Consistency of problem identification and treatment recommendations among interpreters within a clinical motion laboratory
G8
T Novacheck1, J Stout2
1James R. Gage Center for Gait & Motion Analysis Gillette Children's Specialty Healthcare, Department of Orthopedics University of Minnesota, St. Paul, MN, USA; 2James R. Gage Center for Gait & Motion Analysis; Gillette Children's Specialty Healthcare, St. Paul, MN, USA
Background and Objective(s): Variability in treatment recommendations among interpreters of gait data is frequently cited as one of the primary reasons that the utility of gait analysis for surgical decision making remains controversial.[1–2] The subjective nature of the interpretation process is often cited, including the fact that treatment recommendations appear to be influenced by institutional and regional differences.[3] However, regional variations in practice are present in many specialties in medicine.[4] The question of consistency of treatment recommendations within an institution has not been addressed. The Center for Gait and Motion Analysis (CG) of Gillette Children's Specialty Healthcare implemented a process to assess the consistency among interpreters of gait data. The purpose of this study is to describe the consistency of treatment recommendations among multiple interpreters of gait analysis data within a single institution.
Study Design: Descriptive.
Study Participants & Setting: 7 orthopedic physician interpreters of gait data within a tertiary care facility for children with disabilities.
Materials/Methods: Quarterly assessment of consistency among physician interpreters was instituted. A checklist of 22 surgical interventions (2 neurosurgical, 20 orthopaedic procedures (10 bony, 10 soft tissue) and 4 non-surgical options) was created for treatment identification. A graphical user interface was used for direct entry. Data was electronically stored. Cases were selected to reflect the range of GMFCS levels [5] typically seen in the CG. Each case is presented to the interpreter in routine fashion with no other interpreters present. All data typically utilized in a case interpretation was available for review including medical records and imaging. Interpreters were not blinded to the fact that the case is the quarterly consistency case, nor to the referring physician of record. They were blinded to any images, medical records or treatment subsequent to the date of the study. Data chosen for analysis represent 4 consecutive quarters of data between 2015–2016 with 7 interpreters. The mode (majority choice) for each treatment option was chosen as the basis of comparison. The percent agreement with the mode was calculated for each interpreter for each of the 22 surgical treatments. A composite percent agreement was determined for each interpreter for each case. These were averaged across the 4 cases for each interpreter for final comparison.
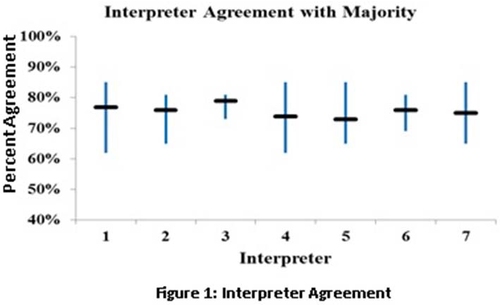
Results: The interpreters had an average of 20 years of gait lab interpretation experience (range 8–32 years). All cases were children with a diagnosis cerebral palsy (age: 9.7±2.4; 2M, 2F; one from each GMFCS level I-IV). Average percent agreement with the majority was 76% (range 73–79%). The range of variability within each interpreter was from 8–23% (Figure 1). No significant difference was noted between recommendations of bony vs. soft tissue procedures (89% and 88% respectfully). Non-surgical options were not included in this analysis.
Conclusions/Significance: The results of this study demonstrate that among a group of experienced physician interpreters of gait data within a single institution, good agreement can be achieved for treatment recommendations. Within institution reliability of treatment recommendations is essential to the consistency care for patients referred for gait analysis and to establishing reliability of gait analysis as a tool for clinical decision-making.
References: 1. Wright JG. G&P 2015; 2. Narayanan U. CurOpinPed 2007; 3. Skaggs DL. JPO 2000; 4. Vitale MG. JBJS 1999; 5. Palisano R. DMCN 1997