Efficacy of long-term intralesional triamcinolone in Morbihan's disease and its possible association with mast cell infiltration
The copyright line for this article was changed on 7 September 2018 after original online publication.
Abstract
Morbihan's disease is characterized by chronic persistent facial edema of the upper half of the face, absence of typical diagnostic findings, and refractoriness to treatment. A 44-year-old man was diagnosed with Morbihan's disease based on clinical signs and histopathology, which showed dermal edema in upper dermis, discrete lymphocytic infiltrate without granulomatous reaction, and mast cell infiltration. After long-term therapy with intralesional triamcinolone a remarkable objective and subjective clinical response was observed. Reported cases of Morbihan's disease are reviewed, with respect to their treatment and histopathological findings. Mast cell infiltration has been observed on histopathology in most patients who responded to intralesional triamcinolone, suggesting a possible marker of response. The long-lasting response seen in our case indicates the efficacy of intralesional triamcinolone in this rare condition.
1 INTRODUCTION
Morbihan's disease (MD) is characterized by chronic persistent erythema and edema of the upper half of the face (Wohlrab, Lueftl, & Marsch, 2005; Balakirski, 2013; Nagasaka, Koyama, Matsumura, & Chen, 2008). Since no specific laboratory and histopathological findings exist, the diagnosis is based on clinical presentation and exclusion of various differential diagnoses such as dermatomyositis, systemic lupus erythematosus, superior vena cava obstruction, angioedema, thyroid disease, or chronic contact dermatitis (Wohlrab et al., 2005, Bechara, Jansen, Losch, Altmeyer, & Hoffmann, 2004). Moreover, the unclear underlying pathogenetic mechanisms and the refractoriness to treatment conduce to the chronic course of disease, which may impair the patient's quality of life. We present a case of MD with remarkable clinical improvement after intralesional triamcinolone treatment along with a brief review of the pathogenetic mechanisms and treatment modalities reported so far in literature.
2 CASE REPORT
A 44-year-old man noticed a persistent, asymptomatic swelling of upper and lower eyelids, which remained constant throughout the day. He had no history of rosacea, allergies, or intake of new medications and his medical history included only a schizophrenic disorder. He was initially referred to our allergology department on May 2009. The in vitro and in vivo testing as well as the additional laboratory investigations revealed no pathologies. Computer tomography of upper chest and magnet resonance tomography of brain and orbits excluded anatomic pathologies, tumor or inflow congestion. Because of the underlying psychotic disorder and therefore poor compliance, the patient was then lost to follow up until February 2016, when he presented again for consultation. He reported that he had already received long-term antibiotics (unknown regime) without improvement. In addition, he underwent a bilateral eyelid debulking in 2012 as well as in 2014 in a plastic surgery department, showing only transient improvement. Physical examination revealed marked, asymptomatic, non-pitting periorbital edema, predominantly on both lower eyelids, and no signs of rosacea (Figure 1a,b). He was diagnosed with Morbihan disease according to clinical findings. The histopathological examination showed edema in upper dermis, discrete perivascular and periadnexal lymphocytic infiltrate without granulomatous reaction and interstitial mast cells in mast cell tryptase and c-Kit staining (Figure 2). The patient was started with intralesional triamcinolone, injected in both lower eyelids on March 2016. The injections were repeated every 4 weeks (first two cycles: triamcinolone 20 mg/lidocaine 1%, 1:1; following cycles: triamcinolone 40 mg/lidocaine 1%, 1:1; 1 ml on each side) leading in subjective and objective improvement of periorbital edema within 4 months. Hence, treatment was maintained and further improvement, especially of left side, was observed (Figure 1c-d). On May 2017, treatment of left lower lid was discontinued, and no recurrence was observed to date (8 months). Injections on right side are still administered every 6 weeks. Except from slight skin discoloration no ocular side effects were reported from patient.
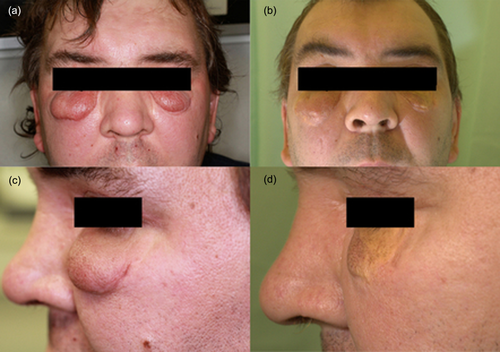
Clinical response to long-term treatment with intralesional triamcinolone: (a) marked, asymptomatic, non-pitting periorbital edema, predominantly on both lower eyelids (February 2016); (b) clinical result after 17 months of treatment (July 2017)
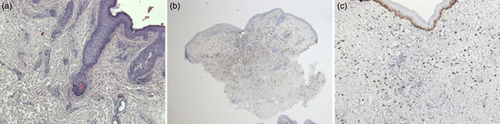
Skin biopsy from patient's lower eyelid: (a) hematoxylin–eosin staining showing edema in upper dermis, discrete perivascular and periadnexal lymphocytic infiltrate without granulomatous reaction; (b) interstitial mast cell infiltration in mast cell tryptase staining; (c) mast cell infiltration in c-Kit staining
3 DISCUSSION
Pathogenesis of MD remains ambiguous. It is likely that vascular dysregulation, fibrosis as well as obstruction of lymphatic vessels are all involved in pathophysiology of persistent facial edema and erythema (Bechara et al., 2004; Bernardini, 2000). The mechanisms of lymphatic vessel destruction may vary by inflammatory trigger, such as rosacea, acne, or immune contact urticaria, and may be reflected in the diversity of histological findings (Wohlrab et al., 2005; Smith & Cohen, 2012). Reported histological findings are summarized in Table 1. In contrast to our case, several reports state the formation of epithelioid cell granulomas around lymphatic vessels which could induce continuous lymphedema and subsequent lymphatic damage leading in formation of facial edema (Nagasaka et al., 2008). Mast cell infiltration is another common histological feature, which was also observed in our case. Fujimoto et al. stated that this finding may be associated with the disease stage and biopsy technique (Fujimoto, Mitsuru, & Tanaka, 2015).
| Year | Author | Journal | Treatment | FU | Histopathology | Rosacea |
|---|---|---|---|---|---|---|
| 1997 | Mazzatenta et al., 1997 | Br J Dermatol | Isotretinoin 0.7 mg/kg/d + Ketotifen 2 mg/d for 4 months | NA |
- Dermal edema - Hypertrophic sebaceous glands - Perivascular and periadnexal infiltrate of lymphocytes, histiocytes, plasma cells, and mast cells |
Yes |
| 2000 | Bernardini, 2000 | Ophthalmology | Debulking of lower lid mass and horizontal eyelid tightening | 3 weeks |
- Dermal edema - Dense lymphocytic infiltrate |
Yes |
| Debulking of lower lid mass and horizontal eyelid tightening | 2 weeks |
- Dermal edema - Vascular hyperplasia - Stellate fibroblast infiltration |
||||
| 2004 | Bechara et al., 2004 | J Dermatol | CO2 laser blepharoplasty and isotretinoin 20 mg/d | 6 months |
- Perivascular and perifollicular infiltrates of lymphocytes, histiocytes, and mast cells - Dilatation of lymphatic vessels |
Yes |
| 2008 | Nagasaka et al., 2008 | Clin Exp Dermatol | Minocycline 200 mg/d + tranilast 300 mg/d + prednisolone 20 mg/d | Few months |
- Dilated vascular vessels - Perivascular lymphocytic infiltrate - Focal granulomatous reaction in upper dermis - Dilated and damage of lymphatic vessels through infiltration of histiocytes in the lumens and adjacent epithelioid cell granulomas |
Yes |
| 2011 | Renieri, 2011 | Klin Monbl Augenheilkd (article in german) | Blepharoplasty + lymphatic massage | 13 months |
- Dermal edema - Fibrosis - Dilated lymphatic vessels - Perivascular lymphocytic infiltrate - Mast cells perivascular |
Yes |
| Intralesional triamcinolone + lymphatic massage | 11 months | |||||
| intralesional triamcinolone | 9 months | |||||
| Blepharoplasty + intralesional triamcinolone | 1 months | |||||
| Metronidazole + Permethrin | No response | NA | Yes | |||
| 2012 | Smith and Cohen, 2012 | Arch Dermatol | Isotretinoin 80 mg/d for 20 months | 24 months | NA | Yes |
| Isotretinoin 40 mg/d for 14 months | 7 months | |||||
| Isotretinoin 60 mg/d for 10 months | 4 months | |||||
| Isotretinoin 80 mg/d for 13 months | 1 months | |||||
| Isotretinoin 40 mg/d for 24 months | 8 months | |||||
| 2013 | Balakirski, 2013 | Hautarzt (article in german) | Isotretinoin 30 mg/d for 12 months, then 20 mg/d for 3 months | 15 months |
- Perivascular and perifollicular lymphocytic infiltrate - Dilatation of vessels - Dermal edema - Mast cell infiltrate |
Yes |
| 2015 | Fujimoto et al., 2015 | Acta Derm Venereol | Minocycline 100 mg/d for 4 months | 8 months |
- Dermal edema - Perivascular and perisebaceous mononuclear infiltrate - Granulomatous reaction in deep dermis - Fibrosis - Mast cell infiltrate in dermis |
No |
| 2015 | Kabuto et al., 2015 | J Dermatol | Minocycline 100 mg/d | 6 months |
- Dermal edema - Perivascular and perifollicular lymphocytic infiltrate - Mast cell infiltrate |
No |
| 2015 | Carruth et al., 2017 | Ophthal Plast Reconstr Surg | Debulking twice + steroid injection | 6 months |
- Dilated lymphatic vessels - Dermal edema - Sebaceous hypertrophy - Peri-infundibular infiltrate of lymphocytes, histiocytes, plasma cells, and mast cells - Perilymphatic lymphocytic infiltrate with focal histiocytes |
Yes |
| Debulking | NA | |||||
| Blepharoplasty | 6 months | |||||
| Steroid injection | 6 months | |||||
| Steroid injection | 3 months | |||||
| 2015 | Rebellato et al., 2015 | AnBras Dermatol | Isotretinoin 20 mg/d for 6 months + Ketotifen 1 mg/d for 2 months | 6 months |
- Perivascular infiltration of dermis - Dilated vessels - Mast cell infiltrate |
No |
| 2017 | Okubo et al., 2017 | J Dermatol | Doxycycline 200 mg/d for 7 months | 14 months |
- Mild lymphatic dilatation - Inflammatory cell infiltration of lymphocytes and mast cells around small blood vessels and adnexa |
No |
| Doxycycline 200 mg/d for 12 months | 10 months | -Nodular inflammatory changes in dermis around the follicles (histiocytes, mast cells, lymphocytes, multinucleated giant cells) | No | |||
| Doxycycline 200 mg/d for 9 months | 6 months |
- Dilation of lymphatic and blood vessels - Palisading granuloma - Perivascular and perilymphatic infiltrate of eosinophils, mast cells |
No | |||
| Doxycycline 200 mg/d for 5 months | 8 months |
- Perivascular lymphocytic and mast cell infiltrate - Focal granulomatous reaction in upper dermis |
Yes |
- FU, follow up; m, months; w, weeks; NA, not applicable.
Because of the rarity of MD, no controlled treatment studies have been conducted to date. Hence, its management remains mainly empirical. Furthermore, the unknown pathogenesis restricts the establishment of more targeted therapies. Treatment options reported in dermatological journals consist mostly of systemic anti-inflammatory agents, given alone or in combination (Table 1). Okubo et al. reported four cases of MD which were treated with long-term doxycycline achieving an average disease-free interval of nine months (Okubo, Takahashi, Akasaka, & Amano, 2017). All of them shared similar histopathological findings, including mast cell infiltration. On the contrary, combination therapy with minocycline and tranilast given in a patient with no presence of mast cell infiltrates in histology remained ineffective (Nagasaka et al., 2008). Promising results have been demonstrated after long-term isotretinoin monotherapy or systemic combination of isotretinoin with ketotifen (Smith & Cohen, 2012; Kabuto, Fujimoto, Honda, & Tanaka, 2015; Mazzatenta, Giorgino, Rubegni, Aloe, & Fimiani, 1997; Rebellato, Rezende, Battaglin, Lima, & Fillus Neto, 2015). Isotretinoin's mechanism of action in MD is postulated to be correlated with its anti-inflammatory and immunomodulatory properties that make it also useful in treatment of rosacea (Smith & Cohen, 2012). Other reported treatment modalities, such as systemic corticosteroids, thalidomide, or antihistamines showed no or only short-term profit (Nagasaka et al., 2008).
Invasive interventions, such as surgical debulking, have been shown to be useful in management of therapy refractory edema in MD, as seen in cases published in ophthalmological journals (Table 1). Carruth et al. reported five cases of MD managed with surgical reduction of eyelid mass with variable success. Better results were shown after combining surgery with adjunctive local anti-inflammatory therapy, such as triamcinolone injection, or after triamcinolone alone. Histopathological results were not provided (Carruth, Meyer, & Wladis, 2017). In a second case series of five MD-patients, combination of blepharoplasty and lymph drainage led to long term improvement, while triamcinolone injections alone showed also beneficial outcomes. In four of these cases, presence of mast cells and absence of granulomas were seen in histology, as in our case. However, this data is available only in German literature (Renieri, 2011). Carbon dioxide laser blepharoplasty represents another reported interventional therapy option, which led to good cosmetic results and no recurrence during the 6-month follow up period in a patient with MD (Bechara et al., 2004).
To date, there are only few reports published in ophthalmological journals, which address the efficacy of intralesional triamcinolone in treatment of MD (Carruth et al., 2017; Renieri, 2011). The presence of mast cells in tissue biopsies of these patients, like in our patient, suggests that the effectiveness of triamcinolone may be associated with mast cell infiltration. Steroids are known to suppress mast cells by inhibiting both their activation and proliferation, as described also for mucosal mast cells in inflammatory bowel disease (Paranjape et al., 2016; Kang & Kim, 2002). Additional data are provided by Paranjape et al., who demonstrated recently the inhibitory effects of dexamethasone on mast cell activation by interleukin-33, including cytokine production, migration, and neutrophil recruitment (Paranjape et al., 2016). Of major importance for the clinical outcome, seems to be the route of administration, that is, intralesional, considering the poor response of MD to systemic corticosteroids. This can be explained by the increased concentration of the anti-inflammatory agent, when applied locally, opposed to an impaired local delivery after systemic administration due to persistent lymphedema and perivascular inflammation. In a case of solid mastocytoma, another clinical entity with mast cell infiltration, clinical improvement could be reached after three intralesional injections of triamcinolone. Due to the prolonged response shown in this case the authors assumed a depletion of mast cells (Kang & Kim, 2002).
4 CONCLUSION
The present case demonstrates, to our knowledge, the longest progression-free interval after triamcinolone initiation in a patient with MD, which may be related to maintenance of therapy. Considering the adverse events of proposed systemic agents, especially if prolonged therapy is needed to reach efficacy, we postulate that long-term intralesional triamcinolone is an effective, safe and minimal invasive prospective option in the management of this refractory condition, especially when mast cell infiltration is present. Clinical studies with big cohort of patients and long-term follow up need to be conducted, to ascertain efficacy and compare different treatment modalities alone or in combination.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS
Patient obtained written informed consent for publication.




