Influence of social networks on cancer survivors' self-management support: A mixed methods study
Funding information: Health Education England (HEE)/National Institute for Health Research (NIHR), Grant/Award Number: NIHR CDRF-2013-04-029; St. Bartholomew's League of Nurses
Abstract
Objective
The role of social networks, especially weaker ties (e.g. casual acquaintances and hobby groups), in self-management of long-term consequences of cancer is unexplored. This study aimed to explore the structure of cancer survivors' social networks and their contribution to self-management support and health-related quality of life (HRQoL).
Methods
The study used a sequential, exploratory mixed methods design. Phase 1 surveyed 349 lymphoma, colorectal, breast and prostate cancer survivors. Phase 2 analysed 20 semi-structured interviews with respondents recruited from Phase 1.
Results
Phase 1 results suggested participants' HRQoL increased if they participated in an exercise group, if their self-management skills increased, and social distress and negative illness perception decreased (p < 0.0005 adj. R2 = 0.631). These findings were explored in Phase 2, identifying underlying mechanisms. Four themes were identified: disrupted networks after cancer treatment; navigating formal support and building individual capacity; peer networks and self-management knowledge and linking networks to enable adaptation in recovery.
Conclusions
This study suggests engagement with community groups, particularly those not directly related to illness management and social interaction with weak ties, make a valuable contribution to self-management support, increase HRQoL and enhance well-being.
1 INTRODUCTION
The role that social networks and connections play in shaping a person's behaviour and subsequent impact on health and well-being is increasingly recognised. Seminal studies demonstrated relationships between increased social engagement and reductions in mortality and morbidity (Berkman & Syme, 1979; Christakis & Fowler, 2007; House et al., 1988). The influence of social networks on self-management support for long-term conditions, such as diabetes, suggests that having a diverse network increases social connectedness and satisfaction with current networks and associated with enhanced self-management skills, physical and mental well-being (Vassilev et al., 2016). This may in part be due to diverse social networks providing greater access to informal practical resources (Kroenke et al., 2013). However, larger social networks and networks including different types of relationships can also require higher levels of relationship management (Vassilev et al., 2019) and be emotionally burdensome to manage. This indicates that the underlying mechanisms through which social networks operate are complex and that networks may have negative, as well as positive, impacts on health and quality of life (Cheng et al., 2013; Hamilton et al., 2010; Vassilev et al., 2016).
Previous cancer social network studies, largely undertaken in women with breast cancer, have found associations between increased network size, overall survival and cancer survival (Beasley et al., 2010; Jones & Storksdieck, 2019; Kroenke et al., 2006, 2017; Lindstrom & Rosvall, 2019; Sarma et al., 2018; Waxler-Morrison et al., 1991). Other studies have identified relationships between higher levels of social network engagement and higher HRQoL (Cheng et al., 2013; Kroenke et al., 2013; Lim & Zebrack, 2006; Soares et al., 2013), lower inflammatory markers and depressive symptoms (Hughes et al., 2014), increased exercise engagement (Kim et al., 2015) and increased support for healthy eating (Crookes et al., 2016). Social support has been found to be valuable in self-management, but there is limited research exploring network characteristics or utilising social network approaches and theories (Balfe et al., 2017; Henshall et al., 2018; Kim et al., 2020; Paterson et al., 2015). Few studies have examined how Socio-Economic Status (SES) could influence social network access to self-management resources for people with cancer or long-term conditions (Juárez-Ramírez et al., 2015; Reeves et al., 2014).
As the incidence of those living with and beyond cancer is predicted to rise (Maddams et al., 2012), self-management support has been adopted as an approach to meet increasing health and well-being needs of cancer survivors (Batehup et al., 2017). Self-management has limitations as it frequently focuses on individual concerns, such as relapse (Fenlon et al., 2015) and does not consider how personal agency, shaped by social networks can influence self-management behaviour outcomes (Dunn et al., 2021).
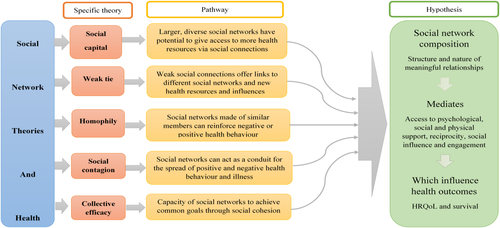
Drawing on social network theories (Figure 1), the aims of this study were to contribute towards the development of a contextualised understanding of self-management and self-management support by describing the dimensions of personal social networks (characteristics and social engagement) of cancer survivors; determining if social network dimensions and social distress are associated with health-related quality of life, exploring how social networks contribute to patients' efforts to self-manage survivorship concerns and determining if social network characteristics are associated with SES.
2 METHODS
2.1 Study design
A mixed methods design, utilising an explanatory sequential approach was chosen to address study aims and reported using GRAMMS guidelines (O'Cathain et al., 2008). Data from Phase 1, a quantitative cross-sectional survey and Phase 2, qualitative semi-structured interviews, were collected concurrently and reported using SRQR guidelines (O'Brien et al., 2014). Survey was the dominant method, its purpose to quantitatively characterise social network dimensions of cancer survivors and contribution to self-management. Phase 1 results informed analysis of Phase 2, enabling description and analysis of social network mechanisms. Ethical approval was gained from East of England Ethics Committee-Essex on 13 May 2015 reference number 15/EE/0137.
2.2 Participants and procedures
Participants were recruited from five NHS Trusts in England between August 2015 and June 2016, while attending hospital appointments or approached by post, following identification through hospital databases. Participants completing Phase 1 were invited to participate in Phase 2.
Respondents were 18 years or older, diagnosed and received primary treatment for breast, bowel, prostate cancer, non-Hodgkin's or Hodgkin's lymphoma and remained disease free (maximum 24 months since diagnosis). Research nurses identified and recruited survey participants. Principal investigator (G. H. J.) received survey responses and recruited interview participants.
2.3 Phase 1: Survey
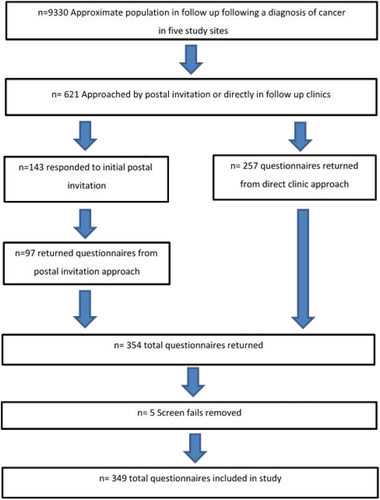
Over 11 months 621 participants meeting the eligibility criteria were approached across 5 Trusts, with 349 consenting to Phase 1 of the study, eliciting a 56% response rate (Burns & Grove, 2003) (Figure 2). The survey consisted of five components:
2.4 Health related quality of life
HRQoL data were collected using the Functional Assessment of Cancer Therapy-General (FACT-G) (Cella et al., 1993) because it is generalisable to all people with a cancer diagnosis.
2.5 Participant social engagement and characteristics
Demographic data were collected on cancer diagnosis and treatment. SES was determined using the Indices of Multiple Deprivation, derived from participants' postcode (Gov.uk, 2015). Engagement in social activity data, for example, recreation, were collected using a section from a questionnaire developed by Vassilev et al. (2013) and previously used with participants with long-term conditions. Face validity was gained through Patient and Public Involvement (PPI) review and pilot study (Table 1).
| Characteristics | Total number | Breast number | Prostate number | Lymphoma number | Colorectal number |
|---|---|---|---|---|---|
| Age | |||||
| Years (mean) | 62.91 | 57.9 | 70.7 | 59.2 | 68.3 |
| Gender | |||||
| Female | 195 | 138 | 0 | 39 | 19 |
| Male | 151 | 0 | 80 | 36 | 35 |
| Missing | 3 | ||||
| Ethnicity | |||||
| White | 341 | 134 | 81 | 72 | 54 |
| Marital status | |||||
| Married/civil partner | 250 | 96 | 63 | 51 | 40 |
| Divorced or widowed | 74 | 23 | 14 | 15 | 10 |
| Never married | 26 | 13 | 3 | 7 | 3 |
| Education attained | |||||
| No qualifications | 53 | 21 | 13 | 11 | 8 |
| School cert/GCE/O level | 217 | 89 | 46 | 54 | 28 |
| A levels | 102 | 40 | 25 | 21 | 16 |
| Vocational | 255 | 99 | 59 | 49 | 46 |
| Degree | 110 | 45 | 22 | 26 | 17 |
| Working status | |||||
| Employment | 134 | 69 | 12 | 29 | 22 |
| Long-term sickness | 14 | 6 | 1 | 4 | 1 |
| Looking after home/family | 24 | 11 | 1 | 6 | 4 |
| Voluntary work | 24 | 7 | 11 | 3 | 1 |
| Education | 4 | 0 | 0 | 2 | 0 |
| Retired | 183 | 49 | 66 | 35 | 30 |
| None of above | 12 | 5 | 1 | 4 | 0 |
| Tenure | |||||
| Owns/mortgage | 300 | 118 | 71 | 65 | 49 |
| Rents | 45 | 20 | 9 | 9 | 4 |
2.6 Social network characteristics
A social network assessment tool was developed based on the name generator approach (Vassilev et al., 2013). Participants identified all members of their social network by name, describing their relationship to them (e.g. ‘Sarah’ and ‘work friend’). Participants scored each member's contribution to their self-management support (0 = never to 5 = a lot) in three domains: illness work (e.g. managing medication), day to day work (e.g. housework) and emotional work (e.g. someone to talk to about worries) and indicated how close members lived to them, for example, a short walk. Face validity was achieved through PPI review and pilot study.
2.7 Self-management
Data were collected using subsection 4 ‘self-monitoring and insight’ and 6 ‘skill and technique acquisition’ from the Health Education Impact Questionnaire (HEIQ) (Osborne et al., 2007), previously validated in cancer populations (Maunsell et al., 2014).
2.8 Social distress
Data were collected using the Brief Illness Perception Questionnaire (BPIQ) (Broadbent et al., 2006), adapted with permission for use in a cancer population. Face validity was gained through feedback from PPI group and pilot study. Cronbach's alpha was undertaken to test internal reliability. The result was 0.68, under the recommended 0.7, but lower results are acceptable within psychological constructs (Klein, 1999). Social Distress data were collected using the Social Difficulties Inventory (SDI) (Wright et al., 2011).
2.9 Statistical analyses
Descriptive statistics are used to summarise demographic and social network dimensions of the sample. Preliminary analyses were conducted to ensure there was no violation of assumptions of normality, linearity, homoscedasticity and multicollinearity. Preliminary linear regression was undertaken, followed by four multiple regression models which observed for relationships between HRQoL and participant characteristics, social network characteristics, network contribution to self-management and social distress. A final multiple regression model was undertaken with all previously significant variables. Statistical analysis was undertaken with SPSS® software, version 25.
2.10 Phase 2: Semi-structured interviews
A purposeful sample of 20 participants reflecting age, gender, disease and SES was selected for Phase 2. Interviews were recorded with consent and undertaken at participants' choice of location. The interview guide was developed from work by Reeves et al. (2014), collecting narrative data on participants' experiences on the role of social networks in self-management support. Sample size was considered large enough to offer meaningful analysis (Kvale, 2007; Quin Patton, 2002; Tashakkori & Teddlie, 2010). Techniques to enhance trustworthiness of data collection were addressed by (R. A.) and (I. V.) critically reviewing a sample of interview recordings (Lincoln & Guba, 1985). The dynamic relationship between the interviewer and interviewees was acknowledged. The interviewer kept a critical journal to reflect on each interview and minimise researcher influence (Bryman, 2016; Spradley, 1979).
2.11 Data analyses and interpretation
Interview findings were analysed deductively, using framework analysis (Gale et al., 2013). Themes identified from survey findings and informed by weak tie theory (Granovetter, 1973) were used to describe and explain how weak tie (non-familial and peripheral) social network members, social network mechanisms and SES influenced self-management support. Data were imported into the software programme NVivo 12 to facilitate analysis (Ritchie & Lewis, 2014). G. H. J. conducted the analysis; subsamples of which were independently coded by A. R. and I. V.
2.12 Data integration
Integration occurred throughout the study. The same sample of participants generated quantitative and qualitative data to explore the subject from different perspectives. Survey findings informed analysis of interview data to gain further understanding of the mechanisms that could explain observed statistical trends. Data from Phases 1 and 2 were used to address the aims of the study and key findings were used to derive a multi-faceted knowledge of the influence of social networks on cancer survivors' self-management support (Bazeley, 2018; O'Cathain et al., 2007; Teddlie & Tashakkori, 2009).
3 RESULTS
3.1 Phase 1
A total of 349 people were recruited, 56% women (n = 195) and 44% men (n = 154). Mean age was 63 years (standard deviation 13.04). Women with breast cancer were the largest diagnostic group 39% (n = 138), followed by men with prostate cancer 23% (n = 82), lymphoma 21% (n = 75) and bowel cancer 15% (n = 54). Participants were most frequently within 2–6 months of completing cancer treatment (38%; n = 131). The sample was 98% white (n = 341). Most respondents 71.6% (n = 250) were married or in a civil partnership. Educational attainment ranged from 15.1% (n = 53) having no educational attainment and 32% (n = 110) having a first degree. Most had retired 51.2% (n = 183) (Table 1).
3.1.1 What are the social network dimensions of cancer survivors?
The 349 participants identified 2,077 social network members (Table 4). Most frequently identified members were friends (26.1%; n = 546), health professionals (16.0%; n = 332) and children (15.5%; n = 322). Spouses were frequently listed (13.0%; n = 271), reflecting that most of the 349 participants were married. There were 1.7% (n = 36) pets, indicating 10% of participants listed an animal. The overall mean number of members listed in a participant's social network (network size) was 6 (SD 4.7). The overall diversity mean (different network member types, e.g. family and neighbours) was 3.6 (SD 1.8). The most commonly attended social groups (attended at least monthly) were social clubs and hobby groups (45.0%), sports and exercise groups (37.5%) and participation in volunteering groups (21.8%); 12% of participants in the study also attended religious groups or places of worship. Overall, 84.2% of participants were satisfied with their current social opportunities (Table 2).
| Relationship | Frequency | % |
|---|---|---|
| Partner | 271 | 12.9 |
| Children | 322 | 15.4 |
| Close family | 211 | 10.1 |
| Extended family | 161 | 7.7 |
| Friends | 546 | 26.1 |
| Work colleagues | 89 | 4.3 |
| Paid domestic support | 6 | 0.3 |
| Neighbours | 61 | 2.9 |
| Health professionals | 332 | 15.9 |
| Recreation group groups | 42 | 2.0 |
| Pets | 36 | 1.7 |
| Total | 2077 | 99.2 |
| Missing | 16 | 0.8 |
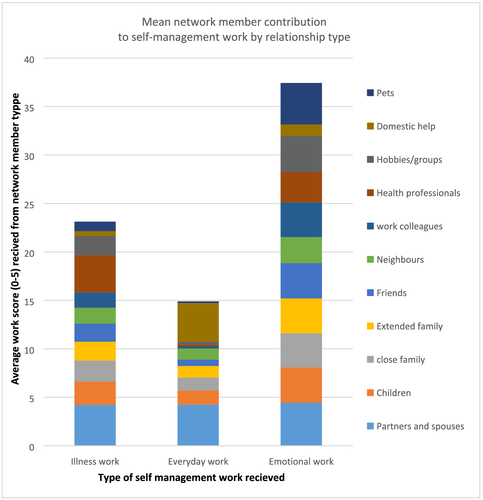
3.1.2 What is the self-management work social network members contribute to?
Across the three self-management work domains spouses contributed most to illness work (Mean [M] = 4.2), everyday work (M = 4.2) and emotional work (M = 4.4) (Figure 3). The lowest scores overall were seen in the day-to-day work domain. Domestic workers (providing childcare or cleaning) scored highest (M = 4.0) after spouses but this score was only found in the breast cancer (female) sub-group. With respect to emotional work, pets achieved the highest score (M = 4.2) after spouses, followed by hobbies and groups (M = 3.7). Within illness work, health professionals contributed the largest amount of work (M = 3.8) after spouses, followed by children (M = 2.3) (Figure 3).
3.1.3 What personal, social network and self-management dimensions influence HRQoL?
Participant characteristics explained 16.4% of the variation in HRQoL (according to the adjusted R2) F(12, 271) = 5.637, p < 0.001, adj R2 = 0.164. There was evidence supporting non-zero effects for five of the 12 variables: age; working status; time spent self-managing; self-management skills and self-management monitoring. Social network engagement explained 16.4% of the variation in HRQoL (according to the adjusted R2) F(18, 303) = 4.494, p < 0.001, adj. R2 = 0.164. There was evidence supporting non-zero effects for: satisfaction with social opportunities, weekly, monthly and less often sport/exercise participation. Network contribution to self-management characteristics did not explain variation with HRQoL, F(5, 314) = 1.785, p > 0.05 (0.116), adj. R2 = 0.012. There was evidence supporting non-zero effects for one variable, emotional work. Social distress characteristics explained 60.2% of the variation in HRQoL (according to the adjusted R2) F(2, 331) = 253.287,
p < 0.000, adj. R2 = 0.602. There was evidence supporting non-zero effects for: illness perception and social distress.
A final multiple regression model explained 63.1% of the variation in HRQoL (according to the adjusted R2) F(13, 266) = 37.757, p < 0.0005, adj. R2 = 0.631. There was evidence supporting non-zero effects for: self-management skills, sport participation (weekly, monthly and less often), social distress and illness perception p < 0.05. (Table 3).
| Variable | β | 95% CI | p-value |
|---|---|---|---|
| Age (years) | −0.117 | −0.240, −0.006 | 0.062 |
| Working status (working/retired) | −0.530 | −3.461, 2.400 | 0.722 |
| Time spent self-managing (1 to 4) | −0.259 | −1.119, 0.601 | 0.553 |
| HEIQ self-monitoring scale 4 (0 to 4) | −0.020 | −0.428, 0.389 | 0.925 |
| HEIQ skills scale 6 (0 to 4) | 0.543 | 0.001, 1.084 | 0.049* |
| Satisfaction with social opportunities (1 to 5) | −0.707 | −2.134, 720 | 0.330 |
| Sport/exercise participation weekly | 3.196 | 0.866, 5.527 | 0.007* |
| Monthly | 5.072 | 0.475, 9.670 | 0.031* |
| 3 monthly | 3.681 | −1.305,8.667 | 0.147 |
| Less often | 5.371 | 1.499, 9.964 | 0.008* |
| Contribution to emotional work by network members (0 to 5 per member) | −0.019 | −0.076, 0.039 | 0.529 |
| Social distress index (0 to 80) | −0.981 | −1.194, −0.767 | 0.001* |
| Illness perception questionnaire (0 to 44) | −0.464 | −0.559, −0.368 | 0.000* |
- * p value < .05.
Our findings indicate that wider engagement of cancer survivors with social activity and the subsequent receipt of network self-management support improves HRQoL. SES was found to be statistically significant when simple linear regression was applied. This was not the case with multiple regression, suggesting that other effects correlated with SES were more important than SES alone.
Survey findings directed analysis aims of Phase 2 of the study. Interview data enabled exploration of why membership of social network groups might contribute towards lower social distress, increased self-management and HRQoL and elicit mechanisms through which this occurred. Analysis also gave the opportunity to explore the subtle influence of SES on social networks and self-management.
3.2 Phase 2 findings
A purposeful sample of 20 participants was recruited from the 220 survey participants who expressed an interest in being interviewed (Table 4). Qualitative analysis identified four themes that illuminated mechanisms through which different types of groups influenced participants' engagement in self-management support and how SES contributed. The themes were; disrupted networks after cancer treatment, navigating formal support and building capacity, peer networks and self-management, and linking networks to enable adaptation.
| Participant number | Gender | Age | Socio economic statusa | Illness type |
|---|---|---|---|---|
| ID1 | Female | 72 | Low | Breast |
| ID2 | Female | 48 | Low | Breast |
| ID3 | Female | 67 | Low | Lymphoma |
| ID4 | Male | 72 | Low | Lymphoma |
| ID5 | Female | 44 | High | Breast |
| ID6 | Male | 52 | Low | Lymphoma |
| ID7 | Male | 74 | High | Prostate |
| ID8 | Male | 63 | Low | Bowel |
| ID9 | Female | 45 | High | Lymphoma |
| ID10 | Female | 64 | Low | Bowel |
| ID11 | Female | 58 | Low | Lymphoma |
| ID12 | Male | 74 | Low | Prostate |
| ID13 | Male | 69 | High | Bowel |
| ID14 | Male | 81 | Low | Bowel |
| ID15 | Male | 32 | High | Lymphoma |
| ID16 | Female | 82 | Low | Breast |
| ID17 | Male | 70 | Low | Prostate |
| ID18 | Female | 67 | Low | Bowel |
| ID19 | Female | 67 | High | Bowel |
| ID20 | Male | 64 | Low | Prostate |
- a Socio-ecconomic status was defined using postcode and Indices of Multiple Deprivation (IMD), range 1 to 10, 1 most deprived, 10 least deprived. Participants with IMD 1-5 classified as having low SES and IMD 6-10 as high SES.
3.2.1 Disrupted networks after cancer treatment
Participants with low SES and networks observed to be dominated by family members in Phase 2, described how they consciously dropped peripheral network members during treatment and did not re-engage with them, choosing to rely only on family members. This was primarily due to the complex relationship work needed to maintain engagement across networks. Disruption to participants' social networks limited capacity to access self-management resources available from within those networks, such as emotional and practical support. At treatment completion, participants described how their previous or newly reshaped social networks either contributed or prevented facilitation to navigate their re-defined network identity to promote their health.People think I'm better now and I'm not better now but everybody expects you to just be better now. That's what I find hard actually is everybody else's expectations I suppose. ID11, female, low SES
I sort of focused in and I focussed on the family because they were the ones looking after me. So when I got back home I got even smaller and it (social network) stayed basically with a small family …. I stopped socialising outside with friends or contacts I had. I chose, well I did it slowly. (ID18, female, low SES)
3.2.2 Navigating formal support and building capacity
I did not think it was something I would need, but actually it (counselling at cancer centre) was the right thing …. You cannot load on people that are close to you all the time, I needed someone who could listen to my upset. ID05, female, high SES
3.2.3 Peer networks and self-management
There's a lady at our work went through a similar thing … she told me with reference to her (bowel) symptoms because we speak together, it took her three years after her operation before she felt she was fit enough, like before the op, so I mean I can see where she is coming from now. (ID08, male, low SES)
3.2.4 Linking familiar and new networks to enable adaptation
My friend, who went to the same exercise class with me before I was ill suggested that exercise teacher might help me at home. I did not know she could do that. So the exercise teacher sees me 1:1, she has kept a slot for me, I'm very lucky. ID09, female, high SES
4 DISCUSSION
4.1 Contribution of social networks to self-management support
Our findings indicate that weak tie network groups appear to have a positive impact on self-management and HRQoL through engagement in a range of opportunities, resources and experiences, suggesting such networks could have a valuable and previously overlooked role in supporting cancer survivors' to self-manage long-term health needs.
Close family members are frequently turned to in times of acute need (Perry & Pescosolido, 2015) and our findings concur but also identified for the first time the mechanisms of how weak tie networks, such as recreational groups, informal peer networks and community cancer support services make valuable contributions to self-management and lowering social distress after treatment. The value of network groups, particularly peer support has been recognised (Dunn et al., 2003). Our paper contextualises the contribution of peer support to self-management within the wider focus of a network approach, while offering some insights as to why support groups may not work for all and the importance of other weak tie networks.
4.2 Network membership, socio-economic status and self-management support
Our findings suggest that characteristics of network membership, such as diversity, appeared to have more influence on ability to engage with network self-management opportunities and that lower SES alone was not prohibitive of network group engagement. Phase 2 findings revealed that participants whose networks were dominated by family members tended to have low SES. Phase 2 findings also indicated that while low SES did not appear to restrict access to direct self-management support it did appear to be indirectly associated with preventing access to social resources, such as transport, limiting engagement. Participants with higher SES were less impacted by access to resources and benefited from additional resources, such as occupational health services.
Participants with lower SES and family dominated networks appeared to have limited opportunities to engage with wider self-management support and resources. This could be due to limited individual and network resources (e.g. employment flexibility) and the potential burden that self-management support could put on network members (Kroenke et al., 2013; Perry & Pescosolido, 2015; Reeves et al., 2014; Walker et al., 2018). It is possible that participants who had embedded family networks could have been satisfied with the variety of resources already provided within their network and did not feel it necessary to seek external support. The substantial emotional and identity investment people have within families can make it challenging to renegotiate these relationships and engage in new or alternative self-management resources (Vassilev et al., 2016). This is more difficult during a time of crisis when people's networks tend to shrink even though self-management and quality of life might benefit from access to larger and more diverse networks.
Acknowledging the contribution of wider social networks and understanding how relationships, positive or negative, within the context of such networks may shape one another, could potentially contribute to upscaling cancer survivorship care, bridging the gap between hospital self-management support and community social networks.
4.2.1 Methodological value
The study indicated the value of adopting a mixed method network approach to illuminate self-management support of cancer survivors. Findings suggest the influence of structural components of networks, such as size and diversity have a nuanced influence on how and why cancer survivors access or do not access resources and support, which cannot be captured and explained by only drawing on either quantitative or qualitative methods alone. Our findings also indicate that HRQoL may be too crude an outcome measure to identify the influence of social networks on cancer survivors' social distress and ability to self-manage. Utilising a well-being outcome measure in conjunction with HRQoL would give the opportunity to measure a variety of positive assets in functioning.
Findings also indicate data collection methods and measures used in the quantitative phase of the study tended to underestimate the involvement and role of weak ties in social networks and self-management support, which could reflect the value cancer survivors' put on relationships with stronger ties. The value of adopting a mixed method approach was further demonstrated as the qualitative analysis demonstrated the key role weak ties play in self-management support and quality of life is largely invisible and their value is precisely due to these links being understated by participants (Rogers et al., 2014). Developing and using measures of network engagement and support capable of capturing the role of weak ties and relationship work is likely to lead to a better understanding of the needs and experiences of cancer survivors.
4.3 Limitations
We recognise that a more robust sequential approach could have been adopted whereby results of the survey directly informed the interview schedule, and not just the analysis. Parallel data collection limited the strengths gained from adopting a mixed method design and could have impacted study findings. Participants were predominantly white (2% self-identified as BME), educated, middle income and did not reflect greater ethnic diversity or a broader SES population.
The HRQoL measure Fact-G (Cella et al., 1993) has been criticised as not reflecting the broader concerns of cancer survivors who have completed treatment (Yost et al., 2013). Future studies could consider more cancer survivor specific HRQoL measures such as the Quality of life in Adult Cancer Survivors (Avis et al., 2005). These limitations suggest the findings need to be interpreted with caution in terms of implications for the wider population.
5 CONCLUSIONS AND CLINICAL IMPLICATIONS
This study set out to explore if the dimensions of cancer survivors' personal social networks shaped self-management support and their relationship with HRQoL. Taking a mixed methods approach and drawing on social network theories, findings suggest that engagement in community groups and interactions with weak tie social network members can make a substantial contribution to self-management and improve HRQoL. This study identified the previously under-recognised contribution of social networks, especially of weak ties, in the context of self-management support for cancer survivors, and has implications for expansion of future health service delivery and improved health. Findings also illuminated some of the mechanisms through which SES and network structure could shape self-management support. Future research should consider incorporating the broader construct of well-being as well as HRQoL.
Findings suggest healthcare professionals need to recognise the wider contribution of social networks to facilitate self-management support of cancer survivors. Healthcare staff can contribute to health and well-being beyond clinical care by advocating survivors' engagement in non-clinical, community cancer services and non-cancer social interaction. Social networks are an untapped self-management resource for cancer survivors and have significant potential to improve health and well-being.
ACKNOWLEDGMENTS
Thank you to the generous contribution of all participants, lead Network Research Nurses Tracey Dobson, Elizabeth Happel, Sophia Strong-Sheldrake, Sabrina Farrugia & Melissa Williams and financial support from St. Bartholomew's League of Nurses.
CONFLICT OF INTERESTS
Gilly Howard-Jones, Clinical Doctoral Research Fellow, NIHR CDRF-2013-04-029, is funded by Health Education England (HEE)/National Institute for Health Research (NIHR) for this research project. Professor Richardson is a National Institute for Health Research (NIHR) Senior Investigator. The views expressed in this article are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The authors have no conflict of interests to declare.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




