Predictive value of 18–24 month neuro-sensory motor developmental assessment for pre-school motor development in high risk, medically complex children
I10
R-A de Regnier, M Weck, M Kay Santella, C Patrick, A Russow, L Boswell
Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA
Background and Objective(s): Many follow up programs monitor high-risk children through 18–24 months of corrected age (CA) but relatively few programs continue to monitor children through preschool or later. The Neuro-Sensory Motor Developmental Assessment (NSA) is a standardized motor assessment used for infants and toddlers that correlates well with the need for therapy at 18–24 months and has been used to predict the quality of life in medically complex children. The purpose of this study was to evaluate the need for ongoing follow up at preschool age for children who were previously evaluated at 18–24 months CA.
Study Design: This was a secondary analysis of a prospective longitudinal study of motor development.
Study Participants & Setting: High-risk children were enrolled at 10–15 weeks of CA from the follow-up clinic if they were extremely preterm (<29 weeks of gestation, n=34), had neonatal cardiac surgery (n=34), neonatal neurologic abnormalities (n=23) or were hospitalized in an intensive care unit at 10 weeks post-term age (n=6).
Materials/Methods: The NSA was performed at 18–24 months of CA and the Movement Assessment Battery for Children, 2nd edition (BC-2) at 3.5–5 years of CA (preschool age). Both were performed by a physical therapist (PT) blinded to the neonatal risk factors. NSA scores were categorized (according to the manual) as normal or minimal, mild, moderate, severe and profound impairments. Low scores on the BC-II were defined as those <5% or if the child was unable to complete the items for that section of the test due to low abilities, as judged by the PT. Children who did not complete test items due to waning attention span were excluded from the relevant data analysis.
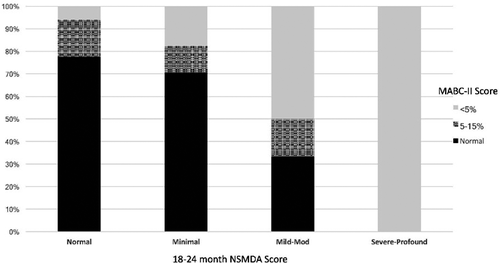
Results: NSA and total BC-II classifications were significantly correlated (p<0.001) for the 85 children with full scores for both tests (Figure). All children with severe-profound impairments on the NSA at 18–24 months CA also had scores <5% or could not be tested using the preschool BC-II. Most children with normal 18–24 month NSA scores had normal preschool BC-II scores (38/49; 77.6%), but 22.4% were noted to have borderline (5–15%, n=8) or low (<5%; n=3) total BC scores at preschool. NSA Fine Motor (FM) scores <25% were correlated with BC-II Manual Dexterity scores (p<0.001), but only 42/73 (57.%) of those with normal 18–24 month NSA FM scores had normal BC-II Manual Dexterity scores at preschool. NSA Gross Motor (GM) scores <25% were correlated with BC-II Aiming and Catching Scores and Balance scores (both p<0.001). Of the children with a normal NSA GM score, 63/73 (86.3%) had normal Aiming/Catching scores and 60/71 (84.5%) had normal balance scores at preschool.
Conclusions/Significance: Although there was a significant correlation between 18–24 month NSA scores and later BC-II scores, in this population of medically complex infants, children with normal NSA scores tended to develop more problems over time, particularly for manual dexterity. As these children may benefit from therapy services prior to school entry, ongoing follow up of motor development should continue beyond 18–24 months in high risk, medically complex infants.