Regenerative endodontic treatment and traumatic dental injuries
Abstract
Pulp necrosis is the most common complication following dental trauma and is often associated with apical periodontitis. The management of these teeth is challenging in terms of large root canals, open apices, thin dentinal walls, and short roots. Over decades the conventional treatment for these teeth was calcium hydroxide apexification, a time-consuming procedure despite high success rates. Subsequently after the introduction of mineral trioxide aggregate and hydraulic calcium silicate materials single visit apical plug procedures became increasingly practiced with comparable success rates to the conventional apexification. The search continued afterward for a clinical procedure that may stimulate further root development and apical closure to avoid the long-term complication of root fracture after apexification. Regenerative procedures using stem cells derived from the apical papilla and blood clots as scaffolds were then introduced for the management of immature teeth, with variable protocols and success rates. This review will cover the evidence available and current position of regenerative endodontic procedures in traumatized immature teeth with apical periodontitis, in terms of clinical protocols, outcome, and potential prognostic factors.
1 INTRODUCTION
Calcium hydroxide apexification and apical plug/barrier techniques employing hydraulic calcium silicate cements (HCSCs) have been utilized for treatment of immature teeth with pulp necrosis and infection with high success rates. Generally, these mechanistic treatment approaches do not result in further root maturation. A meta-analysis or regenerative endodontic treatment (RET) and apexification reported success which was defined as healing of apical periodontitis of 91% for RET and 95% for apexification with this result for the two treatments not considered statistically significant.1 RET for the management of immature teeth that have sustained pulp necrosis and apical periodontitis/abscess has been advocated as there is the potential for further root maturation and the return of vital tissue into the pulp.2, 3 The aim of RET is to regenerate the pulp-dentine complex that has been damaged by infection and/or trauma.4 RET utilizes the triage of tissue engineering concepts of stem cells, bioactive materials that can act as scaffolds and growth factors to provide the micro-environment for regeneration and repair.4-8 A fourth pillar to this triage is the synergistic interaction of these bioengineering applications that can allow biological approaches for the treatment of pulp necrosis.8 The concept of revascularization of the pulp space and biological repair is well known in dental traumatology following avulsion injuries of immature teeth.9 Similarly, RET with stringent disinfection protocols allow utilization of biological approaches for management of teeth with an infected pulp space.
The interest in RET has been substantive since the first landmark cases of Iwaya et al.10 and Banchs and Trope,11 which involved premolar teeth where pulp necrosis and infection had followed fractured occlusal tubercles. At that time the procedure was termed “revascularization”. The terms regenerative endodontic treatment. Revascularization, revitalization, maturogenesis have all been terms to describe this technique.12, 13 For example “regenerative endodontic treatment” has been adopted by the American Association of Endodontists (AAE).14 While the European Society of Endodontology (ESE) guidelines use the term “revitalization” instead of “regeneration”.12, 13
The term “Revascularization” is well understood in the dental trauma literature and relates to teeth without apical periodontitis where the blood supply is restored to the traumatized tooth. In respect to RET which involves treatment of teeth with pulp necrosis and apical periodontitis this term and others has caused confusion to many practitioners and as discussed above is not universally accepted by the major endodontic associations. The American Association of Endodontists (AAE) glossary of endodontic terms define revascularization as “the restoration of the blood supply”.15 In essence, the term “revitalization” has the same meaning as it implies a return of the blood supply. The AAE Glossary of Endodontic Terms define “regenerative endodontics” as “Biologically-based procedures designed to physiologically replace damaged tooth structures, including dentine and root structures, as well as cells of the pulp-dentine complex”,15 As will be discussed later, there is confusion over the term “regenerate” as this implies regeneration of pulp where histological studies show repair rather than regeneration with the new or replaced tissue resembling periodontal-derived fibrous tissue, cementoid and osteoid tissue. However, a strict interpretation of the AAE guideline define RET as procedures to “replace damaged tissue” and neither “regenerate” or “repair” is mentioned in the definition explanation. The true sense of “regeneration” may require development of cell-based (utilizing introduced stem cells, growth factors and manufactured scaffolds) rather than the cell-free protocols currently employed with clinical protocols of blood clots or centrifuged blood substitutes.7
Regenerative endodontic treatment has been described as a paradigm shift in the treatment of immature teeth with pulp necrosis and or apical periodontitis/abscess.16, 17 In the early days of RET in 2007, Murray et al advocated for a call of action to develop therapies for clinical use involving tissue engineering concepts utilizing adult stem cells, scaffolds and growth factors.5 Subsequently in 2008, Huang et al. reported on “The hidden treasure in apical papilla: the potential role in pulp/dentine regeneration and bioroot engineering”.18
The first studies on RET in traumatized teeth were published in 2008.19, 20 Concerns with revascularization were subsequently raised stating that the procedure could not be considered predictable as there were no criteria for subjective analysis particularly in cases with long standing pulp necrosis prior to RET.21 Later in 2012, Andreasen and Bakland further questioned the type of tissue that was generated by this procedure.22 The authors reported that revascularization could result in dentine formation leading to pulp canal calcification. There were concerns that the long-term prognosis was not known when there was ingrowth of cementum, periodontal ligament and bone. These were valid questions at the time and the answers remain controversial.
In 2016, RET was described as the way forward and the first treatment option for immature teeth with pulp necrosis23 and was also advocated for mature teeth with necrotic pulps.24 The AAE and the ESE released position statements on RET.12, 14 By way of contrast, in 2017 it was reported that the evidence for RET is extremely weak and regenerative endodontic protocols should only be used when the prognosis of alternative treatments is considered extremely poor.25 The European Academy of Paediatric Dentistry guidelines support the placement of an apical barrier of mineral trioxide aggregate (MTA) followed by root canal obturation as the treatment of choice for immature teeth with pulp necrosis.25
A recent survey of the attitude and practice of RET among pediatric dentists and endodontists from 13 countries, reported that 43% of the participants have not practiced RET yet, with a gap in knowledge of RET protocols, clinical applications and available evidence.26
The purpose of this review is to examine the evidence available for RET in traumatized immature teeth with apical periodontitis, in terms of outcome, potential prognostic factors and comparisons with other treatment modalities including apexification and apical plugs.
2 INCIDENCE OF TRAUMATIC DENTAL INJURIES
Pulp necrosis is the most common complication following dental trauma with the most affected teeth being the maxillary incisors.27 Numerous studies reported an incidence of traumatic dental injuries of >20% of the population of respective countries and mostly among children.26-32 It has been estimated that more than a billion-living people have sustained dental trauma.33 Therefore, pulp necrosis in immature teeth is of considerable concern where there is a higher risk of tooth loss if root maturation is arrested in children aged 7–9 years. The quality of life following dental trauma is an important issue. Therefore, a treatment that minimizes the risk of tooth loss is desirable.34
3 PULP DIAGNOSIS IN TRAUMATIZED TEETH
Establishing a definitive diagnosis is essential for treatment planning and achieving favorable outcomes, where pulp survival must be considered optimal. It is essential that clinicians be aware that teeth with open apices have better outcomes and recovery after traumatic injuries compared to mature teeth.35, 36
The IADT guidelines recommend clinicians to consider the results of history of pain, pulp sensibility testing, tenderness to percussion, discoloration, the presence of sinus tracts and/or swelling, and the radiographic appearance of a periapical radiolucency, all together in diagnosing pulp necrosis and infection before initiating intervention.37, 38
4 TREATMENT OPTIONS FOR THE TRAUMATIZED IMMATURE TOOTH WITH PULP NECROSIS AND APICAL PERIODONTITIS
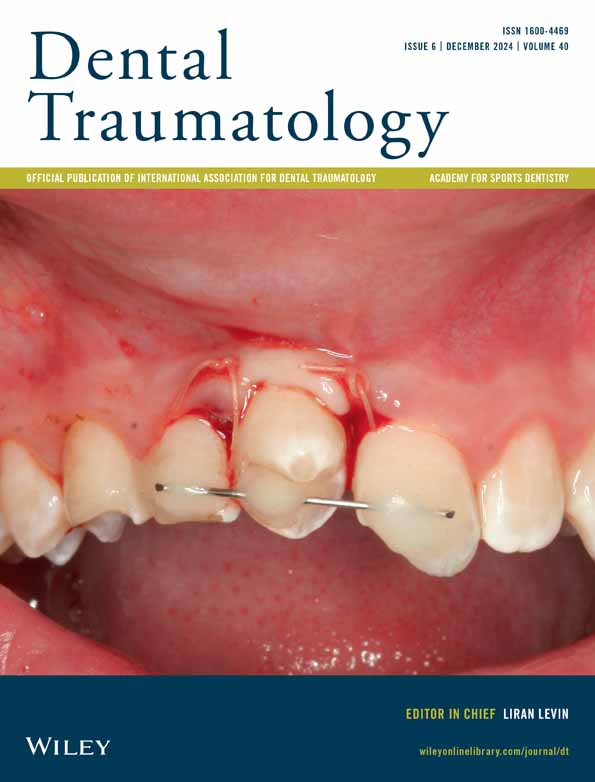
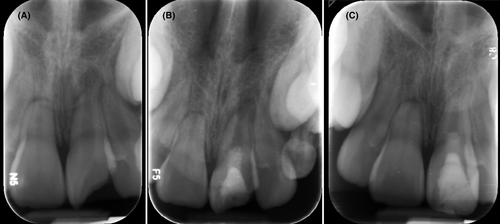
The inherent difficulties in the treatment of immature traumatized teeth are the open apex which poses risks of apical extrusion of endodontic materials (Figure 1), and incomplete root maturation where there is the risk of oblique root fracture.39 Apexification, apical barriers and regenerative endodontic procedures have been practiced in the management of these teeth.
Traditionally calcium hydroxide apexification was used for the management of open apex teeth. A systematic review reported success rates for calcium hydroxide apexification ranged between 87% and 93%.40 It requires multiple applications to stimulate hard tissue barrier formation at the apex enabling conventional root canal therapy to be undertaken without extruding foreign material into the apical tissues.41 Disadvantages of this approach include; it is a time-consuming procedure that may require 9–24 months of treatment,42 requires patient cooperation, patient's and parent's compliance and there is a risk of coronal leakage and contamination of the root canal between appointments.
The effect of long-term calcium hydroxide on root dentine strength remains controversial. Several studies cite Andreasen et al. for not undertaking a calcium hydroxide apexification.43 This animal study reported a time dependent decrease in the fracture strength for teeth dressed with calcium hydroxide (nearly 50% in a year).43 However these results were not substantiated by a subsequent study that reported no difference in fracture strength reduction between the experimental and control groups.44 In the landmark study by Cvek in 1992 on the incidence of transverse root fracture after calcium hydroxide apexification, he analyzed 885 non-vital traumatized incisors and reported that the frequency of fractures was dependent on the stage of root development. It ranged from 77% in teeth with the least developed roots to 28% in teeth with the most developed roots.39
With the development of MTA and the HCSCs, an alternative to apexification with calcium hydroxide is the apical plug technique. The MTA apical plug approach requires a shorter treatment time usually involving an initial dressing of the canal with calcium hydroxide followed by a second appointment where the MTA/HCSCs material is placed. The remainder of the canal is filled with theromoplacticised gutta-percha and sealer,45 or it can be filled with resin composite and fiber posts.46 HCSCs are biocompatible and osseo-inductive allowing cell proliferation and differentiation to produce a hard tissue barrier.5, 47 Numerous studies have reported successful outcomes for MTA apical barrier techniques.17, 48 A systematic review and meta-analysis reported pooled survival rates of 97.1% and success rates of 94.6% for MTA apical plug.1
These approaches of calcium hydroxide apexification or MTA-apical plug techniques do not result in further root maturation with the root remaining weak and subject to oblique root fracture following a secondary trauma.42, 49
On the contrary, RET is a biologically-based treatment approach which has the potential for inducing further root development in terms of root length and thickness. This may strengthen the root and limit the risk of oblique root fractures. RET is advocated by the AAE,14 the ESE,12 the IADT,37, 38 The American Academy of Pediatric Dentists (AAPD)50 as an accepted treatment protocol for treatment of immature permanent teeth.
The main principle in RET is to disinfect the root canal system with no mechanical instrumentation for the walls and subsequently attract mesenchymal stem cells from the apical papilla of immature teeth into the root canal to ideally differentiate into regeneration or repair of the pulp-dentine complex.14, 51 The chemical debridement of the root canal space is supported by the three pillars of tissue engineering namely: stem cells, growth factors and a scaffold.
A systematic review on the outcome of RET procedures reported a high pooled survival rate of 97.8% and a 91.3% success rate over an average follow-up period of 16.7 months.1 Furthermore, a recent systematic review and meta-analysis on the effectiveness of RET reported the success and survival rates of teeth treated with RET were not statistically different from those treated with pulpectomy.52 These findings suggest that treatment with RET is a viable alternative to pulpectomy and conventional treatments.
Similarly, studies have shown successful treatment of traumatized mature teeth with RET.53, 54 Youseff et al. reported successful outcomes in 20 anterior teeth with large periapical lesions treated with either a blood clot or platelet rich-fibrin (PRF), with no significant differences between the two treatment modalities.53 Lu et al. treated 37 mature teeth of which 27 teeth had an etiology of trauma with an average follow-up of 4.3 years and the periapical lesion resolved in 89.2% of the teeth.54
5 RET PROTOCOL
A detailed protocol for RET was released in 2016 by the ESE12 and the AAE and recently revised by the AAE in 2021.14 In essence, the procedure is performed over two visits with three main principles. First, minimal to no filing of the canal so as not to weaken the immature root. Second, a stringent disinfection using low concentration sodium hypochlorite and intracanal medicaments, to minimize damage to the “stemness” capacity of multi-pluripotential cells which differentiate into cells that enhance root maturation. Third, induce bleeding into the canal and await blood clot formation to act as scaffold for regeneration. A hydraulic calcium silicate-based material is subsequently placed over the blood clot followed by an adequate coronal restoration.12, 14
6 DISINFECTANTS, MEDICAMENTS AND SCAFFOLDS
Sodium hypochlorite in concentrations of 1%–6% have been used in RET.55 However, the AAE Clinical considerations for RET recommend the use of 1.5% sodium hypochlorite followed by 17% EDTA,14 as high concentration sodium hypochlorite is cytotoxic to stem cells.56 EDTA demineralizes the dentine to release growth factors contained in the dentine matrix of the root,57-59 and partially reduces the adverse effects on stem cells caused by using sodium hypochlorite.56 EDTA conditioning of the dentine promoted the adhesion, migration and differentiation of pulp stem cells as well as stem cell differentiation.60 For this reason, EDTA is recommended as a final rinse before inducing a blood clot.
Triple antibiotic paste consisting of minocycline, ciprofloxacin and metronidazole has been used in RET11 based on its excellent antimicrobial activity to eliminate bacteria in the infected root canals in vitro.61, 62 The triple antibiotic paste has been shown to affect the survival of stem cells from the apical papilla in vitro.63, 64 Therefore, it is recommended to use triple antibiotic paste at a concentration no >1 mg/mL (0.1–1 mg/mL) in RET to avoid damage of stem cells from the apical papilla.12 In comparison the ESE position statement on the use of antibiotics in RET has suggested that the use of antibiotics is better avoided, and replaced by calcium hydroxide medication to avoid antibiotic resistance and the negative effects of tooth staining.12 However, antibiotic pastes are still recommended as a medicament by the AAE.12, 65
Calcium hydroxide is also recommended as an intracanal medicament for its antimicrobial properties.12 Furthermore, attachment of human apical cells to root dentine was greater for teeth treated with calcium hydroxide compared to triple antibiotic paste.66 However, when calcium hydroxide is placed in the apical half of the root canal there was less of an increase in dentinal wall thickness than when calcium hydroxide was restricted to the coronal half of the root canal space.67
The use of calcium hydroxide rather than antibiotic pastes has been suggested due to the cytotoxicity of the pastes to the stem cells of the apical papilla.57 Alternatively, antibiotic pastes should be used at 1000-fold lower concentrations of 0.1–1 mg/mL than advocated in the original pasty slurry.62 However, antibiotic pastes negatively influenced the release of growth factor from dentine by EDTA, whereas calcium hydroxide increased growth factor release.57, 58
Several studies and case reports have investigated the effectiveness of RET using a blood clot as scaffold.10, 11, 68 Resolution of signs and symptoms and periapical healing was achievable with a reported success rate of 91.3% according to a systematic review and meta-analysis. However continued root development was unpredictable68 and in several instances the attempt to induce bleeding in the canal were unsuccessful.69, 70 This led to the search for alternative scaffolds.
Alternative scaffolds to inducing a blood clot into the canal have included platelet-rich plasma (PRP) and platelet-rich fibrin (PRF).71, 72 The first scaffold used was the PRP where blood is sequentially centrifuged to produce a platelet concentrate. In comparison to a blood clot, it increased cell proliferation and growth factor concentration over time.73 Subsequently PRF was introduced which is prepared from blood collected in tubes and centrifuged without additives. The advantage of PRF over PRP is the prolonged release of growth factors which may have a positive impact on root development.73 It is worth noting here that patient's cooperation and parents' consent to collect blood sample might be a challenge in clinical practice when compared to inducing a blood clot. Also, a systematic review of clinical studies and clinical studies have reported that the use of PRP or PRF is not significantly superior to a blood clot in achieving further root maturation.74, 75
No significant differences were found between blood clot and injectable scaffolds in terms of healing and root development.76 Furthermore, the tissues formed inside the canal were not pulp-like tissues. Histological studies ingrowth of mineralized tissue and fibrous connective tissue into the root canal space.77
A recent systematic review and meta-analysis reported on the effect of intracanal scaffolds on the outcomes of RET. Clinical success of RET using blood clot, PRP, and PRF scaffolds ranged between 84.61%–100%, 91.66%–100%, and 77%–100% respectively. The different scaffolds did not show any statistically significant difference in clinical success, apical root closure and pulpal sensibility.78
The use of scaffolds is considered a cell-free approach. A more advanced cell-based approach involves an artificial/manufactured scaffold, these include stem cells and growth factors.4, 7 The superiority of using artificial scaffolds compared to blood clot induction is not reported in the literature yet and faces commercial and laboratory challenges.7
7 OUTCOME MEASURES
The degree of success of RET is considered by the extent it achieves the goals of RET which are classified as primary, secondary, and tertiary goals. Primary goal: the elimination of signs and symptoms and the evidence of radiographic bony healing. Secondary goal: increased root wall thickness and/or increased root length, (desirable, but perhaps not essential) and the Tertiary goal: positive response to sensibility testing (which if achieved, could indicate a more organized vital pulp tissue).20
The primary goals of RET are reliably achieved due to the stringent disinfection technique.1
However, based on the available evidence the secondary goal of RET is unpredictable and not reliably achieved. Variable increases or no change in root length and root canal width have been reported.67, 68 A quantitative study compared changes in root length, canal width and radiographic root area (RRA) in teeth treated with RET and calcium hydroxide apexification. This study assumed a 20% change in root dimension as “clinically meaningful” and reported no significant differences between the two procedures. Overall, only 27% (4/15) of teeth treated with RET showed clinically meaningful change in the three parameters.79 Another study of 17 traumatized teeth treated with RET reported 13.75% change in root width and 9.51% increase in root length.80 This study therefore did not meet the arbitrary 20% clinically meaningful success. On the contrary, a more recent study of 22 traumatized incisors reported 15.75 ± 12.44% increase in root length, 35.2 ± 23.31% increase in root width and 50.68 ± 32.38% decrease in apical diameter.81 Thus showing variability among studies in achieving root maturation and where potentially meaningful changes in root dimension are not achieved. Furthermore, it is unknown whether increases in root maturation strengthen teeth against cervical root fracture (discussed later in Section 18).
The restoration of pulp sensibility/vitality is the tertiary goal of RET.14 It is a clinician and scientist-based outcome that is desirable to achieve, since it may reflect the presence of a tissue that supports the sensory and defensive functions of a healthy pulp.3, 23 Kim et al. report a positive response to pulp sensibility test shows the regenerated/repaired tissue is vascularized and innervated and does not necessarily indicate regenerated pulp tissue.4 Studies have reported a vital response in a range of 35.1%–81.3%.51, 54, 82 A response to pulp sensibility testing was also associated with greater root maturation as measured by the increase in radiographic root area.83
8 REGENERATION VERSUS REPAIR
Regeneration is defined as the restoration of tissue architecture and biological function of damaged tissues by a tissue comparable to the original tissue.84, 85 Repair is replacement of damaged tissue by a tissue different from the original tissue with subsequent loss of biological function.84, 85 Histologic analysis for teeth that received RET has shown that the newly mineralized tissue deposited on the root canal walls is cementum-like or bone-like tissue, and therefore it is a repair tissue rather than true regeneration.77, 86-90 Even though, an editorial in the International Endodontic Journal in 2019 advocated that RET should consider this repair response as a positive outcome and drew comparisons with medicine where repair is more widely accepted.91
9 DOES THE ETIOLOGY OF PULP NECROSIS MATTER IN RET?
The etiology of pulp necrosis in immature teeth treated with RET varies among studies. For premolars, dens evaginates is the most common predisposing factor, with pulp necrosis occurring due to bacterial invasion through the fractured tubercle into the pulp cavity. This is likely to be a longer standing infection than in teeth with an etiology of trauma. In immature anterior teeth the most common cause is dental trauma or the anomaly dens invaginatus in the upper lateral incisor.
Pulp necrosis and infection in trauma cases is usually the result of bacterial invasion, either directly through an exposed pulp after complicated crown fracture, or indirectly through the exposed dentinal tubules in noncomplicated crown fractures, or from a lacerated periodontal ligament and damaged cementum into an avascular coronal part of the pulp.
Dental trauma as etiology of pulp necrosis has been reported as a negative prognostic factor for RET.40, 81, 92 The variations in the extent of root canal calcific changes in traumatized immature teeth with a necrotic pulp and treated with RET may be a consequence of damage to the Hertwig's epithelial root sheath (HERS), and the resultant interactions with mesenchymal stem cells in the dental follicle.93 Considering that HERS regulates root maturation, the potential for further root maturation might be inconsistent depending on the degree of damage to HERS which is directly related to the severity of the traumatic injury.
In the study by Alobaid et al the lower success rate for RET compared to apexification was explained by the higher number of traumatized teeth in the RET cohort. These authors also noted that more severe trauma cases were treated with RET than in the apexification group.79 In another study, RET had a higher success rate than apexification since their RET cohort contained smaller number of traumatized teeth compared to the apexification group.94 In a retrospective study, Zeng et al reported on the negative effect of trauma on root development after RET using a triple antibiotic paste as a medicament and blood clot as a scaffold.92 They included 116 teeth, the overall success rate in terms of clinical and radiographic healing was 99.1% at 1 year follow up. The overall rate of root maturation after RET was 89.7%. There were significant differences between the different etiological basis for pulp necrosis; the dens evaginates group had a higher rate (98.8%) of further root maturation compared to the trauma group (67.6%). Similar results were reported by other studies.40, 81
In a subsequent multicenter retrospective clinical study on the outcome of RET in immature necrotic teeth, Chrepa et al reported that etiology was a significant predictor of failure as well as root development.83 They included 51 teeth, dental trauma was the etiology of pulp necrosis in 70.7% of the treated teeth, they reported 84% success rate and 94% further root maturation over a follow-up of 2 years. The distribution of the eight failed cases were three with dens evaginatus, three with dental trauma and two with caries. Considering the small sample size, it is hard to draw relevant conclusions from this study.
Considering the primary outcome after RET in relation to the etiology of pulp necrosis, a systematic review and meta-analysis reported that there was no evidence of a difference in etiology for the outcomes of RET. A total of 445 teeth were included, the overall success rate with an etiology of trauma in terms of resolution of signs and symptoms was 94.8% (274 teeth), an etiology of a dens invaginatus was 93.1% (95 teeth) and an etiology of caries was 96% (24 teeth) with no significant differences between the three groups.95 However, this review did not analyze the secondary or tertiary outcomes in relation to the etiology of pulp necrosis.
However, Cheng et al. in a study of 62 teeth followed for a mean of 22.3 months treated with RET reported different injury types varies outcome depending on the extent of the damage to the periodontal ligament cells and apical papilla. The highest success rate was teeth with fracture (84.6%) followed by luxation (83.3%) and combined injuries (78.6%). Teeth suffering avulsion had the lowest success rate (33.3%) and survival rate (66.7%). However, there was no significant difference in the success and survival rates among the other different injury types.96
Unfortunately, avulsed and replanted teeth with immature teeth treated with calcium hydroxide apexification can also have poor outcomes with 40%–50% of teeth lost in a landmark study.35
Prospective clinical trials with large sample sizes and specification of the severity and type of the traumatic injury are needed to reveal the true association of the etiology of pulp necrosis on the outcome of RET.
10 OUTCOME STUDIES ON RET
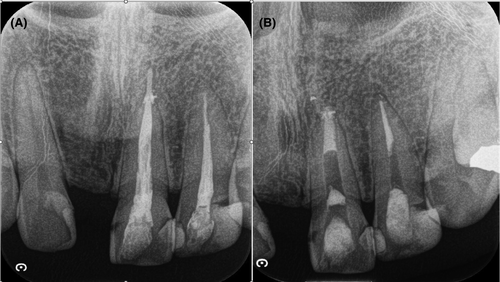
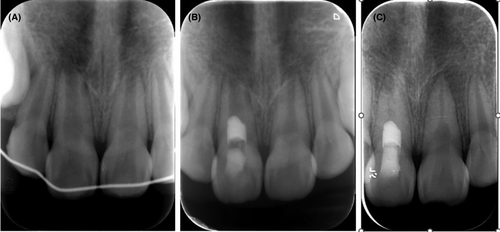
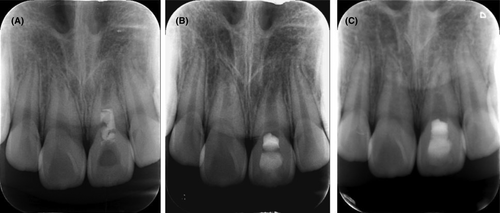
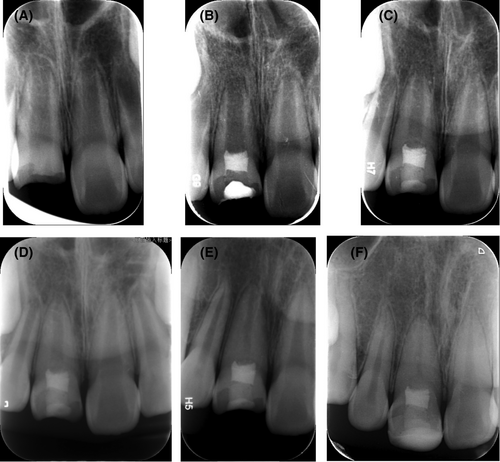
A summary of outcome studies on teeth that sustained dental trauma and were treated with RET is presented in Table 1. Examples of traumatized teeth treated with RET are shown in Figures 2-5. Studies that compared RET and apexification are presented in Table 2. An analysis of these studies attests to the efficacy of RET as a viable alternative to apexification in the treatment of immature teeth with pulp necrosis and apical periodontitis. A recent systematic review and meta-analysis reported high survival and success rates of 93.8% and 88.3% respectively in the treatment of traumatized immature teeth.106 However, the increase in root width is more reliably achieved than the increases in root length. The key concern though is whether these increases in root width and length are clinically meaningful?
| First author | Teeth | Age (years) | Trauma | Medicament | Scaffold | Barrier | Outcome % | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|
| Saoud et al.97 | 20 | 11.3 ± 1.9 |
CCF 80 UCF 10 Luxation 10 |
TAP | BC | MTA |
55% complete apical closure Only 45% of teeth met criteria of >20% increase in root width |
12 |
| Nagata et al.98 |
12 11 |
7–17 |
Lateral luxation 47.8 Extrusion 39.1 Intrusion 4.3 Avulsion 8.7 |
TAP CHX |
BC | MTA |
↑ RL 41.7% ↑ RL 27.3% Discoloration TAP group 83.3 |
9–19 |
| Ulusoy et al.75 | 88 | 8–11 | CCF 100 | TAP | PRP, PRF, PP, BC | WMTA |
73.9% Complete Apical Closure Radiographic Canal Area sig > in BC group 86% vitality for all teeth |
28.25 ± 1.2 |
| Nazzal et al.99 |
6–16 Mean 8.3 |
CF 80 Avulsion 13.3 Intrusion 6.6 |
TAP | BC | PPC |
Primary 83.8 Slow ↑ in wall width No significant change in length Rapid apical closure |
Mean 43.22 Range 27–59 | |
| Mittman et al.85 | 16 |
6–11 Average 10 |
Avulsion 75 Lateral luxation 18.75 Intrusion 6.25 |
Ledermix | BC | MTA |
81.3% survival 18.7% failed due to resorption Resorption 56.3 Ankylosis 31.3 Discoloration 92.9 Maintained bone level 85.7 |
Mean 22 |
| Rizk et al.100 | 25 | 9.08 ± 1.16 |
CCF 53.8 UCF 46.2 |
TAP |
PRP PRF |
MTA |
Primary goal 100% Secondary goal No sig diff but only marginal increases PRF Significant difference in discoloration |
12 |
| Wikström et al.*101 | 75 | UCCF 73 |
CF + luxaton 55.7 Lat lux 39% Avulsion/Intrusion 23 |
Not stated | BC |
WMTA Biodentine Endosequence |
Healed 60% Failure 14.7% Failure To Bleed 25.3% |
24–52 |
| Cerqueira-Neto et al.102 | 20 | 10.2 ± 2.62 |
CF + Luxation 63.6 CF 9.2 Luxation 18.2 Avulsion 9.1 |
CH (n = 11) Single visit (n = 9) |
BC | A mix of CH/2% CHX gel and zinc oxide |
CH as a medicament vs Single visit 9.1 vs 33.3 Primary goal 91.8 vs 100 Secondary goal 45.5 vs 66.7 Tertiary goal 9.1 vs 33.3 |
24 |
| Jayadevan et al.103 | 21 | 16.8 ± 4.28 | All trauma but type not known | TAP |
A-PRF PRF |
Biodentine |
Survival 78.5% Survival 77.5% Both groups reported significant differences in increases in root length and canal width |
14 ± 1.61 13.45 ± 1.89 |
| Cheng et al.96 | 62 | 8.6 ± 1.4 |
UCF 22.6 CCF 40.3 Luxation 9.8 CF+ luxation 22.5 Avulsion 4.8 |
TAP CH |
BC CGF |
WMTA |
Healed 80.6% BC significantly reduced risk for failure than CGF |
Mean 22.3 |
- Abbreviations: A-PRF, advanced platelet-rich fibrin; BC, blood clot; CCF, complicated crown fracture; CGF, concentrated growth factor; CHX, chlorhexidine; MTA, mineral trioxide aggregate; PP, platelet pellet; PRF, platelet-rich fibrin; PRP, platelet-rich plasma; TAP, triple antibiotic paste; UCF uncomplicated crown fracture.
| Author | Teeth | Trauma | Follow-up (months) | CH | MTA | RET |
|---|---|---|---|---|---|---|
| Jeeruphan et al.94 |
20 19 22 |
RET 35 MTA 57.89 CH 81.82 |
12.9 ± 5.07 14.6 ± 6.17 27.32 ± 30.47 |
Healed 77.27 Failed 22.73 |
Healed 68.42 Healing 26.31 Failed 5.26 |
Healed 80 Healing 20 |
| Alobaid et al.79 |
19 RET 12 Apexification* |
79% with 59% severe trauma 75% with 13% severe trauma |
17 | - |
100 Adverse event 1 |
100 Adverse events 8 |
| Silujjai et al.80 |
29 RET 17 MTA |
29.41 57.69 |
60 60 |
- |
Healed 80.77 |
Healed 76.47 ↑Root width 13.75 |
| Lin et al.40 |
21 RET 13 CH Apex |
30.43 38.23 |
12 12 |
Healed 100 ↑RL 26.47 ↑RW 0 AC 82.35 |
Healed 100 ↑RL 82.60 ↑RW 81.16 Apical closure 65.21 |
|
| Pereira et al.104 |
22 22 |
AP v RET CF 4.55v 0 Luxation 31.82v22.73 Comb CF + L 54.55v63.64 Avulsion 9.09v13.64 |
Min 12 |
Healed 86.36 RR 9.09 |
Healed 95.45 RR 31.82 |
|
| Casey et al.105 |
93REPs 89 MTA 29 CH |
75.3 Comb Apex 78 |
33.6 31.1 31.1 |
86.2 |
88.1 |
76.3 |
- Note: Jeeruphan et al. included 35% trauma cases in the RET cohort, 57.9% in the MTA cohort and 81.8% in the calcium hydroxide apexification cohort. Alobaid et al, included 94.7% of trauma cases in the RET cohort and 75% trauma cases in the apexification cohort. Silujjai et al. included 57.7% of trauma cases in MTA and 29.4% of trauma cases in RET. Casey et al consisted of 75.3% trauma cases in RET and 78% trauma in apexification.
- Abbreviations: AC, apical closure; CH, calcium hydroxide; MTA, mineral trioxide aggregate; RET, regenerative endodontic treatment; ↑RL, increase in root length; RR, root resorption; ↑RW, increase in root width.
- * In Alobaid et al, the Apexification group included 7 teeth treated with calcium hydroxide and 5 teeth treated with MTA apical barrier technique with both groups consolidated to reach the 12 teeth treated with apexification and MTA barriers.
Alobaid et al. assumed that a 20% increase in radiographic root area could be considered clinically meaningful with only 3/15 teeth (20%) meeting this threshold.79 Ong et al. in a systematic review and meta-analysis of 11 studies assessing root length, root width and apical closure reported changes as 77.3%, 90.6% and 79.1% respectively.107 However, when the 20% threshold was applied only 16.1% and 39.8% of teeth met these criteria. Other studies also reported that neither apexification or RET provided reliable changes in further root maturation.80 Further, prospective clinical studies comparing apexification and RET are required.
11 RET AND ROOT RESORPTION
Beside pulp necrosis, traumatic injuries to immature and mature permanent teeth can cause other types of pathological conditions, such as external inflammatory root resorption (EIRR), internal root resorption and root fracture. The conventional management of teeth with inflammatory root resorption that is accepted by the IADT guidelines is long-term dressing with calcium hydroxide.37 With the aim of utilizing the antibacterial and anticlastic properties of the calcium hydroxide. Therefore, it is expected that the stringent disinfection protocols of RETs would arrest EIRR.
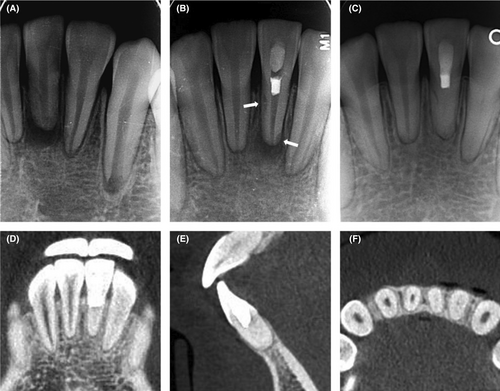
Traumatized teeth with external infection related root resorption were shown to be managed with REPs resulting in resolution of apical periodontitis and arrest of external root resorption.108-115 An example of a replanted avulsion tooth with EIRR treated with RET is displayed in Figure 6.
A recent review on the use of RETs in teeth diagnosed with external inflammatory root resorption reported biological repair and good prognosis following dental trauma.116 These studies suggest that outcomes after RET may be expanded from a clinical perspective beyond the primary, secondary, and tertiary outcome goals. Further research is required.
12 RADIOGRAPHIC RESPONSES OF TEETH TREATED WITH REPs
- Type 1, increased thickening of the canal walls and continued root maturation;
- Type 2, no significant continuation of root development with the root apex becoming blunt and closed;
- Type 3, continued root development with the apical foramen remaining open;
- Type 4, severe calcification (obliteration) of the canal space;
- Type 5, a hard tissue barrier formed in the canal between the coronal MTA plug and the root apex.
These authors noted that the outcome of continued root development was not as predictable as increased thickening of the canal walls.
Other radiographic responses have been reported. These include ingrowth of bone and an adjacent calcific barrier in the apical third of the root, ingrowth of bone and some increase in dentine width without apical closure, no substantial change in root length or width although a calcific opacity at the apex can occur likely to be a proliferation of the Hartwig's epithelial root sheath to form some further root development and healing of the periapical lesion without apical closure and thickening of the root canal walls or any change in the root.2 These variations are consistent with the findings of Chen et al.117 where further root maturation is not predictable or consistent.
13 ADVERSE EFFECTS OF RET
Adverse effects which include discoloration and pain were reported more frequently in RET (8/19, 42%) than in calcium hydroxide and MTA apical barrier apexification (1/12, 11%).79
In RET teeth the most common cause of failure was reinfection or persistent infection, compared to root or tooth fracture in teeth treated with apexification.79, 80, 94
14 TOOTH DISCOLORATION
The appearance and pleasant esthetic of anterior teeth is of particular concern to the patients, and currently is considered as a patient centered outcome. Studies and case reports have reported discoloration after RET in the range of 44%–62% of the cases.68, 85, 118
A systematic review reported that the use of triple antibiotic paste with minocycline as an intracanal medicament, along with using MTA as an intracanal barrier over a blood clot are associated with discoloration of teeth following RET.119 Biodentine (Septodont, Saint-Maur-des-Fossés, France) Total fill putty and iRoot BP (FKG, USA) have been shown to induce less coronal discoloration in crowns of teeth when used to treat complicated crown fractures and in vital pulp therapy.120, 121
In San Antonio study the incidence of tooth discoloration was high (29/47 teeth, 62%). Teeth where MTA was the coronal plug had 97% discoloration rate. Furthermore the MTA treated teeth were 21 times more prone to discoloration when compared to cases treated with Biodentine regardless of the intracanal medicament used.83 The use of double antibiotic paste or calcium hydroxide as intracanal medicament is advised to avoid discoloration, and care should be taken to limit the extension of the coronal plug placed over the blood clot to a level below the cemento enamel junction.
Intracoronal bleaching using sodium perborate has been shown to be effective in treating discoloration post RET.122, 123 An example of a tooth that discolored after treatment with RET and successfully bleached is shown in Figure 7.
15 INTRACANAL CALCIFICATION
Intracanal calcifications have been reported after RET, with variable calcification patterns from calcific barrier to canal obliteration. An example of an avulsed tooth treated with RET that developed extensive intracanal calcification is shown in Figure 6.
In a study of 29 teeth, RET associated intracanal calcification was observed in (18/29 teeth, 62.1%).124 These constituted a calcific barrier (5/18 teeth, 27.8%) and canal obliteration (13/18 teeth, 72.2%). There was a higher frequency of intracanal calcification in teeth with induced bleeding (16/23 teeth, 69.6%), compared to teeth without bleeding (6/18 teeth, 33.4%). Also, calcification occurred more frequently in teeth medicated with calcium hydroxide (10/13 teeth, 76.9%) when compared to teeth medicated with antibiotic pastes (6/13teeth, 46.2%).124
A systematic review and metanalysis was conducted on intracanal calcification after RET and its relation to the type of intracanal medicament.125 Eight studies were included and reported an overall prevalence of 30.7%. Teeth medicated with calcium hydroxide had 46.5% compared to 25.8% for teeth medicated with antibiotic pastes. Similarly, the complete canal obliteration was higher in cases treated with calcium hydroxide. In a recent study, the incidence of intracanal calcification was 10.9% (6/55 teeth) However, these cases included traumatized teeth and teeth with developmental malformations.81
Therefore, predisposing factors for revascularization associated intracanal calcification may include the type of intracanal medicament and whether intracanal bleeding was induced. While intracanal calcification does not affect resolution of apical periodontitis, it does not indicate achievement of the secondary or tertiary goals. Furthermore, complete obliteration will make future endodontic treatment if necessary more challenging.
16 TREATMENT FAILURE
Like any endodontic procedure the success rate of RET is not 100%. In RET teeth the most common cause of failure was reinfection/ persistent infection.79
RET relies on both stringent disinfection and the regenerative capacity of the stem cells of the apical papilla. It has been suggested that failure in RET may be attributed to the use of low concentrations of NaOCl irrigation in an attempt to preserve the stemness of the apical tissues.126
Not surprisingly, a study investigated the microbiome changes following a calcium hydroxide apexification protocol (5.25%–6% NaOCl +17% EDTA) and two RET protocols with different concentration of sodium hypochlorite and antibiotic pastes (1.25% NaOCl, 17% EDTA, and 0.1 mg/mL TAP) and RET (5.25% NaOCl, saline and 1 g/mL TAP).127 It showed that the apexification and RET group utilizing higher disinfection protocols had significantly less residual microbial DNA as assessed by quantitative polymerase chain reaction analysis.127
There are considerable challenges involving disinfection in RET. This balance between disinfection and regenerative induction may become more important when RETs are more broadly adapted into mature teeth with potentially more complex root canal morphology. This is a vexing question as the presence of residual bacteria is known to impact on the outcomes of RET.128 A systematic review of failed cases reported that 79% of failed RET cases were associated with persistent infection. While 63% of the failed RET cases were identified at the 1-year review, the other 37% were identified after more than 2 years follow up and generally associated with persistent infection.129
Failures of teeth treated by REP can also be related to the actual trauma especially avulsion injuries where external replacement root resorption of the root may occur regardless of the type of treatment undertaken as damage has occurred to the periodontal attachment apparatus. Coronal leakage has also been reported as an etiology for failure.129
Failed cases can be treated either with repeat RET or with conventional approaches such as, apexification, apical plug, conventional RCT, apical surgery or extraction.130 Almutaairi et al reported retreatment of failed cases; via the use of MTA in 17 cases (25%), nonsurgical root canal treatment in 11 cases (16%), extraction in 8 cases (12%), another RET in 3 cases (5%), and calcium hydroxide apexification in 2 cases (3%).129
17 REGENERATIVE ENDODONTIC TREATMENT AND ORTHODONTIC MANAGEMENT
Inadequate lip coverage and increased overjet are associated with a higher incidence of dental trauma.131, 132 It is therefore not surprising that traumatized teeth have been treated with RET and orthodontic treatment. Successful cases have been reported and lighter acting orthodontic forces were recommended.133, 134 However other reports showed late long-term complications of severe external invasive cervical resorption, pulp necrosis and internal tunneling resorption.135 Further research is required on this topic.
18 DOES RET STRENGTHEN TEETH?
The literature is inconclusive on the effect of restorative materials and adhesive approaches on the fracture resistance of immature teeth, being mainly based on in vitro experimental studies that may not necessarily reflect the clinical conditions. An in vitro study investigated the fracture resistance of immature teeth treated with five different restorative scenarios. (1) Apexification with composite resin in the crown; (2) Apexification with composite resin in the crown and 3 mm into the root; (3) Immediate revascularization with composite resin in the crown; (4) Successful revascularization with composite resin in the crown; and (5) Control: a mature tooth treated with gutta-percha and sealer and restored with composite resin in the crown. There was no statistical difference in the fracture resistance for the five restorative scenarios.136
While several experimental studies have shown that the use of fiber posts following apexification increases the fracture resistance.137-141 A retrospective clinical study reported no significant difference in the fracture rate of teeth that had MTA apexification and restored with reinforced or non-reinforced techniques over an average of 30 months follow-up.142 The incidence of root fracture in the teeth restored with the reinforced materials was 5.5%, and for the nonreinforced materials (8.3%) which was not statistically significant. The two significant predisposing factors affecting the incidence of root fracture were preoperative external inflammatory root resorption and when the patient was older than 15 years.
The cervical third of the root is known as the area of weakness for traumatized immature teeth and poses the risk of transverse root fractures in immature teeth.39 The clear disadvantage in the RET protocol is the placement of a HCSC as a 3 mm intracanal barrier in the cervical third of the root canal. This barrier prevents penetration of the regenerated tissues and therefore further root maturation in the cervical third.68 This prevents achievement of the goal of strengthening the immature root via RET in the area of the root most susceptible to fracture. However, neither calcium hydroxide apexification, apical barrier techniques or RET strengthen immature teeth in the cervical third of the root.
An immune-fluorescence histological study of a tooth successfully treated with RET showed that nonmineralized tissue interlocked with preexisting dentinal tubules. This attachment was loose in places with the hair-like projections disassociated from the preexisting dentine and not intimately adapted. This loose adaptation of the old and new tissue also contained necrotic debris. Furthermore, and consistent with other studies, the revitalized tissue was repair rather than regenerated dentinal tubules.143 The authors suggested that these projections may lack the required strength to increase the fracture resistance of the root as the newly formed mineralized tissue appeared to dissociate easily from the canal walls. This loose association of the de novo mineralized tissue has not been observed in other histological studies.77, 86-90 However, apposition of cementoid into the intracanal space may not significantly strengthen the root of the tooth.
Furthermore, several studies have shown that there is minimal increase in the canal wall thickness leaving dentinal walls thin and susceptible to fracture.68, 79 Indeed, teeth treated with RET have sustained transverse root fractures.109, 110 Further research on the long-term survival of RET treated teeth is required.
19 EFFICACY OF TREATMENT CHOICES
Several studies and two systematic reviews have shown that apexification and RET offer comparable clinical outcomes for treatment of traumatized immature teeth.40, 80, 103, 144, 145 Generally, RET was associated with some increase in thickness of the canal wall.
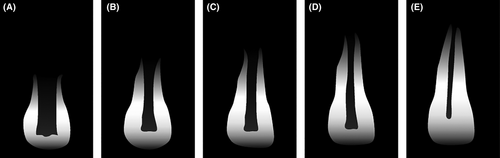
Kim et al. suggested that RET should be considered for teeth with Cvek 1–3 incomplete root formation (Figure 8), since any further increase in canal wall thickness or root development will be beneficial (Figures 4,5). In comparison teeth with near or complete root formation (Cvek 4 and 5) may be treated with RET (Figures 2,3), MTA barrier techniques or conventional endodontic therapy.

Unfortunately, teeth with incomplete root maturation treated with RET are still more often associated with unfavorable outcomes. A study of 159 traumatized maxillary incisors reported the 61 teeth treated with RET had poorer outcomes than teeth treated with apexification or pulpotomy. In this study teeth with less than ¾ of root development were treated with RET with 63.8% of the RET teeth reporting either pulp necrosis, partial canal obliteration no apical closure or ingrowth of bone.146 Unfortunately, the treatment of teeth with very immature development is often associated with poor outcomes.
20 CONCLUSIONS
RET reliably achieves resolution of the signs and symptoms of pulp necrosis and apical periodontitis in traumatized immature teeth with apical periodontitis. The greatest concern related to RET is the failure to reliably achieve a clinically significant increase in root maturation as measured by an increase in root width and root length. Furthermore, the initial concerns voiced at the early adoption of RET remain and primarily relate to repair of pulp tissue rather than true regeneration of the pulp-dentine complex and lack of evidence on the root strengthening effect of RET.
However, RET has been employed as a biologically-based treatment for traumatized permanent teeth with apical periodontitis for nearly two decades and has achieved comparable success rates to traditional mechanistic approaches. RET appears advantageous for treatment of immature teeth with Cvek 1–3 root development whereas Cvek 4 and 5 can be treated in a timelier fashion with apical barrier techniques or conventional root canal treatment. However, the treatment of immature teeth with Cvek 1–3 root maturation especially after an avulsion and replantation remains a clinical challenge often associated with poor outcomes.
AUTHOR CONTRIBUTIONS
Bill Kahler: Conceptualisation, Investigation, clinical cases, Methodology, formal analysis, Writing–original draft, Writing–review & editing. Jing Lu: Conceptualisation, clinical cases, methodology, writing. Nessrin Taha: Conceptualisation, Methodology, writing, reviewing, editing, formal analysis.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts to declare.
Open Research
DATA AVAILABILITY STATEMENT
No data.