provided free-text comments that we included in this analysis. We identified five categories illustrating participants' experiences with fertility: (1) challenging experiences of fertility care, ranging from insufficient fertility evidence to poor care from treating physicians, leading to an overall perception of inadequate care related to fertility; (2) PCD-related reproductive concerns, such as pregnancy risks, heritability of PCD and delayed PCD diagnosis; (3) non-PCD-related factors complicating fertility, such as challenges in accessing fertility treatment, age as a limiting factor for fertility and other diseases affecting fertility; (4) psychological impact of infertility, marked by emotional distress, grief and coping strategies; and (5) family caregivers as gatekeepers of fertility information, reflecting their role in managing, delaying, or shaping how and when children learn about fertility.
Conclusion
We need enhanced support and standardised reproductive counselling and healthcare for people with PCD to enable informed decisions on fertility and to reduce the fertility-related concerns and psychological impact faced by many.
Patient or Public Contribution
This participatory study was co-designed with people with PCD and a patient advisory group. Patients actively shaped research priorities, contributed to study design and questionnaire development, and played a key role in data interpretation and dissemination.
1 Introduction
Understanding the fertility experiences of people with primary ciliary dyskinesia (PCD) and parents of affected children (family caregivers) is important, given the high risk of infertility associated with the condition. PCD is a rare genetic multi-organ disease that impairs the structure and function of motile cilia throughout the body. This ciliary dysfunction mainly leads to chronic upper and lower airway symptoms such as recurrent infections, bronchiectasis and hearing impairment, significantly impacting the quality of life of those affected [1]. Beyond its respiratory manifestations, infertility affects up to 80% of males and 60% of females with PCD [2]. Male infertility is the result of dysmotile sperm and sperm agglutination due to defective cilia in the testes [3]. Female infertility, although less well understood, is thought to result from ciliary dysfunction in the fallopian tubes and uterus [4-6]. Females with PCD also have an increased risk of ectopic pregnancies [2], likely due to impaired oocyte transport. Recent research highlights a significant need for fertility treatments among both males and females to achieve successful conception [2]. Despite this, referral to fertility specialists is not routinely integrated into PCD care, and people with PCD are often dissatisfied with the fertility information provided by their healthcare providers [7].
To date, there is a significant gap in studies exploring the lived experiences of individuals with PCD and their family caregivers in relation to fertility. Evidence from studies on other conditions associated with infertility suggests that the inability to conceive is often an unexpected and distressing experience and often a personal tragedy [8, 9]. Alongside these psychological challenges, illness-related challenges often influence reproductive decisions. Females with chronic lung conditions often receive conflicting advice regarding the impact of their condition on pregnancy and how pregnancy might affect their health [10]. Lastly, fertility treatments are known to be physically, emotionally and socially difficult [8, 11].
To understand the concerns and impact of fertility problems on people with PCD, we explored how they and their family caregivers report their experiences with fertility. This understanding is essential to identify and address the needs of people living with PCD and is crucial for developing patient-centred resources, support systems, fertility care guidelines and healthcare services.
2 Methods
2.1 Study Design and Procedure
We analysed free-text data from a questionnaire on fertility and fertility care, which we conducted as part of the Living with PCD study (previously named COVID-PCD), an international participatory study involving over 750 participants from 49 countries. Our research team at the University of Bern, Switzerland, launched Living with PCD during the coronavirus disease 2019 (Covid-19) pandemic to monitor the impact of Covid-19 on people with PCD. Following the pandemic, we shifted the study's focus to address broader questions raised by individuals with PCD. Both study participants and people with PCD outside the study [12] identified the topic of fertility as a research priority. We lead the Living with PCD study in close collaboration with a study advisory group consisting of members of PCD patient associations worldwide. We have published a detailed study protocol [13].
Living with PCD is an anonymous study open to individuals worldwide who have a confirmed or suspected PCD diagnosis. Participants include adults, adolescents and family caregivers of children with PCD who complete questionnaires on behalf of their children. Patient associations invited their members to participate by sharing the invitation link via email and on social media. Participants self-registered on the study website, after which they received a questionnaire covering demographic information and details about their PCD diagnosis and symptoms, followed by shorter weekly follow-up questionnaires and occasional questionnaires on special topics. We sent a special questionnaire on fertility and fertility care to all study participants on 12 July 2022 and to all participants who joined later by 8 March 2023. We sent up to three reminders via email to non-responders. Participants entered data directly into an online database using the Research Electronic Data Capture (REDCap) platform [14], hosted by the Swiss medical registries and data linkage centre at the University of Bern, Switzerland. Participants gave informed consent at enrolment and could leave the study at any time by contacting the study team. The ethics committee of the canton of Bern, Switzerland, approved the study (study ID: 2020-00830).
2.2 Data Collection/Questionnaire
We developed the fertility questionnaire together with fertility specialists, reproductive endocrinologists and members of the study advisory group. The questionnaire contained mainly closed questions with five open-ended questions, of which the last question invited participants to ‘Please write any additional comments you may have about fertility in people with PCD or comments to this questionnaire.’ The analysis of these additional comments forms the focus of this manuscript. We developed the questionnaire in English, and native-speaking members of the study team translated the questionnaire into French, German, Italian and Spanish; two members of the study team or advisory group checked the translations. We used DeepL to translate responses of participants in languages other than English and asked a native speaking member of the research group to review and verify these translations. We edited the participants' quotes for language and clarity [15] and included information on participants' age, sex and fertility. To ensure the anonymity of our participants, we report their age in age groups: 0–5 years, 6–12 years, 13–17 years, 18–29 years, 30–39 years, 40–49 years and ≥ 50 years. We only selected one quote per individual to ensure diverse representations. We present the results of other parts of the survey elsewhere [2, 7].
2.3 Analysis
We employed conventional content analysis [16]. This approach is specifically suitable when ‘existing theory or research literature on a phenomenon is limited’ [16], allowing for researcher immersion with data at hand. We coded data mainly inductively, aiming at capturing and reflecting participants' experiences related to fertility. However, at a later stage, deductive codes relating to care provision and diagnostics helped to organise the findings.
The first author (L.D.S.) undertook the main analyses with support from S.M. and was supervised by M.G. L.D.S. is a medical doctor and a PhD student in epidemiology with basic training in qualitative research. Her research is mainly focused on PCD with a particular emphasis on fertility, using mainly quantitative methods. S.M. is a PhD student in public health with a background in social sciences and with in-depth training and experience in undertaking qualitative research. She had little prior knowledge of the topics of PCD and fertility. M.G. is a senior researcher and medical doctor with a PhD in epidemiology, with extensive experience in qualitative methods, and a PCD expert leading international PCD research collaborations [17].
L.D.S. read the free text responses several times to gain a general understanding of the information and achieve immersion. By reading every response word by word, she identified initial codes related to participants' experiences and sorted them into categories, creating an initial coding scheme. S.M. independently read a selection of open-ended questions, coded them and discussed impressions of participants' experiences with L.D.S. In an iterative process, L.D.S. and S.M. reviewed, compared and refined the categories by grouping overlapping or similar codes together. If they could not agree on the categories, they went back through the participants' responses to make sure they had captured what participants expressed and stayed close to the data. They discussed differences in coding and reassessed to reach consensus. The last author, M.G., read a random selection of open-ended responses and participated in several meetings to critically reflect upon the analysis procedure and interpretation of findings. We used NVivo 1.7.1 to facilitate data management during analysis.
3 Results
Overall, 266 adults, 16 adolescents and 102 parents or family caregivers of children with PCD completed the fertility questionnaire. Among them, 206 (122 females, 46 males, 4 adolescents and 34 parents) left a comment and were included in this analysis. The adults had a median age of 42 years. Most participants were from the United Kingdom (41; 20%), the United States (33; 16%) or Germany (31; 15%). Two hundred (97%) reported having a PCD diagnosis confirmed by a physician, and six (3%) had a suspected diagnosis. Among 121 adult participants who had already tried to conceive, 38 (31%) had naturally conceived children, 49 (40%) had conceived children with the use of fertility treatments and 34 (28%) had not been able to conceive a child with or without the use of fertility treatments.
We identified five categories illustrating the experiences with fertility of people with PCD and their family caregivers: (1) challenging experiences of fertility care, (2) PCD-related reproductive concerns, (3) non-PCD-related factors complicating fertility, (4) psychological impact of infertility and (5) family caregivers as gatekeepers of fertility information. Of note, the categories are not to be understood as separate topics as they are interlinked in many instances (Figure 1).
3.1 Challenging Experiences of Fertility Care
Participants reported different challenging experiences, ranging from insufficient fertility evidence to poor care from their respective doctors, leading to an overall perception of inadequate care related to fertility. The consequences of inadequate care were manifold: The perception of inadequate care led to the feeling that trying to conceive naturally was a ‘waste of time’ rather than starting fertility treatment early. The challenging experiences motivated some participants in self-advocacy efforts to organise, research, reach out to each other and exchange experiences. Still, some participants reported having had good experiences and good care, albeit in a minority of cases.
Insufficient Fertility Evidence
‘However, without looking for it, I unexpectedly became pregnant at the age of 36. My pulmonologist at the time called me “miraculous” and concluded that, fortunately, medicine does not explain everything’.
P181, female, ≥ 50 years, with one child
‘Isn't it psychologically tricky not to know if you are fertile? Also, if you think you might not be, as a teenager, you might become more careless about protection?’
P167, parent of a child, 0–5 years
In several cases, participants hypothesised that fertility was not a priority in PCD care and research. Indeed, they felt that there is ‘not a huge amount of urgency for better understanding these issues in the medical community’. Adding to this, participants postulated that information was particularly lacking for females, leaving them with many open questions.
Perception of Inadequate Care Related to Fertility
‘I have always been amazed that nobody has ever spoken to me about PCD and fertility issues, despite being diagnosed in my early 20s by a leading PCD hospital and being treated by them ever since. I am now beyond the age of having children, but I would hope this is something that will be improved in the future for younger generations.’
P44, female, ≥ 50 years, has never tried to become pregnant
In some instances, participants even considered the information received as wrong: for instance, that ‘a PCD patient is by definition infertile’ or ‘people with PCD are […] sterile’. Participants also pointed out that fertility experts lacked knowledge about PCD, which prevented them from effectively addressing their specific information needs.
Further, participants perceived the way fertility information was disclosed as challenging due to physicians' lack of empathy. They reported that both PCD physicians and fertility specialists often provided this information in an offhanded manner, without sufficient explanation or context.
‘The first fertility doctor I saw refused to accept that [PCD] could be impacting on my fertility and wouldn't accept me for in vitro fertilization (IVF) treatment […]’.
P31, female, ≥ 50 years, with one child conceived via fertility treatment
Thus, participants underlined the need for fertility education and counselling for health professionals on PCD.
Consequences of Inadequate Care
‘I was actually very frustrated in the end that the doctors didn't give me any information at all, otherwise I would have tried to have a child much sooner.’
P165, female, ≥ 50 years, with one child conceived via fertility treatment
‘I had the usual treatment from a professor of pneumology, an ENT specialist, a gynaecologist, and a [general practitioner]. None of these health professionals alerted me to the possibility of having difficulty conceiving a child naturally. I therefore took the personal step of calling a [fertility] centre but with a certain fear of not being legitimate, given that PCD is little known by health professionals.’
P190, female, 30–39 years, pregnant at the time of the survey
3.2 PCD-Related Reproductive Concerns
In addition to the effects of PCD on fertility, participants shared other reproductive concerns arising from having PCD, such as PCD and pregnancy, particularly the impact of PCD on a potential pregnancy or on their ability to care for children, as well as concern about the heritability of PCD. Some participants were not even aware they had PCD when they were pregnant or faced fertility problems, and this delay of a PCD diagnosis hindered optimal care.
PCD and Pregnancy
‘I ultimately decided I was already too sick to care for children and to not try, which was/is heartbreaking.’
P164, female, 30–39 years, has never tried to become pregnant
‘The whole pregnancy and birthing process affected my lungs and respiratory wellbeing in a negative way very considerably, […] and it would have been a much better experience and treatment outcome for me if there had been a combined treatment approach from respiratory and fertility/obstetric specialists.’
P110, female, ≥ 50 years, with two children
‘Oddly enough, while I was pregnant I was at my healthiest. My lungs and infections were the best they have ever been.’
P112, female, 40–49 years, with two children
‘I find it much easier to clear mucus when pregnant—if only my lungs could stay that way all the time!’
P41, female, 40–49 years, with two children
Concern About Heritability of PCD
‘[…] the idea that I, as a person with a genetic disease, could pass on the corresponding genes to my offspring is a weighty point for me in my (at least current) attitude of not wanting to have children.’
P94, male, 30–39 years, has never tried to father a child
Delay of PCD Diagnosis
‘Infertility (no sperm at all in the spermiogram) was clarified twice, as the attending doctor assumed a test error. The diagnosis of PCD was also suspected a few months later due to the infertility by a general practitioner who referred me for clarification.’
P1, male, ≥ 50 years, never fathered a child
3.3 Non-PCD-Related Factors Complicating Fertility
Apart from these PCD-specific factors, participants mentioned other fertility challenges complicating their fertility journey. Among these, challenges in accessing fertility treatment, age as a limiting factor for fertility and other diseases affecting fertility constituted the main themes.
Challenges in Accessing Fertility Treatment
‘Although I had two babies with the help of IVF, it doesn't tell the whole fertility treatment story. In total, I went through three different rounds of fertility treatments with IVF. In all three rounds combined, I had five chromosomally normal embryos, which we attempted to transfer. Two never took, one was an early miscarriage, and two were my precious babies who are now 3 years old and 3 months old. Prior to IVF, we also tried timed intercourse with the help of ovarian stimulation, as well as intrauterine insemination over the span of a year. And, of course, there were the 2 years spent trying on our own to get pregnant before we consulted with fertility doctors.’
P113, female, 40–49 years, with two children conceived via fertility treatment
‘There is a life without children, and I don't like this whole fertilisation technology.’
P101, female, ≥ 50 years, has never been pregnant
Age as a Limiting Factor for Fertility
‘I'm on the waiting list for IVF, which might take up to 2 years' time, so I regret I didn't start the process earlier because I'll turn 36 by then.’
P17, female, 30–39 years, has never been pregnant
Other Diseases Affecting Fertility
‘My partner does not have PCD but does also have some fertility challenges […] and this was relevant to our journey.’
P21, male, 30–39 years, has never fathered a child
3.4 Psychological Impact of Infertility
‘Fertility has been a much bigger issue for me with PCD than any lung problems, although I have a significant wet cough daily.’
P170, female, 30–39 years, with two children
‘I am now 49 years old and have given up of course. It just wasn't in my stars to become a mother.’
P146, female, 40–49 years, has never been pregnant
‘I will never have a family. Such heartache. I hope things improve for people with PCD.’
P158, female, 40–49 years, has never been pregnant
‘[…] we were blessed with the opportunity of adopting a 10-day-old baby. She is now 30 years old. We were both happy with this decision and did not have the need to continue with fertility treatments.’
P171, female, ≥ 50 years, has never been pregnant
3.5 Family Caregivers as Gatekeepers of Fertility Information
Family caregivers of children with PCD not only felt responsible for their child's current health but were also concerned about possible future health problems, of which they believed fertility was an important aspect.
Many family caregivers stated that they were aware of possible fertility problems, and most felt it was important that they were informed at diagnosis that their child might have fertility problems. However, family caregivers assessed their own need for information and that of their children differently, as many did not see the need to inform their children about fertility at an early age. By doing so, they acted as gatekeepers for fertility information. Several family caregivers of children with PCD wanted to be the ones to inform their children before the physicians did and reinforced their responsibility to determine the right time to educate their child about possible fertility problems.
‘As a parent of children with PCD, I think that if they are going to have issues with fertility, they should know earlier in life. It's part of planning their futures. They should keep in mind the goals and the obstacles they will need to overcome.’
P80, parent of a child, 6–12 years
Others only wanted to inform their children when they were ‘adolescents/young adults’, ‘during puberty or later when she grows up or becomes pregnant’ or ‘when the time comes that he wants children’.
‘I'm a mother of a teenager with PCD, and I completed that particular survey on behalf of my son. Every survey in the past was completed by him in person. This one I did by myself because we have not talked to our child about fertility yet. His doctor says we should not worry until we have results of sperm tests and for now, he is too young for it. So we wait. But I think that [the] fertility topic is very important and every patient should be fully informed.’
P64, parent of an adolescent, 13–17 years
‘[…] knowing that at the right and appropriate time, they can have access to and be provided with specialist counselling and help is the key. They are not alone to find out the information by themselves.’
P24, parent of a child, 6–12 years
Many described the importance of gradual, age-appropriate information, with fertility counselling only being offered to adults.
4 Discussion
People with PCD reported challenging experiences related to their fertility. They faced uncertainty and disjointed care when making family planning decisions and were often left to navigate their fertility journey on their own with little support from healthcare professionals. Reproductive concerns among females about the impact of a potential pregnancy on their lung health and the fear of passing on PCD unsettled them in their decision to have children. Additionally, challenges in accessing fertility treatment, the time-critical nature of fertility and the long delays to receive a PCD diagnosis complicated their fertility journey. Infertility was described as a significant psychological burden, which was also recognised by family caregivers of young children.
Our study shows that people with PCD often have challenging experiences with fertility care. Many are not treated in PCD centres but by physicians with little experience with the disease, a difficulty shared with people living with other chronic diseases. People with multiple sclerosis or chronic lung diseases such as asthma also report a lack of discussions, information and education and little knowledge from healthcare professionals about fertility [10, 18]. Even individuals with cystic fibrosis (CF), for whom the effects on fertility are known and therefore organised care could be expected, are not satisfied with their fertility care and wish for earlier and improved fertility education [19, 20]. Among men with CF, infertility has been associated with significant psychological distress, adverse effects on mental health and unmet support needs, highlighting the critical importance of integrating reproductive and psychosocial care within chronic disease management [21]. Similar to what we observed, studies in CF that examined provider attitudes have highlighted structural limitations in care, where pulmonologists often act as the main providers but may lack the training or systems to adequately address reproductive health needs—leading to a disconnect between respiratory and fertility services and unmet patient expectations [22-24].
Women with CF also share concerns about the impact of their chronic condition on reproduction, as was the case with our participants. CF influences them in their pregnancy and parenting decisions as they feel they may not be well enough to support a family or conceive children [25]; similar considerations have been shared by women with asthma or sarcoidosis [10]. While people living with chronic diseases often become experts in managing their condition, they rely heavily on physicians and the health system for fertility issues if they need treatment. We have found that inequities in accessing fertility care further complicate the fertility journey. Additionally, for many individuals, advanced fertility treatments like IVF are not affordable because of their healthcare system [26].
Our findings show that the combination of these diverse challenges can lead to detrimental consequences for people living with PCD who face fertility issues, particularly in terms of psychological well-being and related concerns. Research with childhood cancer survivors has shown that the psychological dimension is often overlooked in discussions about infertility. Newton et al. pointed out that survivors of childhood cancer often feel the ongoing psychological distress that results from living with uncertain fertility, which contributes to anxiety and a sense of uncertainty about their own future [27]. The unpredictability of their illness worsens this burden.
Our findings also show that family caregivers are aware of potential fertility issues but often become gatekeepers of this information about their child's fertility and future reproductive health, at times deliberating about the best timing to deliver this information. Family caregivers of children with PCD had previously expressed fertility concerns about their child's future, worrying about the impact of fertility treatments and whether PCD could be passed on to grandchildren [28]. However, by acting as a gatekeeper, parents themselves may limit children's ability to receive optimal care. Shifting responsibility to adult care may carry the risk of important knowledge being lost as care for adults is less well organised than paediatric care in PCD in many countries [29]. These results point to the need for appropriate guidance for parents of children with PCD on how to best hold these discussions with their children, as well as about the appropriate timing to raise the topic.
We also found that people with PCD have a high need for information and support in relation to their fertility. This need is particularly pronounced among those who are not treated in specialised PCD centres and instead rely on physicians with limited experience in treating the disease. They wish for clearer information from healthcare professionals, more information about the impact of the disease on fertility and better integration of fertility and respiratory services. To improve their care, we need to improve the existing evidence base on fertility and create disease-specific guidelines to provide them with accurate information and counselling on their fertility journey. One participant mentioned that leaflets on PCD and fertility would be useful to share with general practitioners and other health professionals. Others mentioned that sharing studies, statistics and fertility solutions for people with PCD within the community would be very useful and appreciated. People with PCD would benefit if the psychological aspect of fertility were better integrated into their care. Information about fertility needs to be communicated honestly, sensibly and in a timely manner, with concerns recognised and support offered. By being aware of the risk of psychological effects of fertility and infertility problems, healthcare professionals can also identify those who need support and offer them professional counselling, for example, by a psychologist or social worker. Above all, accurate and timely PCD diagnosis is important to ensure that those affected receive appropriate care and fertility information.
This is the first study to explore the experiences of people with PCD regarding fertility. The large sample size and international scope of our study allowed us to capture insights from a diverse group of participants worldwide. The open-ended comment box in our questionnaire enabled participants to share a wide range of experiences, which resulted in a rich and varied collection of perspectives from individuals with PCD and their family caregivers. Additionally, the anonymity of the survey may have led them to share their experiences more openly.
The use of questionnaires as our data collection method limited the depth of information we could obtain, as this approach did not allow us to ask probing or follow-up questions, as would be possible in an interview. Another key limitation of this study is the lack of purposeful sampling, as participants were self-selected and completed the questionnaires based on their own interests. It is likely that individuals with fertility issues were more inclined to participate, and those with negative experiences may have been particularly motivated to share their experiences. It is also important to note that the experiences shared cover a long period of time during which significant advances in knowledge and care have been made. Participants' reflections may, therefore, reflect historical gaps that have been partially addressed in recent years. Additionally, our study primarily reflects the experiences of people with PCD who are in contact with PCD support groups, predominantly from high-income countries in Europe and North America, where PCD diagnosis and care are also more established. Unfortunately, our study does not include individuals from minority groups where cultural identity is often closely tied to motherhood [30], and we could not capture socio-cultural aspects related to infertility. Infertility can carry a significant stigma, and societal norms, cultural expectations and personal experiences strongly influence the path to parenthood.
We need enhanced support and standardised reproductive healthcare for people with PCD and their family caregivers to enable informed decisions on fertility, as well as to reduce the fertility-related concerns and psychological impact faced by many of them.
Living With PCD Patient Advisory Group (in Alphabetical Order)
Bernhard Rindlisbacher, Selbsthilfegruppe Primäre Ciliäre Dyskinesie, Switzerland; Catherine Kruljac, PCD Australia, Australia; Emilie Wattellier, Association ADCP, France; Fiona Copeland, PCD Support UK, the United Kingdom; Hansruedi Silberschmidt, Verein Kartagener Syndrom und Primäre Ciliäre Dyskinesie, Germany; Isabelle Cizeau, Association ADCP, France; Katie Dexter, PCD Support UK, the United Kingdom; Lucy Dixon, PCD Support UK, the United Kingdom; Michele Manion, PCD Foundation, the United States; Sara Bellu, Associazione italiana Discinesia Ciliare Primaria Sindrome di Kartagener A.P.S., Italy; Susanne Grieder, Selbsthilfegruppe Primäre Ciliäre Dyskinesie, Switzerland; Trini López Fernández, Asociación Española de Discinesia Ciliar Primaria/Síndrome de Kartagener, Spain.
Author Contributions
Leonie D. Schreck: conceptualisation, methodology, data curation, formal analysis, visualisation, writing – original draft, writing – review and editing, project administration, investigation. Sophie Meyer: methodology, writing – original draft, writing – review and editing, formal analysis, validation. Eva S. L. Pedersen: conceptualisation, writing – review and editing, project administration, supervision, funding acquisition. Yin Ting Lam: writing – review and editing, software. Hansruedi Silberschmidt: writing – review and editing, data curation, conceptualisation. Sara Bellu: conceptualisation, data curation, writing – review and editing. Hansruedi Silberschmidt: writing – review and editing, data curation, conceptualisation. Sofía C. Zambrano: writing – review and editing, supervision, methodology. Claudia E. Kuehni: conceptualisation, writing – review and editing, supervision, funding acquisition, resources. Myrofora Goutaki: conceptualisation, methodology, supervision, funding acquisition, investigation, writing – review and editing, formal analysis, validation.
Acknowledgements
We thank all participants and their families, and we thank the PCD support groups and physicians who advertised the study. We would like to particularly thank Bernhard Rindlisbacher, whose death in March 2025 saddened us all deeply. Bernhard has been a member of the Living with PCD advisory group since its start, and it was his initiative that gave birth to the study, opening a new area in PCD research, which is truly participatory and unites efforts of people living with PCD, researchers and clinicians to find out more about PCD and change the world to a better one. We thank our collaborators who helped set up the Living with PCD study: Cristina Ardura, Christina Mallet, Helena Koppe and Dominique Rubi from the University of Bern and Jane S. Lucas and Amanda Harris from the University Hospital Southampton. We thank Sophie Christin-Maitre (Sorbonne University), Bernard Maitre (Université Paris-Est Créteil), Nathalie Massin (American Hospital of Paris), and Lara Gonçalves Pissini (University of Bern) for their help in the design of the fertility questionnaire. Our research was funded by the Swiss National Science Foundation, Switzerland (SNSF 192804 and SNSF 10001934) and the Swiss Lung Association, Switzerland (2021-08_Pedersen), and we also received support from the PCD Foundation, the United States; the Verein Kartagener Syndrom und Primäre Ciliäre Dyskinesie, Germany; the PCD Support UK; and PCD Australia, Australia. L.D.S., E.S.L.P., Y.T.L., C.E.K., and M.G. participate in the BEAT-PCD Clinical Research Collaboration supported by the European Respiratory Society.
Disclosure
During the preparation of this study, the author(s) used ChatGPT 4o, DeepL and Grammarly to improve the readability and clarity of the manuscript. After using these tools/services, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
Ethics Statement
Bern Cantonal Ethics Committee (Kantonale Ethikkommission Bern) approved our study (Study ID: 2020-00830).
Consent
Participants provide their informed consent to participate in the study at registration. Participation is anonymous. Participants can withdraw consent to participate at any time by contacting the study team.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Living with PCD data is available upon reasonable request from Claudia Kuehni ([email protected]).




