An application of the Biobehavioral Family Model: Examining the impact of maternal depression on child asthma mediated by insecure attachment and child depression
Abstract
enObjective
Child asthma disparities are prevalent in socio-economically stressed single-parent families. Stress impacts childhood asthma mediated by immune and autonomic pathways, but specific family stress pathways are not well established. This study tests the hypothesis, derived from a version of the Biobehavioral Family Model, that single parent maternal depression impacts child asthma mediated by insecure attachment and child depression.
Methods
In a cross-sectional study, children with asthma (age 7–17 years old) from a socio-economically disadvantaged population and their single parent mothers (N = 202) were assessed for depression and attachment security. Child asthma disease activity was assessed by symptom report and lung function tests. Structural equation modeling (SEM) was used to test a model in which caregiver depression impacts child asthma disease activity mediated by insecure attachment and child depression.
Results
SEM results indicated that maternal depression statistically predicted child depression (β = 0.21, p < 0.01) and insecure mother–child attachment (β = 0.17, p < 0.05). In addition, insecure attachment statistically predicted child depression (β = 0.50, p < 0.001). Child depression mediated the adverse effects of maternal depression and insecure attachment on child asthma disease activity (β = 0.43, p < 0.01). There was no direct effect of insecure attachment on child asthma.
Conclusion
In single-parent families, maternal depression may impact child asthma disease activity, mediated serially by insecure attachment and child depression. Longitudinal and/or intervention studies are needed to establish a causal effect. These findings suggest that caregiver depression and parent–child relationships may be important targets for family intervention. These interventions may help improve child asthma outcomes and reduce health disparities.
摘要
zh目标
在社会经济压力大的单亲家庭中, 儿童哮喘的差异性很普遍。压力对儿童哮喘的影响是由免疫和自律神经途径带来的的, 但具体的家庭压力途径还没有很好地研究清楚。本研究测试了从生物行为家庭模型的一个版本中得出的假设, 即单亲母亲的抑郁症对儿童哮喘的影响是由不安全的依恋和儿童抑郁症引发的。
研究方法
在一项横断面研究中, 针对来自社会经济弱势人群的哮喘儿童 (7-17岁) 及其他们的单亲母亲 (N=202) 作抑郁症和依恋安全方面的评估。儿童哮喘疾病活动是通过症状报告和肺功能测试来评估的。结构方程模型 (SEM) 被用来测试一个模型, 在这个模型中, 照料者的抑郁表现影响儿童哮喘病的活动, 并由不安全的依恋和儿童的抑郁影响。
研究结果
SEM结果显示, 母亲抑郁症在统计学上预测了儿童抑郁症 (Β=0.21, p<0.01) 和不安全的母子依恋 (Β=0.17, p<0.05) 。此外, 不安全的依恋在统计上预测了儿童患抑郁的可能性 (Β = .50, p < .001) 。儿童抑郁症引发了母亲抑郁症和不安全依恋对儿童哮喘疾病活动的不利影响 (Β = .43, p < .01) 。不安全的依恋对儿童哮喘并没有直接影响。
结论
在单亲家庭中, 母亲的抑郁症可能会影响儿童哮喘病的活动, 依次引发不安全的依恋和孩子的抑郁症。需要进行纵向和/或干预研究以确定因果效应。这些发现表明, 照顾者的抑郁和亲子关系可能是家庭干预的重要目标。这些干预措施可能有助于改善儿童哮喘症状的结果, 并减少在健康方面的差异。
INTRODUCTION
Stress and childhood asthma
The impact of stress on childhood asthma is now well-established, and psychobiologic pathways underlying these effects are beginning to be elucidated. A meta-analytic study of 30 years of research has established that stress impacts the immune system in ways that can potentiate disease (Segerstrom & Miller, 2004). More specifically, there is robust evidence that stress impacts childhood asthma (Schreier et al., 2011), mediated by hypothalamic–pituitary adrenal and immune pathways (Chen & Miller, 2007). In particular, strained parent–child relations bring about adverse outcomes in asthma by diminishing cortisol's ability to regulate cytokine activity and subsequent airway inflammation (Marin et al., 2009). Furthermore, child depression is associated with the presence of childhood asthma and with worse asthma symptoms (Booster et al., 2016; Katon et al., 2007; McQuaid et al., 2001; Waxmonsky et al., 2006), and dysregulation in autonomic pathways and mechanisms have also been identified as a mediator of the effects of stress and depression on child asthma (Lehrer, 1998; Miller et al., 2009; Ritz et al., 2010). Specifically, Miller's Autonomic Nervous System (ANS) Dysregulation Model proposes (Miller, 1987; Miller & Wood, 2003), and laboratory-based studies support, that child depressive emotional states are accompanied by a specific pattern of ANS dysregulation (cholinergic/vagal bias), which potentiates airway constriction and worsens child asthma (Hsu et al., 2020; Miller et al., 2009). Vagal bias is a predominance of vagal over sympathetic reactivity to a stressful stimulus. Because airway constriction is partially mediated by vagal/cholinergic neural mechanisms, a relatively higher level of vagal versus sympathetic reactivity (i.e., vagal bias) is proposed to potentiate the effect of irritants, allergens, infections, and emotional distress on airway constriction in asthma.
The biobehavioral family model applied to childhood asthma
Despite advances in knowledge of physiologic mechanisms by which stress impacts child asthma, identification of specific stressors, and how they operate, has been limited by the lack of organizing multilevel-systemic models. The Biobehavioral Family Model (BBFM) has proved useful in this regard (Wood, 2018; Wood et al., 2000). The BBFM is a heuristic model which prioritizes family factors, based on the evolutionary observation that the family social system serves as protection from, and as a means of adapting to, social stress and adversity. If the family process is functional, the family will buffer family members from stress, but if the family process is dysfunctional, stress and maybe exacerbated resulting in anxiety and depression, and consequent physical illness. The BBFM identifies specific pathways by which family relational process impacts emotional/psychological as well as physical illness, mediated through psychobiological stress pathways. A comprehensive presentation of the BBFM is found elsewhere (Wood, 2018). In short, the BBFM posits a cascade of effects by which negative “family emotional climate” contributes to parent–child attachment insecurity, which influences child disease activity mediated by child emotion dysregulation (e.g., anxiety and depression) accompanied by physiological dysregulation (Wood et al., 2000) (see Biobehavioral Family Model in Figure 1).
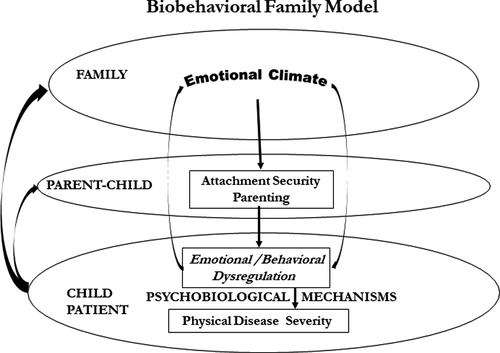
In the BBFM “family emotional climate” is defined as the balance of hostility and warmth within the family's patterns of interactions. These are the most elemental aspects of emotional interaction, thus supporting the broad heuristic application of the model. The model is also unique in positing, with evidence to support, that the impact of family relational stress on disease activity is mediated by psychobiologic stress pathways (Priest et al., 2015, 2019; Roberson et al., 2021; Wood, 1993; Wood et al., 2000; Woods et al., 2020). The BBFM has been extensively applied to childhood asthma (Miller & Wood, 2003). Structural equation modeling (SEM) testing the BBFM model showed that negative family emotional climate statistically predicted child depressive symptoms, which statistically predicted asthma disease severity, with maternal–child attachment insecurity a partial mediator (Wood et al., 2006). The study controlled for asthma treatment adherence, and therefore the findings are consistent with a mediating psychobiologic stress pathway, specifically depression linked dysregulated ANS function, as posited and demonstrated in related studies (Hsu et al., 2020; Lehrer, 1998; Miller et al., 2009; Ritz et al., 2010).
Incorporation of caregiver depression into BBFM modeling in childhood asthma
A parallel line of research suggests that caregiver depression may also contribute to child asthma by way of child depression. Population-based longitudinal and prospective studies reveal increased risk of subsequent asthma symptoms in children having cumulative exposure to maternal depression (Brew et al., 2017; Kozyrskyj et al., 2008; Otsuki et al., 2010). Furthermore, longitudinal studies indicate that maternal depression contributes to offspring depression (Goodman et al., 2011; Hammen, 2009).
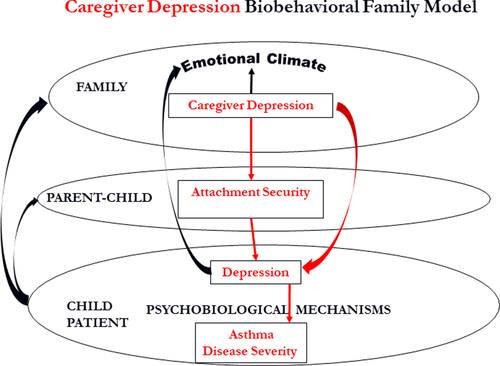
In our previous studies of caregiver depression and childhood asthma, we modified BBFM modeling by replacing family emotional climate with caregiver depression. Findings indicated that negative/hostile maternal parenting mediated the effect of maternal depressive symptoms on child depressive symptoms, and child depressive symptoms mediated the effect of negative parenting on child asthma (Lim et al., 2008). A subsequent study extended these findings to mother–father dyads, and demonstrated inter-parental negativity and negative parenting as mediators linking parental depressive symptoms with child asthma disease activity mediated by child depressive symptoms (Lim et al., 2011).
Maternal depression, maternal–child attachment, child depression, and child asthma
Myrna Weissman's research indicates that the improvement in child depression as a consequence of treating maternal depression was partially explained by improved bonding (Weissman et al., 2015). This is consistent with a meta-analysis of 2064 mother–child pairs which showed that maternal depression was associated with child insecure attachment (Atkinson et al., 2000), and studies that showed that insecure attachment predicted subsequent child and adolescent depression (Blatt & Homann, 1992; Lee & Hankin, 2009; Sund & Wichstrøm, 2002). There are also suggestions in the literature that insecure attachment may be associated with childhood asthma (Cassibba et al., 2004; Mrazek et al., 1987). Taken together, these studies suggest the importance of examining the role of insecure attachment as a possible mediator of the impact of maternal depression on child asthma through child depression.
While it is assumed that caregiver depression will affect “family emotional climate,” by focusing on caregiver depression as the exogenous variable we sought to extend and expand findings from previous longitudinal findings demonstrating an effect of caregiver depression on child asthma (see Figure 2 for the hypothetical extension of the BBFM).
Focus on single maternal families in socio-economically disadvantaged populations
Our research program has focused on socio-economically disadvantaged children with asthma and their families because of their high levels of social-economic stress and documented health disparities (Akinbami et al., 2002). It is our belief that families who have adaptive BBFM-based patterns of relationship will be more able to buffer their children from socio-economic stress. Therefore, we seek to identify specific BBFM pathways by which family relational weaknesses affect child asthma. Such findings can provide specific targets for intervention aimed at improving family function and hence child asthma health outcomes.
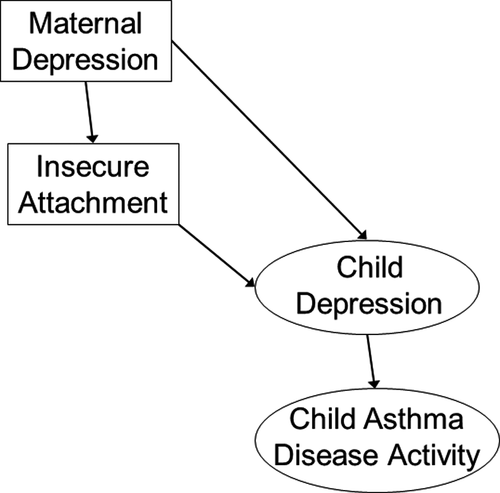
Single maternal families are a predominant family structure in socio-economically disadvantaged inner-city populations of children with asthma (Federico & Liu, 2003). Single mothers are more vulnerable to depression due to economic hardship and social isolation, than are mothers in parental partnership (Brown & Moran, 1997; Cairney et al., 1999, 2003). Furthermore, asthma health disparities exist for children in these families (Moncrief et al., 2014; Scharte et al., 2012). Whereas our previous research examined maternal depression as it related to child asthma in socio-economically disadvantaged populations without regard to family structure, we decided to focus the present study on single parent maternal families because of the maternal vulnerability to depression and because children from these families have the greatest asthma disparities (Akinbami et al., 2002; Bennett, 1994). These are the families that stand to benefit most from novel interventions derived from a better understanding of the pathways underlying the impact of stress on child asthma. Based on previous research and on the Caregiver Depression BBFM model as seen in Figure 2, we designed a cross-sectional study of single mothers and their children with asthma from a socio-economically disadvantaged population. Specifically, we hypothesized that maternal depression would have a direct effect on child depression, that insecure attachment would partially mediate the effect of maternal depression on child depression, and that child depression would mediate the effect of insecure attachment on child asthma (see hypothesized model in Figure 3).
Treatment adherence versus stress in childhood asthma
There are two main potential proximal (to disease activity) links in the cascade of pathways by which maternal depression may impact child asthma: medication treatment adherence and psychobiologic stress mechanisms (Wood et al., 2018). Some studies have pointed to poor adherence as a mediator (Bartlett et al., 2004; Celano et al., 2010; Rodríguez et al., 2017). However, the evidence for poor adherence as a mediator is mixed, with some studies failing to establish the effect of adherence (Ho et al., 2003; McQuaid et al., 2003). The current investigation derives from our previous work demonstrating that asthma-relevant psychobiologic pathways mediate the effect of child depression on asthma (Hsu et al., 2020; Miller et al., 2009). While both adherence and psychobiologic pathways may mediate effects of caregiver depression and other stressors on asthma, the present study seeks to extend previous psychobiologic stress research by testing the proposed Caregiver BBFM model while statistically controlling for treatment adherence. Our findings could help identify specific family relational factors (caregiver depression and insecure attachment) that may transmit the exogenous stress effects of socio-economic disadvantage on child asthma disparities. Confirming specific family-relational pathways could lead to novel targeted family systems interventions to reduce child asthma morbidity in this population. Furthermore, confirming psychobiological pathways of the effect of stress on child asthma could provide compelling evidence for the importance of addressing socio-economic disadvantage to reduce health disparities, rather than simply encouraging better treatment adherence.
METHOD
The current study uses data from a project applying the BBFM to childhood asthma. The overall project examined the impact of family relational stress and child depression on childhood asthma. One previous study using the project data set examined parental self-report data of family emotional climate as it impacted child depression and asthma disease activity (Wood et al., 2006). Another study used data from mothers in single and in two-parent families to examine maternal depression in relation to child internalizing symptoms and asthma (Lim et al., 2008). Another used family interaction observational data to examine marital conflict and negative parenting as mediators of the effects of both parents’ depression on child asthma from two-parent families (Lim et al., 2011). The current study uniquely examines only the single maternal families from the data set. We wanted to focus on this subsample to determine if and how insecure attachment and child depression together mediate the impact of maternal depression on child asthma in families characterized by maternal vulnerability to stress, depression, and child asthma disparities. The goal is to use the findings to develop targeted family interventions for single mothers and their children to reduce child asthma disparities.
Procedures
This study was approved by the Child and Youth Internal Review Board of a Women and Children's Hospital. With IRB approval, parents of children who received a diagnosis of “asthma exacerbation” as a reason for the emergency department (ED) visit were contacted by phone, the study was described, and participants were invited to participate. Consent (parents) and assent (children) were obtained, and a demographics and child medication interview was conducted by phone. Three onsite visits were conducted approximately 1 week apart. The day before each visit a phone medication adherence interview was conducted. Visit one took place in the Asthma Clinic of the Women and Children's Hospital. It included an M.D. diagnostic interview, symptom assessment, and pulmonary function tests to confirm the diagnosis of asthma and characterize disease severity. Visit two, also at the Asthma Clinic, repeated the symptom assessment and pulmonary function tests. Visit three took place in the Child and Family Asthma Studies Center. During visit three asthma symptom assessments and pulmonary function tests were conducted, along with assessments of child and caregiver depression and relationship security. Referral for counseling was made if the child or the mother showed clinically significant depressive symptoms.
The current study is cross-sectional. However, three onsite visits were conducted 1 week apart to achieve average, and therefore more reliable, indices of the child's current medication adherence and pulmonary function (Forced Expiration Volume in 1 s [FEV1]). The maternal and child psychological assessments occurred only on visit 3.
Participants
Single maternal families were selected from the larger sample of socio-economically disadvantaged families who participated in our family stress and child asthma research program. Children and their families were serially recruited from patients coming to an inner-city pediatric ED because of asthma symptoms. Ninety-one percentage of the participants in the current study were of minority status (see Table 1 for minority status). Inclusion criteria were (a) patient aged 7–17 years, (b) diagnosis of asthma, (c) living in a single maternal family (defined as a mother-only household), and (d) English speaking. Exclusion criteria were (a) co-morbid chronic medical conditions (other than allergy) and (b) living in residential facilities. Contact was established with approximately 60% of the potential participant pool. Eighty-eight percentage of contacted families were eligible. Sixty-one percentage of those eligible enrolled. Those who completed versus those who were eligible for the study did not differ in age (M = 11.34, SD = 2.75 vs. M = 11.50, SD = 2.87; t908 = 0.85, p = 0.40), gender (56.3% vs. 59.5% male; Χ2 = 0.33, p = 0.34), or Medicaid status (28% vs. 25% Medicaid; Χ2 = 1.10, p = 0.30). However, those who completed included more African Americans and fewer Caucasian Americans compared to those who were eligible for the project but did not participate (60% vs. 47% AA, 27% vs. 38% CA, 13% vs. 15% other; Χ2 = 15.58, p < 0.001). Among the families who completed the full study (N = 397), only single maternal families (N = 202) were studied in the present investigation. The sample of single maternal families differed from that of two-parent families in the larger dataset redistribution of insurance (57% vs. 31% Medicaid status) and educational status of mothers (60% vs. 40% high school or less). Children ranged in age from 7 to 17 years (M = 11.3, SD = 2.6). Mothers ranged in age from 23 to 60 years (M = 37.3, SD = 7.7).
| n (%) | Mean (SD) | |
|---|---|---|
| Child | ||
| Age in year | 11.30 (2.6) | |
| Gender | ||
| Boy | 107 (53.0%) | |
| Girl | 95 (47%) | |
| Ethnicity | ||
| African American | 140 (69%) | |
| European American | 18 (9%) | |
| Hispanics | 24 (12%) | |
| Other minority | 20 (10%) | |
| Asthma disease activity | ||
| Intermittent | 24 (12%) | |
| Mild persistent | 28 (14%) | |
| Moderate persistent | 79 (39%) | |
| Severe persistent | 71 (35%) | |
| Mother | ||
| Age in year | 37.3 (7.7) | |
| Education status | ||
| Less than high school | 46 (23%) | |
| High school graduate | 89 (44%) | |
| Some college and graduate | 67 (33%) | |
| Biological mother | ||
| Yes | 192 (95%) | |
| No | 10 (5%) | |
The characteristics of the study sample are shown in Table 1.
Measures
Demographics
The child's gender, age, ethnicity, family type, and mother's education, age, and insurance were obtained by interview and were used as control variables when appropriate.
Maternal depressive symptoms
The Beck Depression Inventory-II (Beck et al., 1996) is a self-report instrument, measuring depressive symptoms in adults with high reliability and established validity. For the current sample, the internal consistency was 0.89.
Child depressive symptoms
Child depressive symptoms were assessed both with a self-report and structured clinical interview. The Children's Depression Inventory (CDI) (Kovacs, 1985) is a 27-item self-report of depressive symptoms with moderate to high internal consistency, test–retest reliability, and established validity (Twenge & Nolen-Hoeksema, 2002). In this sample, the internal consistency was 0.84. The Child Depression Rating Scale-Revised (CDRS-R) (Poznanski & Mokros, 1995) is a 17-item clinician-guided interview measure of depressive symptoms. The CDRS-R has good test–retest reliability, internal consistency, and inter-rater reliability (Poznanski & Mokros, 1995). Half of CDRS-R interviews were completed by an M.D. child psychiatrist or a Ph.D.-level clinician/researcher, and the remaining by a masters-level clinician. Both were trained by the child psychiatrist, using standard CDRS-R training procedures. For the current sample, the inter-rater reliability for CDRS-R was 0.91, and the internal consistency was 0.86.
Mother–child attachment
Mother–child attachment was reported by the child using the Relatedness Questionnaire, a 17-item reliable and valid instrument (Lynch & Cicchetti, 1991). This instrument includes two dimensions: psychological proximity seeking and emotional quality. Proximity seeking reflects the child's desire to be closer to the parent and better attended to. Emotional quality refers to the positive (happy, calm, etc.) and negative (angry, sad, and scared) emotions the child feels in the presence of the parent. The internal consistencies for this study were 0.84 (proximity seeking) and.85 (emotional quality). Configurational algorithms yield five categories of relatedness: optimal, adequate, deprived, avoidant, and confused (Lynch & Cicchetti, 1991). The categories were designed to be analogous to the attachment-style categories established by other empirical means. In our study, consistent with other studies, children with optimal or adequate styles were categorized as secure, whereas the other three styles were categorized as insecure.
Asthma disease activity
Standard criteria for asthma disease activity (National Heart Lung & Blood Institute, 2007) were used to characterize the level of disease. The Asthma Disease Activity rating was based upon the configuration of the average frequency of daytime and nighttime symptoms and measures of pulmonary function. The symptoms were assessed by the research nurse or asthma specialist during an interview with the child and parent. FEV1 was used to evaluate pulmonary function. FEV1 was measured using a portable spirometer (Nelcor Puritan Spirometer “Renaissance” #220) that met the American Thoracic Society performance standards. A trained pulmonary function technician conducted the spirometric maneuvers. Using the NHLBI 2007 criteria, Asthma Disease Activity was rated independently by the asthma research nurse practitioner and a masters level clinician, both of whom were trained in the NHLBI 2007 criteria by the asthma physician co-investigator. They were blinded to maternal and child depression and attachment scores. The range of disease activity was 1 (mild intermittent), 2 (mild persistent), 3 (moderate), and 4 (severe persistent). Agreement between raters for asthma disease activity was 87%. All discrepancies were reconciled by the asthma physician co-investigator, with only consensus scores used in the data analysis.
Treatment adherence control variable
Chart reviews and caregiver and patient interviews were conducted by the research nurse to determine medications prescribed (i.e., medication name, dose, and frequency). Medication adherence to the prescription was assessed with Bennett Johnson's 24-h recall interview (Johnson et al., 1992), adapted for child asthma (Bender et al., 2008). Adherence to controller medication as prescribed was assessed by three phone interviews occurring the day before each research visit. The research nurse or PhD-level clinician asked the child (>13 years old) or the caregiver (child <13 years old) the medication name, dose, and when it was taken during the 24 h preceding the call. Based on the phone interviews and the prescription from the child's physician, medication adherence was evaluated according to how consistently the medication was taken according to prescription. The interviews were rated independently by the asthma research nurse and PhD-level clinician using a four-point scale (1-very poor, 2-fair, 3-good, and 4-very good), and then consensed if there was a discrepancy. The asthma physician co-investigator trained the raters according to the 24-h recall method. Each interview was consensed. Inter-rater reliability before consensing was 0.95. Medication adherence in the current study was correlated with FEV1 scores (r = 0.20, p < 0.05), indicating adequate adherence assessment.
Data analyses
Pearson correlation analyses were used to test bivariate associations among the study variables. SEM was used to test the direct and indirect pathways posited. Because SEM modeling tests hypothetical directions of effect, it is customary to refer to “statistical prediction” which is not meant to convey causal effect. We conform to this language usage. SEM analyses were conducted with AMOS 21.0 using maximum likelihood estimation. All SEM models were examined for model fit using widely used statistical indices: chi-squares, IFI, CFI, and RMSEA.
Maternal depression and insecure attachment were entered as observed variables to the model. The attachment was coded dichotomously, 0 for securely attached and 1 for insecurely attached. Child depression and asthma disease activity were entered as latent variables to the model. The self-report depression (CDI) scores and clinical expert-rated depression (CDRS) scores were used as indicators of the child's depression. The pulmonary function score (FEV1), daytime, and nighttime symptoms of asthma were used as indicators of the child's asthma disease activity. Two variables were entered as control variables to the model; one was the education level of the mother (coded dichotomously, 0 for high school graduate or less and 1 for partial college or more) because it was associated with maternal depression. The other was medication adherence because it was associated with pulmonary functions (i.e., FEV1) of the child.
There were <2% missing data in three study variables (i.e., CDI, daytime symptoms, and nighttime symptoms), and 12% missing data in the CDRS variable. The patterns of parameter estimate and fit measures were similar with or without cases with missing data. Considering the potential moderating role of child gender in models of depressive symptoms and family process (Davies & Lindsey, 2001; Davies & Windle, 1997), preliminary SEM analyses were conducted to determine whether child gender moderated the hypothesized pathways in the model using multi-group analysis (Hong et al., 2003). A model that allowed parameter estimates to differ in the two groups was compared with a model that constrained path coefficients to be identical for the two compared groups. There was no significant difference between the gender-specific model and the constrained model, Δχ2(6) = 8.81, p = 0.18. That is to say, the hypothesized model was not significantly different according to gender. Thus, we performed subsequent analyses using the full sample. The sample size and composition were not sufficient to test moderating effects of child ethnicity. Except for the FEV1 scores (r = 0.22, p < 0.01), there were no associations between age and the study variables, so age was not tested as a moderator.
We began analyses by testing a measurement model of child depressive symptoms and asthma disease activity with indicators. Then, we identified the hypothesized model and an alternative model with a more inclusive pathway, respectively. In the alternative model, the direct path from insecure attachment to asthma disease activity was added because the insecure attachment was significantly correlated with multiple indicators of asthma disease activity at the bivariate level. Differences in the chi-square values of the two nested models indicated whether the additional link in the second model was necessary to better fit the data. Finally, we conducted a post-hoc analysis to probe for significant mediating effects of the hypothesized model using bootstrapping procedures with the imputed data.
RESULTS
Descriptive statistics and correlations among study variables
Descriptive statistics and bivariate correlations of the study variables are presented in Table 2. About 21% of mothers showed depressive symptoms above the clinical cutoff for moderate to severe depression (scores >19), 19% of mothers evidenced mild depressive symptoms (scores of 14–19), and 60% of mothers showed minimal depressive symptoms (scores of 0–13). About 25% of the children scored above a clinical cutoff (score of 13) on the CDI, and 19% scored in the clinical range of the CDRS-R (score of 40 or above). For asthma disease activity, participants were characterized as 12% mild intermittent, 14% mild persistent, 39% moderate persistent, and 35% severe persistent. The distribution of medication adherence was as follows: 21% very poor, 21% fair, 17% good, and 41% very good.
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 BDI | 12.44 (8.98) | ||||||||
| 2 Insecure attachment | – | 0.17* | |||||||
| 3 CDI | 8.8 (6.71) | 0.24** | 0.47*** | ||||||
| 4 CDRS | 31.25 (9.59) | 0.24** | 0.33*** | 0.63*** | |||||
| 5 FEV1 | 89.02 (18.37) | −0.07 | −0.17* | −0.06 | 0.01 | ||||
| 6 Day symp | 2.38 (1.13) | 0.02 | 0.24** | 0.31*** | 0.23** | −0.10 | |||
| 7 Night symp | 2.27 (1.38) | 0.02 | 0.18* | 0.24** | 0.22* | −0.17* | 0.53*** | ||
| 8 Adherence | 2.77 (1.19) | −0.07 | −0.05 | −0.07 | −0.01 | 0.20** | −0.10 | −0.07 | |
| 9 Education | – | −0.14* | −0.02 | −0.09 | −0.07 | 0.13 | −0.12 | −0.15* | 0.03 |
- Abbreviations: BDI, Beck Depression Inventory; CDI, Child Depression Inventory; CDRS, Child Depression Rating Scale; FEV1, Forced Expiratory Volume in 1 s; Day Symp, Daytime Symptoms; Night Symp, Nighttime Symptoms; Adherence, Medication Adherence.
- Insecure Attachment and Education were dummy coded, insecurely attached (30.2%) 1, securely attached 0; partial college or more 1 (33.0%), high school graduate or less 0.
- *p < 0.05; **p < 0.01; ***p < 0.001.
Testing the hypothesized model
Before testing the hypothesized model, we assessed the measurement model of both child depression and asthma disease activity (allowing the two constructs covary) by reviewing the magnitude and significance of the factor loadings, as well as the CFI and RMSEA indices of model fit. Results of the analysis suggested that all criteria were satisfactory, as the model generated all significant factor loadings, with χ2(4, N = 202) = 4.35, p = 0.36, CFI = 0.99, RMSEA = 0.02. Thus, the presence of signs of relationships between the predictor and the criteria was confirmed.
Then, we conducted model tests of mediation. In the following model testing process, medication adherence was controlled for by specifying a direct path from adherence to asthma disease activity; this approach was taken because the literature suggests that child and family dysfunction are associated with poor adherence in asthma. The education level of the mother was also controlled for by specifying a direct path to maternal depressive symptoms because there was a significant negative correlation (r = −0.14, p = 0.049) between the two variables. In addition, the education level of the mother and medication adherence were allowed to covary.
In the first step, we began with identifying the hypothesized model, which estimated both direct and indirect paths from maternal depressive symptoms to child depressive symptoms via insecure attachment, and an indirect path from maternal depressive symptoms to child asthma disease activity through insecure attachment and child depressive symptoms serially. The hypothesized model (see in Figure 2) provided an excellent fit to the data, χ2(24, N = 202) = 31.02, p = 0.15, CFI = 0.97, IFI = 0.97, RMSEA = 0.04. Modeling indicated that maternal depressive symptoms directly predicted child depressive symptoms (β = 0.21, p < 0.01) and insecure attachment to mother (β = 0.17, p < 0.05). The strength of association between insecure attachment to mother and child depression was beyond the moderate level (β = 0.50, p < 0.001), indicating at least a moderate statistical effect of insecure attachment on child depression. Child depression, in turn, predicted increased asthma disease activity (β = 0.43, p < 0.01).
Thus, the results presented in Figure 4 were consistent with our hypothesis that insecure attachment mediates the effect of maternal depression on child depression, and child depression mediates the effect of insecure attachment on child asthma. In other words, maternal depression may affect child asthma serially mediated by insecure attachment and child depression.
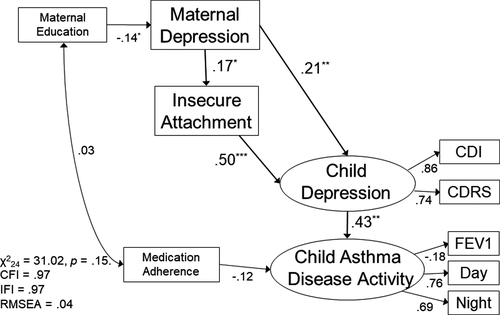
Although the hypothesized model was found to have a strong fit to the data, it is possible that the interrelations of the study variables could also fit an alternative model. Thus, in the second step, we tested an alternative model. A direct path from insecure attachment to disease activity was added to the hypothesized model because the insecure attachment was significantly correlated with multiple indicators of asthma disease activity at the bivariate level (as presented in Table 2). This alternative model was estimated to examine the plausibility of pathways for the observed relations in the study. The alternative model showed adequate fit to the data, χ2(23, N = 202) = 29.62, p = 0.16, IFI = 0.98, CFI = 0.98, RMSEA = 0.04, but the additional direct path from insecure attachment to disease activity was not significant.
In the third step, we compared the two nested models using the chi-square difference test and found that the alternative model did not result in a significant improvement in fit compared to the hypothesized model, Δχ2(1, N = 202) = 1.16, p = 0.28. This finding supported the hypothesized model as a better model compared to the alternative one because it fits the data equally well with more parsimonious pathways. It is also noteworthy that the results of testing this more inclusive model indicated that insecure attachment does not directly affect asthma disease activity.
In the final step, we tested the significance of indirect effects in the hypothesized model using bootstrapping procedures. The findings are presented in Table 3. The bootstrapped unstandardized indirect effect from maternal depressive symptoms to child depressive symptoms was 0.05, 95% CI [0.01, 0.11], from maternal depressive symptoms to asthma disease activity was 0.01, 95% CI [0.01, 0.03], from insecure attachment to asthma disease activity was 0.44, 95% CI [0.22, 0.71], respectively. Thus, all indirect effects in the hypothesized model were statistically significant.
| Estimate | SE | 95% CI | p | |
|---|---|---|---|---|
| Maternal depression to child depression | ||||
| Total effect | 0.191 | 0.044 | 0.107, 0.279 | 0.001 |
| Indirect effect (maternal depression →insecure attachment →child depression) | 0.054 | 0.024 | 0.011, 0.109 | 0.012 |
| Direct effect | 0.137 | 0.042 | 0.056, 0.218 | 0.001 |
| Insecure attachment to child asthma disease activity1 | ||||
| Indirect effect (insecure attachment →child depression →child asthma disease activity) | 0.443 | 0.128 | 0.217, 0.711 | 0.001 |
| Maternal depression to child asthma disease activity2 | ||||
| Specific indirect effect (maternal depression →child depression →child asthma disease activity) | 0.010 | 0.004 | 0.004, 0.020 | <0.001 |
| Specific indirect effect (maternal depression →insecure attachment →child depression →child asthma disease activity) | 0.004 | 0.002 | 0.001, 0.009 | 0.008 |
| Overall indirect effect (maternal depression →insecure attachment →child depression →child asthma disease activity) | 0.014 | 0.005 | 0.006, 0.026 | <0.001 |
Note
- No direct paths were posited in the hypothesized model at 1 and 2 pathways.
DISCUSSION
The findings of this study were consistent with the hypothesized model, which posited that maternal depression affects child asthma, serially mediated by insecure attachment and child depression. It is also noteworthy that the testing of an alternative model including a direct pathway from insecure attachment to disease activity indicated that this direct pathway was not significant, lending further credence to our hypothesis that insecure attachment operates through child depression in its effect on asthma.
Our findings extend the prospective studies demonstrating that caregiver depression precedes and predicts subsequent asthma symptoms in their children (Brew et al., 2017; Kozyrskyj et al., 2008; Otsuki et al., 2010). In addition, these findings are consistent with and expand the BBFM as described above, thus supporting the model's heuristic and clinical value. They provide the rationale and foundation for future longitudinal and/or family intervention study designs to further elucidate directions of effect and develop novel targeted family-based interventions.
Theoretical implications
Because the present study specifically controlled for adherence, the results lend support to the research demonstrating psychobiologic stress pathways in childhood asthma. The authors do not dispute the important role that medication adherence and good asthma management play, nor the evidence that supporting, educating, and empowering stressed caregivers may improve child asthma outcomes, through improving asthma management (Foronda et al., 2020). However, our past and current research suggest that although adherence is important, it may not be sufficient when the child is depressed and/or living in the context of impaired parent–child attachment or hostile parenting.
The effect of caregiver depression on child asthma through child depression has important links to research demonstrating psychobiological mechanisms underlying the effect of child depression on asthma. Specifically, studies show that child depressive symptoms, in children with asthma, are associated with autonomic nervous system dysregulation (specifically increased vagal/cholinergic responsivity) and airway resistance in response to laboratory stress (Hsu et al., 2020; Miller et al., 2009). Taken together, this psychobiologic research and the current findings demonstrate the importance of the further study of the pathophysiologic mechanisms by which family relations impact stress and depressive symptoms in children, which in turn impact airway function in children with asthma.
The BBFM was intentionally conceived to inspire alternative variable configurations. It has been shown to be useful for studying various emotional and physical diseases and disorders in different age groups, family configurations, and ethnic cultures (Priest et al., 2015, 2019; Roberson et al., 2021; Wood, 1993; Wood et al., 2000; Woods et al., 2020). We propose that the BBFM may serve as a prototype for integrative multi-level modeling that examines family-psycho-biologic pathways by which family relational process not only influences childhood disease but also either transmits the impact of socio-economic stress on a child emotional and physical well-being, or helps buffer the child from these effects.
Limitations and future directions
Our study was cross-sectional and therefore findings cannot demonstrate causal effects. While we posited that caregiver depression would contribute to child asthma mediated by insecure attachment and child depression, it is likely that child depression and worse asthma disease activity contribute to maternal depression. Even so, once the caregiver is depressed, for whatever reason, that depression may in turn worsen the child's emotional well-being and contribute to an increase in asthma disease activity. Longitudinal intervention research is called for to test the directions of predicted effect in the model examined in this study and to develop efficacious family-based interventions.
The samples in our projects were intentionally recruited from an inner-city ED to recruit families who were economically and socially disadvantaged because they frequently rely on emergency medical settings for care. Therefore, our findings may not be appropriately generalized beyond at-risk inner-city populations. Furthermore, because our study focused on single maternal families, the findings may not generalize to single paternal families nor two-parent families. However, we regard it as a strength of our study to focus on single maternal families whose children are known to have the greatest health disparities and to define specific pathways by which these disparities may come about.
We found no moderating effects of child gender. There was insufficient sample size and demographic distribution to examine multiple demographic moderating effects. Potential moderating effects specific to socio-economic disadvantage, including perceived and systemic prejudice and racism should be examined as they relate to caregiver depression and its impact on child asthma.
Despite the limitations in this study, we conclude that these findings lay the groundwork for future testing of causal pathways linking caregiver depression and childhood asthma outcomes, and examination of socio-economic moderating factors. Such research would facilitate the development of targeted family therapy, and social system-based interventions, to improve asthma outcomes and reduce health disparities, particularly for children in vulnerable single-parent families. Such approaches could be applied to other childhood diseases and disorders as well.
Clinical implications
The BBFM is not a model of change. Rather, it is a model of both adaptive and maladaptive family function. As such it provides for the identification of dimensions and configurations of family relations that are targets for change to improve family function.
The findings of the current study suggest that caregiver depression and parent–child relationship security may be important targets for family therapeutic intervention to improve child asthma. There are many evidence-based interventions that may be integrated into family-based interventions. There is good evidence that treating caregiver depression can improve parent–child bonding and child depression (Weissman et al., 2015; Wickramaratne et al., 2011). In addition, we found, in a pilot study (n = 8), that treating depressed caregivers with medication led to subsequent improvement in the child's asthma symptoms (Brown et al., 2008). There are also evidence-based interventions for child depression that could be incorporated (Compton et al., 2004), as well as interventions to improve parent–child attachment (Berlin et al., 2008; Diamond et al. 2014). Integrating these approaches into BBFM-informed systemic family therapeutic intervention could help improve outcomes and reduce health disparities for children with asthma, and possibly for other stress-related illnesses as well.
Policy implications
The greatest asthma health disparities exist for inner-city children living with single mothers who are vulnerable to depression because of conditions of economic hardship, racism, and social isolation (Brown & Moran, 1997; Cairney et al., 1999, 2003; Federico & Liu, 2003; Moncrief et al., 2014; Scharte et al., 2012). It is essential to identify family psychobiologic pathways by which the stress caused by socio-economic disadvantage are transmitted to children. Only then will the medical profession, and the general public be compelled to recognize the impact of socio-economic engendered psychobiologic stress on child asthma. This recognition could inspire advocacy for resources and approaches that can address not only the biological aspects of asthma, through medication and disease management but also the social and family stress factors potentiating the child's asthma.
ACKNOWLEDGEMENTS
This study was supported by 5RO1MH064154 from the National Institute of Mental Health and R01HL123609 from the National Heart Lung and Blood Institute. We wish to acknowledge Ms. Melina Hillsberg and Mr. William R. Tallmadge for assistance in preparing this manuscript.




