Prediabetes and the risk of type 2 diabetes: Investigating the roles of depressive and anxiety symptoms in the Lifelines cohort study
Abstract
Aims
Depression and anxiety may increase the risk of progressing from prediabetes to type 2 diabetes. The present study examined the interactions between prediabetes status and elevated depressive and anxiety symptoms with the risk of type 2 diabetes.
Methods
Participants (N = 72,428) were adults aged 40 years and above without diabetes at baseline from the Lifelines Cohort Study (58% female; mean age = 51.4 years). The Mini-International Neuropsychiatric Interview screened for elevated symptoms of major depressive disorder and generalized anxiety disorder. Glycated haemoglobin A1c (HbA1c) levels determined prediabetes status at baseline (2007–2013), and HbA1c and self-reported diabetes diagnoses determined diabetes status at follow-up (2014–2017). Groups were formed for elevated depressive and anxiety symptoms, respectively, and prediabetes status at baseline (elevated depressive/anxiety symptoms with prediabetes, elevated depressive/anxiety symptoms alone, and prediabetes alone), and compared to a reference group (no prediabetes or anxiety/depression) on the likelihood of developing diabetes during the follow-up period.
Results
N = 1300 (1.8%) participants developed diabetes. While prediabetes alone was associated with incident diabetes (OR = 5.94; 95% CI = 5.10–6.90, p < 0.001), the group with combined prediabetes and depressive symptoms had the highest likelihood of developing diabetes over follow-up (OR = 8.29; 95% CI = 5.58–12.32, p < 0.001). Similar results were found for prediabetes and anxiety symptoms (OR = 6.57; 95% CI = 4.62–9.33, p < 0.001), compared to prediabetes alone (OR = 6.09; 95% CI = 5.23–7.11, p < 0.001), though with a smaller effect. The interaction between depressive symptoms and prediabetes was synergistic in age-and-sex adjusted analyses.
Conclusions
Individuals with elevated depressive, and to some extent anxiety, symptoms in combination with prediabetes may represent a high-risk subgroup for type 2 diabetes.
What's new?
- Depressive and anxiety symptoms may increase the likelihood of progressing from prediabetes to type 2 diabetes; however, research to date has been limited.
- We found that those with depressive symptoms combined with prediabetes were the most likely group to develop type 2 diabetes compared to those with either depressive symptoms or prediabetes alone.
- Findings suggest that those with depressive symptoms, and to some extent anxiety symptoms, and prediabetes should be closely monitored and may benefit from targeted prevention efforts.
1 INTRODUCTION
Prediabetes is characterized by impaired glucose regulation, with blood glucose levels falling above the normal range, yet below the diagnostic threshold for type 2 diabetes. Prediabetes is associated with an increased risk of developing type 2 diabetes,1 a prevalent2 chronic condition that can lead to serious vascular complications and premature mortality.3 In Europe, approximately one in five adults (22%) at risk of type 2 diabetes are estimated to meet the criteria for impaired glucose regulation,4 and estimates of up to 70% of those with prediabetes progressing to type 2 diabetes have been reported.5 Identifying factors that increase the risk of progressing from prediabetes to type 2 diabetes could help improve prevention efforts and aid in reducing the disease burden of prediabetes and type 2 diabetes.
Mental health conditions, such as depression and anxiety, and related symptoms have been shown in meta-analyses to increase the risk of developing type 2 diabetes, with pooled effect estimates ranging from 18%–60%.6-9 Previous research has also demonstrated that depressive and anxiety symptoms can compound the risk of type 2 diabetes among those with prediabetes. In a recent study of 1708 adults from Germany, anxiety was found to accelerate the progression from prediabetes to type 2 diabetes during a follow-up period of approximately 6.5 years.10 A longitudinal study of 2486 middle-aged adults from Canada also found that those with prediabetes combined with depression or anxiety had higher risks of self-reporting a diagnosis of type 2 diabetes approximately 5 years later compared to those with either condition alone.11 Together, these studies suggest that depressive and anxiety symptoms may play a central role in the transition from prediabetes to type 2 diabetes. However, given that shared pathophysiological pathways may exist linking depressive/anxiety symptoms and prediabetes to type 2 diabetes,5 it remains unclear whether depressive or anxiety symptoms and prediabetes are independent or interconnected risk factors for type 2 diabetes as more evidence is needed. Furthermore, prediabetes has been associated with an increased mental health disease burden compared to normoglycemia,12 and thus examining these interactions longitudinally in a large sample could provide us with a clearer understanding of their interplay.
The present study examined the longitudinal associations and interactions between elevated depressive and anxiety symptoms and prediabetes with the risk of developing type 2 diabetes in a large sample of middle age and older adults. We hypothesized that (1) elevated depressive symptoms amongst those with prediabetes would be associated with the greatest risk of developing type 2 diabetes, and (2) there would be a synergistic interaction between elevated depressive symptoms and prediabetes at baseline with the risk of developing type 2 diabetes. Similar hypotheses were examined for the interaction between elevated anxiety symptoms and the risk of developing type 2 diabetes.
2 METHODS
2.1 Sample
Data were from the Lifelines Cohort Study and Biobank (Lifelines).13 Lifelines is a multi-disciplinary prospective population-based cohort study examining in a unique three-generation design the health and health-related behaviours of 167,729 persons living in the North of the Netherlands. It employs a broad range of investigative procedures in assessing the biomedical, socio-demographic, behavioural, physical and psychological factors which contribute to the health and disease of the general population, with a special focus on multi-morbidity and complex genetics. The design of Lifelines involves repeated survey data collection and laboratory visits where biological samples are collected and anthropometric assessments are performed, with data collected on a rolling basis. Baseline surveys and laboratory assessments were completed in 2007–2013; follow-up surveys were completed in 2011–2014 and 2012–2015; and a second laboratory visit, and third follow-up survey were completed in 2014–2017. Details on the Lifelines design and recruitment procedures are described elsewhere.13, 14 The Lifelines study design was approved by the Ethics Committee of the University Medical Centre Groningen and all participants provided informed consent prior to participation.
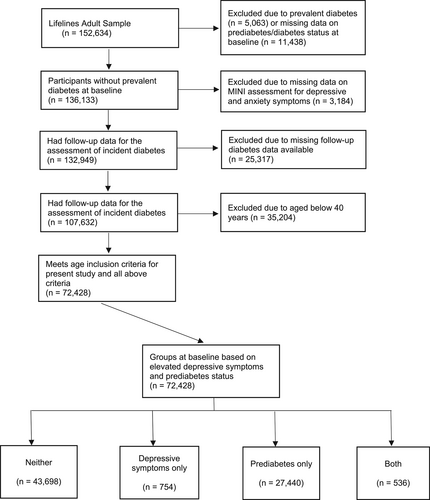
Data on 152, 634 adults were originally available from baseline. For the present analyses, the following inclusion criteria were applied: (1) having complete data on the screening tool for depressive and anxiety symptoms and on glycated haemoglobin A1c (HbA1c) at baseline, (2) being aged 40 years old or older at baseline, (3) not having diabetes at baseline, and (4) having available data on diabetes status in at least one follow-up survey or the follow-up laboratory visit. The final analytical sample for the present study was 72,428 participants, with a mean age of 51.4 years (58.1% female). A participant selection flow chart is presented in Figure 1.
2.2 Measures
Depressive and anxiety symptoms were assessed using the Mini International Diagnostic Interview (MINI),15 a screening tool for current major depressive disorder episodes and generalized anxiety disorder, at baseline. The MINI is a structured interview designed to briefly assess psychiatric disorders according to the Diagnostic Statistical Manual IV or International Classification of Diseases-10 diagnostic criteria. Respondents were asked whether they experienced depressive symptoms, such as sadness or anhedonia, in the past 2 weeks, and generalized anxiety symptoms, such as excessive worry and anxiety about several different topics, in the past 6 months. Previous research supports the reliability and validity of the MINI.15, 16 More information about the use of MINI as a diagnostic tool for depressive and anxiety symptoms in the Lifelines study is available elsewhere.17, 18 In the present study, the elevated depressive symptoms group and the elevated anxiety symptoms group refers to those with a positive screen for major depressive disorder and generalized anxiety disorder, respectively, on the MINI.
Prediabetes was determined by baseline HbA1c levels, collected from 2008 to 2013, ranging from 39 mmol/mol (5.7%) to 46 mmol/mol (6.4%), according to the American Diabetes Association (ADA) diagnostic criteria for prediabetes.19 The ADA HbA1c threshold for prediabetes is lower than other diagnostic guidelines such as those published by the World Health Organization (42 mmol/mol or 6.0%) and was therefore selected to identify a greater number of participants at high risk. Incident type 2 diabetes at follow-up was determined by HbA1c levels of 47 mmol/mol (6.5%) or above during the second laboratory visit or by self-reported physician diagnosis at any of the three follow-up survey assessments. Information on the laboratory analysis is described elsewhere.20 Participants with HbA1c levels of 47 mmol/mol (6.5%) or above at baseline, with a self-reported physician diagnosis of diabetes at baseline or with missing data on diabetes status at baseline, were excluded.
Covariates, including sociodemographic and lifestyle/health characteristics at baseline, were examined in adjusted analyses, and are presented, with their respective categories, in Table 1. Apart from body mass index (BMI), covariates were based on self-report. Socio-demographic covariates included age, sex, ethnicity, educational attainment and marital status. Response options for ethnicity included white/eastern and western European, white/Mediterranean or Arabic, Black, Asian and other (e.g., mixed ethnicities). The two first response categories were collapsed for analysis. Physical activity was assessed by the number of days active during a typical week in the past month, derived from the Short Questionnaire to Assess Health Enhancing Physical Activity (SQUASH) questionnaire,21 with scores ranging from 0 to 7 days per week. Smoking status was coded as non-smoker or current smoker. BMI was measured by trained research staff during the laboratory visit and was calculated as kg in weight/meters2 in height and categorized according to World Health Organization BMI classification. Alcohol consumption frequency was assessed by asking respondents how often, in the past 4 weeks, did they drink alcoholic drinks.
| Variable | Sample (N = 72,428a) | |
|---|---|---|
| N | % | |
| Sex | ||
| Female | 42,064 | 58% |
| Male | 30,364 | 42% |
| Age | ||
| 40–44 | 17,207 | 24% |
| 45–59 | 40,651 | 56% |
| 60–74 | 13,775 | 19% |
| 75 and above | 795 | 1% |
| Educational attainment | ||
| Low (lower vocational education or less) | 24,582 | 34% |
| Medium (lower secondary or intermediate vocational education) | 26,660 | 37% |
| High (higher secondary or vocational education or more) | 20,332 | 28% |
| Marital status | ||
| Married/civil partnership | 40,732 | 87% |
| In a relationship, living apart | 1136 | 2% |
| Single/widowed/divorced | 4922 | 10% |
| Ethnicity | ||
| White | 66,279 | 99% |
| Asian | 261 | <1% |
| Black | 81 | <1% |
| Other | 524 | 1% |
| Body mass index | ||
| Normal weight (BMI up to 24.9) | 30,047 | 42% |
| Overweight (BMI 25–29.9) | 31,280 | 43% |
| Obese (BMI 30 and above) | 11,076 | 15% |
| Smoking | ||
| No | 59,666 | 83% |
| Yes | 12,306 | 17% |
| Alcohol use, past month | ||
| None | 13,868 | 19% |
| 1 day per month | 3956 | 6% |
| 2–3 days per month | 8015 | 11% |
| 1 day per week | 9260 | 13% |
| 2–3 days per week | 17,411 | 24% |
| 4–5 days per week | 8777 | 12% |
| 6–7 days per week | 10,692 | 15% |
| Days active, typical week in past month | ||
| 0 | 5093 | 8% |
| 1 | 5361 | 8% |
| 2 | 7347 | 11% |
| 3 | 8143 | 12% |
| 4 | 7981 | 12% |
| 5 | 9289 | 14% |
| 6 | 7517 | 11% |
| 7 | 16,496 | 25% |
| Elevated depressive symptoms | ||
| No | 71,138 | 98% |
| Yes | 1290 | 2% |
| Elevated anxiety symptoms | ||
| No | 69,924 | 97% |
| Yes | 2504 | 3% |
| Prediabetes | ||
| No prediabetes | 44,452 | 61% |
| Prediabetes | 27,976 | 39% |
| Depression-prediabetes groups | ||
| Neither | 43,698 | 60% |
| Depressive symptoms only | 754 | 1% |
| Prediabetes only | 27,440 | 38% |
| Depressive symptoms and prediabetes | 536 | 1% |
| Anxiety-prediabetes groups | ||
| Neither | 42,903 | 59% |
| Anxiety symptoms only | 1549 | 2% |
| Prediabetes only | 27,021 | 37% |
| Anxiety symptoms and prediabetes | 955 | 1% |
| Incident Diabetes | ||
| No diabetes | 71,128 | 98% |
| Diabetes | 1300 | 2% |
- a Sample size varies due to missing data on covariates.
2.3 Statistical analysis
Descriptive statistics were examined for baseline depressive and anxiety symptoms groups, prediabetes status, and incident type 2 diabetes at follow-up. Logistic regression analyses first examined the independent associations between depressive symptoms, anxiety symptoms, and prediabetes with the risk of type 2 diabetes in separate analyses. Groups formed based on the presence and absence of elevated depressive symptoms, elevated anxiety symptoms, and prediabetes were first modelled independently (i.e., each group entered in a separate analysis) as predictors of new-onset type 2 diabetes. The potential joint effect of elevated depressive or anxiety symptoms and prediabetes on type 2 diabetes was then examined in separate logistic regression analyses, where participants were categorized into one of four mutually exclusive groups: (1) no prediabetes and no/low depressive symptoms; (2) elevated depressive symptoms only; (3) prediabetes only; and (4) both elevated depressive symptoms and prediabetes. Similar groups were formed for elevated anxiety symptoms and prediabetes status. In both sets of analyses, the reference category was those with no/low depressive/anxiety symptoms and without prediabetes. Odds ratios (OR) with 95% confidence intervals (CI) are reported. The Rothman Synergy Index (S)22-24 was calculated to examine whether the joint effect of prediabetes and depressive/anxiety symptoms was greater than the sum of the individual effects. An S value greater than 1.00 is indicative of synergism (i.e., greater than the additive effect). Analyses were performed using Stata Version 14 (StataCorp, College Station, TX). The 95% confidence intervals for S were calculated using the Stata IC package for biological interaction.25
A subgroup analysis was additionally performed to examine the associations between elevated depressive symptoms and elevated anxiety symptoms in the transition from prediabetes to type 2 diabetes, with a subset of participants with prediabetes at baseline (n = 27,976).
Of the included sample, the number of missing values for the covariates ranged from 0.3% (BMI) to 35% (marital status). Missing data on covariates were imputed using the multiple imputation by chained equation procedure in Stata with 20 generated data sets.26 S in fully adjusted analyses was calculated with complete cases only. All other fully adjusted analyses with complete cases are presented in Tables S1 and S2.
3 RESULTS
There were 1300 (1.8%) new cases of type 2 diabetes over a follow-up period of up to 9 years. At baseline, there were 27,976 participants with prediabetes, 1290 participants with elevated depressive symptoms and 2504 participants with elevated anxiety symptoms. Sample sizes according to groups stratified by the presence/absence of prediabetes and depressive symptoms, as well as by the presence/absence of prediabetes and anxiety symptoms, are presented in Table 1. Tables S3 and S4 describe the baseline sample characteristics according to groups.
Table 2 demonstrates the proportions within each group with incident diabetes as well as the results of the logistic regression analyses. In univariate analyses, elevated depressive symptoms were associated with a 42% increased likelihood of incident type 2 diabetes (95% CI = 1.02, 1.99) and prediabetes was associated with an almost 6-fold increased likelihood of incident type 2 diabetes (OR = 5.91, 95% CI = 5.09, 6.86), after adjusting for socio-demographic and health-related covariates. Elevated anxiety symptoms were not uniquely associated with incident type 2 diabetes in fully adjusted analyses. However, in age and sex adjusted analyses, elevated anxiety symptoms were associated with a 46% increased likelihood of incident type 2 diabetes (95% CI = 1.11, 1.92).
| Group | N incident type 2 diabetes (%) | OR (95% CI) Age-and-sex adjusted | OR (95% CI) Fully adjusted |
|---|---|---|---|
| Univariate associations | |||
| Depressive symptoms | |||
| No | 1252 (1.8%) | Reference | Reference |
| Yes | 38 (2.9%) | 1.88 [1.35, 2.61], p < 0.001 | 1.42 [1.02, 1.99], p = 0.038 |
| Anxiety symptoms | |||
| No | 2449 (3.44%) | Reference | Reference |
| Yes | 55 (4.2%) | 1.46 [1.11, 1.92], p = 0.007 | 1.23 [0.93, 1.63], p = 0.141 |
| Prediabetes | |||
| No | 26,898 (37.8%) | Reference | Reference |
| Yes | 1078 (82.9%) | 7.18 [6.20, 8.33], p < 0.001 | 5.91 [5.09, 6.86], p < 0.001 |
| Joint associations: depressive symptoms | |||
| Neither | 215 (0.5%) | Reference | Reference |
| Depressive symptoms only | <10 (<1%) | 2.02 [0.95, 4.30], p = 0.069 | 1.60 [0.75, 3.42], p = 0.227 |
| Prediabetes only | 1047 (3.8%) | 7.20 [6.20, 8.37], p < 0.001 | 5.94 [5.10, 6.90], p < 0.001 |
| Both | 31 (5.8%) | 12.37 [8.39, 18.22], p < 0.001 | 8.29 [5.58, 12.32], p < 0.001 |
| Joint associations: anxiety symptoms | |||
| Neither | 207 (0.5%) | Reference | Reference |
| Anxiety symptoms only | 15 (1.0%) | 2.20 [1.30, 3.73], p = 0.003 | 1.94 [1.14, 3.30], p = 0.014 |
| Prediabetes only | 1038 (3.8%) | 7.40 [6.35, 8.61], p < 0.001 | 6.09 [5.23, 7.11], p < 0.001 |
| Both | 40 (4.2%) | 9.08 [6.42, 12.83], p < 0.001 | 6.57 [4.62, 9.33], p < 0.001 |
- Note: Incident diabetes was defined as either a self-reported physician diagnosis or an HbA1c level ≥47 mmol/mol (6.5%) during the follow-up period. Fully adjusted analyses control for age, sex, educational attainment, ethnicity, marital status, body mass index category, physical activity, alcohol consumption, and smoking status. Groups with sample sizes of less than 10 are considered as potentially identifiable and are therefore reported as <10, in accordance with the Lifelines publishing guidelines.
In fully adjusted joint analyses examining prediabetes and elevated depressive symptoms, we found that the greatest likelihood of developing type 2 diabetes was amongst those with combined prediabetes and elevated depressive symptoms (OR = 8.29, 95% CI = 5.58, 12.32); followed by those with prediabetes only (OR = 5.94, 95% CI = 5.10, 6.90); and by those with elevated depressive symptoms only (OR = 1.60, 95% CI = 0.75, 3.42). Similar results were found with elevated anxiety symptoms and prediabetes, with the highest odds found amongst those with combined prediabetes and elevated anxiety symptoms (OR = 6.57, 95% CI = 4.62, 9.33); followed by those with prediabetes only (OR = 6.09, 95% CI = 5.23, 7.11); and by those with elevated anxiety symptoms only (OR = 1.94, 95% CI = 1.14, 3.30).
The synergy index, adjusted for age and sex, suggests that the joint effect of elevated depressive symptoms and prediabetes was greater than the sum of the individual effects (S = 1.57, 95% CI = 1.002, 2.474, p = 0.049). Notably, the confidence intervals for S overlap with 1.00 when adjusting for all covariates (S = 1.34, 95% CI = 0.74, 2.45, p = 0.336). S for the joint effect of elevated anxiety symptoms and prediabetes was >1.00 in the age-and-sex adjusted analysis, consistent with synergism, but with confidence intervals that overlapped with 1.00 (S = 1.06, 95% CI = 0.72, 1.57). S for elevated anxiety symptoms and prediabetes in the fully adjusted analysis was not indicative of synergism (S = 0.91, 95% CI = 0.52, 1.57, p = 0.734).
As shown in Table 3, we found that elevated depressive symptoms were associated with an approximate 70% increased risk of progression from prediabetes to diabetes among those with prediabetes at baseline (95% CI = 1.18, 2.47). However, the effect estimate decreased in the fully adjusted analysis (OR = 1.39, 95% CI = 0.96, 2.03). Elevated anxiety symptoms were not associated with the progression from prediabetes to type 2 diabetes in the subgroup analyses.
| Group | N incident type 2 diabetes (%) | OR (95% CI) Age-and-sex adjusted | Or (95% CI) Fully adjusted |
|---|---|---|---|
| Elevated depressive symptoms | |||
| No | 1047 (3.8%) | Reference | Reference |
| Yes | 31 (5.8%) | 1.70 (1.18, 2.47), p = 0.005 | 1.39 (0.96, 2.03), p = 0.085 |
| Elevated anxiety symptoms | |||
| No | 1038 (3.8%) | Reference | Reference |
| Yes | 40 (4.2%) | 1.21 (0.88, 1.68), p = 0.24 | 1.07 (0.77, 1.49), p = 0.685 |
- Note: Fully adjusted analyses control for age, sex, educational attainment, ethnicity, marital status, body mass index category, physical activity, alcohol consumption, and smoking status.
4 DISCUSSION
The present study examined the longitudinal associations between prediabetes and elevated symptoms of depression and anxiety with the risk of developing type 2 diabetes during a follow-up period of up to 9 years. Overall, our hypotheses were partially supported. When groups were stratified by the presence/absence of elevated depressive/anxiety symptoms and prediabetes at baseline, those with combined elevated depressive symptoms and prediabetes were the most likely group to develop type 2 diabetes, in age-and-sex adjusted analyses and in analyses adjusted for sociodemographic and lifestyle/health characteristics. Furthermore, in age-and-sex adjusted analyses, elevated depressive symptoms and prediabetes interacted in a synergistic way, compounding the risk of developing type 2 diabetes. This finding was in line with previous findings from Canada,11 although synergism in the present study decreased in fully adjusted analyses. Participants with combined elevated anxiety symptoms and prediabetes were also the most likely group to develop type 2 diabetes in the stratified analyses, though with no indication of a synergistic interaction.
In subgroup analyses, among those with prediabetes at baseline, we found that only elevated depressive symptoms increased the likelihood of progressing to type 2 diabetes, a finding that weakened in fully adjusted analyses. The finding that elevated anxiety symptoms was not associated with the progression from prediabetes to diabetes is inconsistent with a previous study from Germany,10 where the presence of anxiety was found to accelerate progression to type 2 diabetes. This discrepancy may be attributable to measurement differences, a higher overall incidence of type 2 diabetes in the previous study, or the use of a diagnostic interview compared to self-report scales for depressive and anxiety symptoms,10 and highlights the need for further research on the potential synergistic role of mental health in progressing from prediabetes to type 2 diabetes.
The present study contributes to the limited longitudinal research examining the combined role of mental health and prediabetes as risk factors for developing type 2 diabetes. There are several possible mechanisms through which depression, and to some extent anxiety, may contribute to an increased likelihood of prediabetes developing into type 2 diabetes. Increased activity of the hypothalamic–pituitary–adrenal (HPA) axis is associated with the pathophysiology of depression and anxiety,27 which, through increased cortisol exposure, can lead to a number of metabolic precursors for type 2 diabetes (e.g., insulin resistance, hypertension and visceral adiposity).28 Similarly, inflammatory markers and activation of the immune system have also been suggested as links between depression and the development of diabetes.5 Depression is associated with the activation of several connected biological systems, including the HPA-axis, sympathetic nervous system, and inflammatory responses, that can affect insulin resistance and glycaemic outcomes.28 Further confounding the relationship between depression, anxiety, and the transition from prediabetes to type 2 diabetes is that some medications prescribed for treating these mental health disorders have been shown to be associated with an increased risk of type 2 diabetes.29 Individuals with mental health difficulties may also engage in increased use of health services, and therefore may be more likely to have other conditions such as diabetes screened for and identified earlier, thus increasing the likelihood of self-reporting a diabetes diagnosis. Depressive and anxiety symptoms are also associated with suboptimal lifestyle behaviours, such as smoking, increased calorie consumption, and decreased physical activity, which are all in turn associated with an increased risk of type 2 diabetes.28 Therefore, depressive and anxiety symptoms may compound biological, metabolic, and lifestyle risk factors, contributing to the progression of prediabetes to type 2 diabetes.
The main strengths of the present study were the use of a large prospective cohort study with objective assessments of prediabetes and type 2 diabetes, including both diagnosed and undiagnosed diabetes. Despite its strengths, the study had important limitations. First, although the incidence of diabetes in middle age and older adulthood is most likely to represent type 2 diabetes rather than type 1 diabetes, it was not possible to objectively differentiate between the two conditions in the present study. The date of onset for diabetes diagnoses was also not available, and the analyses did not control for potential medications taken for depression, anxiety or prediabetes. In addition, the sample had limited ethnic and racial diversity. While Lifelines is representative of the northern provinces of the Netherlands, it is a largely homogeneous population.13 The study was also limited by the sole use of the MINI, assessed at only one point in time, as a screening tool for depressive and anxiety symptoms. As a diagnostic screening interview, the MINI may have a lower proportion of positive responses on the depressive and anxiety assessments compared to self-reported symptom scales, which may make it difficult to compare across studies using different instruments. Future research using more detailed, comprehensive assessments of depression and anxiety, with frequent assessments to capture change, is needed on prediabetes, mental health and the risk of type 2 diabetes. Despite the large sample size, the present study was also limited by a relatively small number of incident cases of diabetes within each group. Replicating the study in another large dataset with multiple measurement would be beneficial. Unmeasured confounding is a risk in all observational research and may be present in this study. Finally, all Lifelines participants receive feedback on their health status after they take part in the study, and receiving such feedback has been shown to reduce the risk of cardiovascular disease via the initiation of preventive behaviours.30 Therefore, the present sample may represent a relatively healthier sample compared to the general population.
To conclude, our study suggests that individuals with combined depressive symptoms and prediabetes may represent a unique subgroup that is particularly vulnerable to type 2 diabetes. Therefore, this group may benefit from greater monitoring and preventive care. Future research should aim to further disentangle the mechanisms linking mental health and prediabetes to type 2 diabetes and aim to investigate the temporal dynamics between the onset of depressive or anxiety symptoms and the onset of prediabetes. Further research using complex assessments of anxiety symptoms and longer follow-up periods is needed to examine the role of anxiety in the progression to type 2 diabetes among individuals with prediabetes. Together, this could help improve our understanding of the complex ways in which mental health symptoms and prediabetes may interact to contribute to the development of type 2 diabetes.
AUTHOR CONTRIBUTIONS
Sonya S. Deschênes, Amy McInerney, Finiki Nearchou, Arie Nouwen, and Norbert Schmitz conceptualized the study and planned the study design. Sonya S. Deschênes conducted the statistical analyses. Sonya S. Deschênes, Brendan Byrne, and Amy McInerney wrote the first draft of the manuscript. All authors reviewed and edited the manuscript. All authors approved the final version of the manuscript.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the services of the Lifelines Cohort Study, the contributing research centres delivering data to Lifelines, and all the study participants. Open access funding provided by IReL.
FUNDING INFORMATION
The Lifelines initiative has been made possible by subsidy from the Dutch Ministry of Health, Welfare and Sport, the Dutch Ministry of Economic Affairs, the University Medical Center Groningen (UMCG), Groningen University and the Provinces in the North of the Netherlands (Drenthe, Friesland, Groningen). The present study was additionally funded by the University College Dublin Ad Astra Start Up grant and from a support grant from Enterprise Ireland.
CONFLICT OF INTEREST STATEMENT
None to report.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of the present study are available by Lifelines (https://www.lifelines.nl/); however, data access is restricted. Requests for data access can be sent to the Lifelines Cohort Study and Biobank (https://www.lifelines.nl/researcher/how-to-apply).