Exposure to endocrine-disrupting chemicals and implications for neurodevelopment
Abstract
Human brain development is a complex multistep process that is partly coordinated by the endocrine system. Any interference with the endocrine system might affect this process and result in deleterious outcomes. Endocrine-disrupting chemicals (EDCs) represent a large group of exogenous chemicals with the capacity of interfering with endocrine functions. In different population-based settings, associations between exposure to EDCs, particularly in prenatal life, and adverse neurodevelopmental outcomes have been demonstrated. These findings are strengthened by numerous experimental studies. Although mechanisms underlying these associations are not entirely delineated, disruption of thyroid hormone and, to a lesser extent, sex hormone signalling have been shown to be involved. Humans are constantly exposed to mixtures of EDCs, and further research combining epidemiological and experimental settings is required to improve our understanding of the link between real-life exposures to these chemicals and their impact on neurodevelopment.
Graphical Abstract
Abbreviations
-
- ADHD
-
- attention-deficit/hyperactivity disorder
-
- ASD
-
- autism spectrum disorder
-
- BPA
-
- bisphenol A
-
- EDC
-
- endocrine-disrupting chemical
-
- PBDE
-
- polybrominated diphenyl ether
-
- PCB
-
- polychlorinated biphenyl
-
- PFAS
-
- per- and polyfluoroalkyl substance
What this paper adds
- Endocrine-disrupting chemical exposure is linked to impaired brain development.
- The impact of endocrine-disrupting chemicals on brain development is supported by evidence from a population-based to a molecular level.
- Study of human-relevant chemical mixtures, rather than single compounds, is necessary to fully understand the impact of endocrine-disrupting chemicals on human health.
Human brain development is a highly complex process that starts in the third gestational week and continues until early adulthood.1 This complex process involves tightly regulated cellular events, consisting of proliferation, migration, differentiation, and myelination, among others.1 The endocrine system governs many of these key events throughout neurodevelopment and thus constitutes a fundamental element of the process. Therefore, any kind of internal or external influence on the endocrine system could affect neurodevelopment. Exposure to endocrine-disrupting chemicals (EDCs), a group of chemicals altering hormone systems, stands as a major example of environmental interference.
The prenatal period and early childhood are particularly critical stages for neurodevelopment. Many programmed key events of neurodevelopment occur during these periods; therefore, the fetus and infant are especially vulnerable to environmental effects including EDC exposure.2 Puberty is another critical life stage because of increased neuroendocrine activity. Exposure to chemicals interfering with hormonal pathways during these critical stages of neurodevelopment is indicated to result in adverse cognitive and behavioural outcomes.2
In this review, we first provide a summary of EDCs' main characteristics and major sources for human exposure. We continue by outlining the evidence supporting the link between EDC exposure and neurodevelopment from population-based and experimental studies and the pertinent underlying biological mechanisms.
ENDOCRINE-DISRUPTING CHEMICALS
Brief history, definition, and main characteristics
The first evidence of the detrimental impact of EDCs on human health goes back to the 1940s when the use of diethylstilboestrol was initiated. Diethylstilboestrol, a synthetic oestrogen, was introduced to prevent miscarriage and other pregnancy complications and thus was frequently prescribed to pregnant females.3 However, diethylstilboestrol was shown to cause vaginal cancer among female offspring and be associated with some genital malformations among male offspring.3 Furthermore, it has been associated with multigenerational neurodevelopmental issues such as attention-deficit/hyperactivity disorder (ADHD).4 The use of diethylstilboestrol was banned in the late 1970s in the USA and many European countries; still, diethylstilboestrol stands as a representative example of a chemical that causes adverse health outcomes throughout generations by interfering with the hormone systems. In spite of this and accumulating evidence from contemporaneous studies on the link between chemical use and reproductive abnormalities in wildlife, the term ‘endocrine disruptor’ was coined for the first time only in 1991 at the Wingspread Conference.3 In 2002, the World Health Organization and International Programme on Chemical Safety introduced the definition of an endocrine disruptor as ‘an exogenous substance or mixture that alters function(s) of the endocrine system and consequently causes adverse health effects in an intact organism, or its progeny or (sub)populations’, and this definition is generally accepted among the scientific community and in the regulatory context.3
EDCs can affect hormonal function in numerous different ways (e.g. by acting directly on hormone receptors, altering hormone receptor expression, signal transduction in hormone-responsive cells, or hormone metabolism or transport).5 They can also act on cell fate or death of endocrine cells or hormone-responsive cells.5
EDCs induce complex effects, which can be explained by the mechanisms underlying their actions. Like hormones themselves, EDCs show effects at low doses, often within the range of environmental exposure.6 Considering that receptors can be saturated readily, hormones and EDCs both generate non-linear dose responses, most commonly sigmoidal dose–response curves, which makes their actions at low doses more relevant as the small changes in doses can create significant differences in response at the low end of a sigmoidal curve.6 Besides, they can produce non-monotonic dose responses (e.g. U-shaped or inverted U-shaped), which might be originated from acting on ample receptors with different affinities, the changes in receptor affinity at different doses of the substrate, up- or downregulation of receptors, or cytotoxic responses of the hormone-responsive cells.6 Since some EDCs act on a plethora of receptors and, in some cases, have a higher affinity towards receptors, they can even exert more prominent non-monotonic dose responses than the hormones themselves.6 Further, different EDCs display additive or synergistic effects in the body, which is sometimes referred to as the cocktail effect.3
Sources of exposure
EDCs comprise a large group of different classes of chemicals, such as phenols (bisphenol A [BPA] and its analogues), phthalates, per- and polyfluoroalkyl substances (PFASs), alkylphenols, brominated flame retardants, halogenated aromatic hydrocarbons, and organochlorine compounds.7 As of today, most of the organochlorine compounds, polychlorinated biphenyls (PCBs), a subgroup of halogenated aromatic hydrocarbons, and some PFASs are banned; the use of several other EDCs is restricted in accordance with the Stockholm Convention.8 Nevertheless, a considerable number of those banned chemicals are still found in the environment because of their persistence, and in the human body, as most of them cannot be excreted entirely. In this manner, most of these banned or restricted chemicals still pose a serious threat to health, in addition to the ones currently in common use.
Humans are exposed to a large number of EDCs on a daily basis. The main sources of EDC exposure for humans can be listed as diet and food packaging materials, personal care products and cosmetics, cleaning products, consumer goods, drugs, and pesticides.3 In the food industry, BPA is widely used for hard-plastic-containing materials and the inner coating of cans; PFASs are commonly used for food packaging because of their water and oil repellent features.3 Phthalates are used in the production of soft plastic (e.g. for food packaging materials, PVC flooring, and medical tubings).3 Personal care products and cosmetics are also rich in EDCs, for instance, triclosan, parabens, and benzophenones are used as antimicrobial agents, preservatives, and sunscreens respectively.7 Consumer goods including electronic devices, building materials, medical instruments, and toys are other major sources of exposure that may contain different combinations of phthalates, PFASs, and brominated and phosphorylated flame retardants.3 Additionally, drugs can act as EDCs. One prominent example is paracetamol, notably considered safe to use during pregnancy, but recently shown to have endocrine-disrupting properties associated with adverse effects on sexual development in males.9 These various sources of EDC exposure result in the fact that humans are exposed to different mixtures of EDCs rather than single compounds.
LINKS BETWEEN EDC EXPOSURE AND NEURODEVELOPMENT
The brain is a noticeable target for EDCs, and exposure during neurodevelopment may result in unfavourable consequences. This is clearly supported by evidence from both epidemiological and experimental studies (summarized in Table 1). Even though the underlying mechanisms are still not fully delineated, recent findings shed light on the link between EDCs exposure and neurodevelopment.
| Chemicals | Major exposure sources | Association with human traits | Experimental evidence | Hormonal pathways involved |
|---|---|---|---|---|
| PCBs | Electrical equipment and devices | ASD, ADHD | Changes in memory, locomotor activity, sociosexual behaviour | Thyroid hormone signalling |
| PBDEs | Flame retardants | Cognition, ASD | Locomotor dysfunction, hyperactivity | Thyroid hormone signalling |
| PFASs | Food packaging, water-resistant consumer goods | ASD | Anxiety-like behaviour, changes in social and mate preference, stress response | Thyroid hormone signalling |
| Phenols | Hard-plastic-containing materials | Cognition, ASD, ADHD, externalizing behaviour, maladjustment | Anxiety-like behaviour, changes in social and mate preference, stress response, locomotion, memory | Thyroid and sex hormone signalling |
| Phthalates | Food packaging, personal care products, consumer goods | Cognition, ASD, ADHD | Changes in coping with stress, locomotion, social interaction | Thyroid hormone signalling |
- Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; PBDE, polybrominated diphenyl ether; PCB, polychlorinated biphenyl; PFAS, per- and polyfluoroalkyl substance.
Evidence from epidemiological studies
Epidemiological studies have focused on various neurodevelopmental outcomes including cognition, autism spectrum disorder (ASD), ADHD, and neurobehaviour, as well as some other psychiatric phenotypes, such as depression and anxiety. Numerous studies have investigated the relationship between prenatal exposure to different EDCs and cognitive traits. The strongest association with such traits has been established for organophosphate pesticides and polybrominated diphenyl ethers (PBDEs).10 Additionally, some phthalate metabolites have been shown to be negatively associated with IQ scores.11 These studies, conducted on a single chemical basis, have been complemented with approaches where mixture exposures have been taken into account. For example, Tanner et al. examined associations between exposure to a mixture of 26 EDCs and IQ in a population-based cohort study.12 Their analyses revealed that prenatal exposure to a mixture of EDCs was associated with lower IQ, in particular among young males, and bisphenol F was identified as a primary chemical of concern.
ASD or autistic features are some of the most studied neurodevelopmental outcomes in the context of EDC exposure. Ye et al. evaluated the existing scientific literature that connects EDC exposure to ASD and accompanying autistic traits.13 They concluded that prenatal exposure to BPA, some phthalates, PCBs, and PBDEs might be linked with the aetiology of ASD, autistic traits, or relevant neurobehavioural alterations. In addition, a potential association between PFASs and ASD has recently become concerning. In a high-risk ASD cohort, Oh et al. found that prenatal exposure to the two PFASs, perfluorooctanoic acid and perfluorononanoic acid, was associated with an increased risk of ASD.14
ADHD and related behavioural disturbances have also been a focus of epidemiological studies addressing neurodevelopmental disturbances arising from EDC exposure. The relationship between BPA exposures and ADHD or ADHD-related traits has been supported by some studies; yet, the results are inconsistent.15 Similarly, contradictory findings exist on the link between exposure to PCBs and ADHD. Even though there is supporting evidence for some PCBs' relation with ADHD traits,2 the lack of association from the pooled analysis from seven European birth cohort studies weakens this evidence.16 In this analysis, the researchers investigated the relationship between pre- and postnatal exposure to polychlorinated biphenyl-153, p–p´-dichlorodiphenyldichloroethylene, and hexachlorobenzene and ADHD among 4437 mother–child pairs; they did not find any association for increased risk of having ADHD before the age of 10 years. On the other hand, phthalates have been shown to be associated with ADHD more consistently.2
Since the prevalence of neurodevelopmental disorders is relatively low and subsyndromal symptoms might be the indicators of future neurodevelopmental disorders, researchers also examined the associations for neurobehavioural traits rather than full-blown disorders. There is increasing evidence of a link between different EDCs and internalizing (e.g. anxiety, somatization) or externalizing (e.g. aggression, hyperactivity) behaviours.10, 17 Even though identical associations could not be demonstrated in different populations, prenatal exposure to BPA, brominated flame retardants, and organophosphate pesticides were connected to an increased likelihood of having externalizing behaviours; BPA was also linked to maladjustment among children.10
Despite the growing findings on the associations between EDC exposure and adverse neurodevelopmental outcomes, the observational evidence from epidemiological studies remains somewhat inconclusive and making inferences is a challenging task. Different population characteristics, confounding factors, sampling time and analytical methods, sexually dimorphic dynamics, and the fact that humans are exposed to mixtures and not single chemicals are some of the reasons which hinder drawing definitive conclusions.15 Hence, experimental studies are critically important to validate observational findings and enlighten the molecular mechanistic background of the established associations.
Evidence from experimental studies
A substantial number of animal studies has tested the effects of EDCs on various neurodevelopmental processes and their relation to adverse outcomes. BPA is one of the most studied EDCs in animal studies and has been proven to affect numerous endpoints; brain volume differences, disturbances in spatial memory and spatial learning, and increased anxiety-like behaviour and aggression were demonstrated to be induced by exposure to BPA in rat and mouse models.18 Behavioural alterations were also established in zebrafish exposed to BPA.19 PCBs are another group of EDCs that have been examined thoroughly in animal models, and their significant effects on neuroendocrine signalling have been demonstrated.20 In mouse and rat models, alterations in memory, locomotor activity, and sociosexual behaviour have been observed due to PCB exposure.20 The effects of PBDEs on neuroendocrine signalling are also well established; similar behavioural changes in rats and mice, such as locomotor dysfunction and hyperactivity, have also been reported for PBDEs.20
In addition to the literature on the roles of single chemicals in neurodevelopment, the importance of addressing EDC mixtures has recently been demonstrated within the context of neurodevelopment.21 The study identified EDCs of concern for language development and created a mixture of these EDCs as measured in a population of Swedish pregnant females. Testing of this mixture in different experimental systems demonstrated that it induces behavioural changes and alterations in genes linked to neurodevelopmental disorders already at concentrations found in the human population.21 A similar mixture was used to treat mice at different doses throughout gestation, and it was shown to increase active coping with stress in both sexes, increased locomotion and decreased social interaction among males.22 The results exemplify the valid connection between experimental studies and observational epidemiological studies. In another study by Forner-Piquer et al., mice and zebrafish larvae were exposed to a mixture of pesticides containing six different chemicals.23 Increased anxiety-like behaviour and concomitant slowing pattern in electrocorticography were observed in the mouse model; behavioural changes, in particular motor behaviour, were present in zebrafish. In addition to these studies, Gore et al. recently used a mixture including bisphenols, phthalates, vinclozolin, and perfluorinated, polybrominated, and polychlorinated compounds to test postnatal brain development in rats.24 They reported sex-specific changes in rats' anxiety-like, social, and mate preference behaviours and stress responses.
Along with the in vivo studies delineating the role of EDCs in neurodevelopment, in vitro studies have also been performed. For instance, bisphenol S, a substitute for BPA, was shown to elicit impairment in neuronal proliferation and differentiation, and oxidative stress.25 Even though some inconsistencies in the experimental findings are present in the literature, the actual evidence leaves no room for doubt that EDCs impact on neurodevelopment in experimental settings.
Relevant biological mechanisms
EDCs can interfere with various endocrine pathways which are crucial for neurodevelopment. Thyroid hormones and sex steroids are endocrine pathways that have been studied most in the context of endocrine disruption and thus also in relation to neurodevelopment.
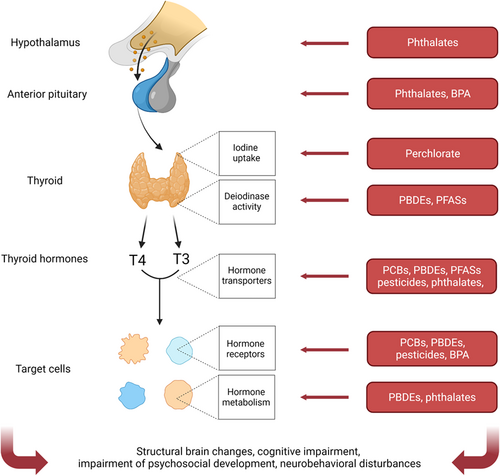
The importance of thyroid hormone signalling for pre- and postnatal brain development is well established in the scientific literature. Thyroid hormone deficiency is associated with impairment in cognition and psychomotor development as well as with structural brain changes.26 Thyroid hormone signalling plays a critical role in the link between EDCs and neurodevelopment, and there is a substantial amount of evidence showing that a number of EDCs interfere with thyroid homeostasis (Figure 1).26 PCBs have been shown to decrease triiodothyronine and thyroxine levels in the central nervous system of rats; PBDEs have also been linked to diminished thyroid hormone levels in humans, rats, and mice,20 which is profoundly pertinent for neurodevelopmental toxicity. Besides, pesticides, PFASs, phthalates, BPA, and other phenols were shown to act on the hypothalamus–pituitary–thyroid axis.26 They exert their effects via modes of actions, such as acting on thyroid hormone transporters, receptors, or metabolism.
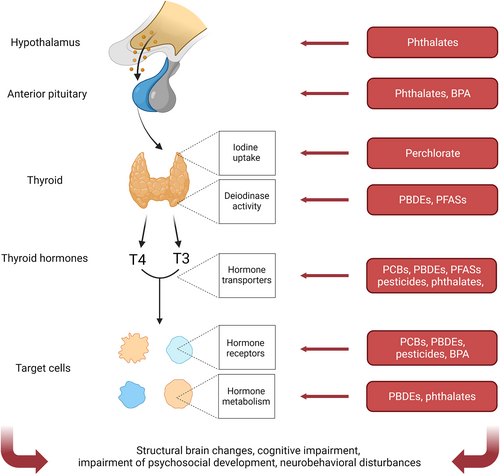
Effects of endocrine-disrupting chemicals on hormonal axes and their consequences on neurodevelopment, exemplified on thyroid hormone regulation
Abbreviations: BPA, bisphenol A; PBDE, polybrominated diphenyl ether; PCB, polychlorinated biphenyl; PFAS, per- and polyfluoroalkyl substance; T3, triiodothyronine; T4, thyroxine.
Sex hormones (oestrogens and androgens) also play a role in neurodevelopment. Influences of different sex hormones on cognitive traits including memory and learning and structural organization of the brain have been established.27 Thus, interference by EDCs with sex hormones during brain development could potentially result in neurodevelopmental deterioration. Examples of such EDCs are organochlorine compounds, alkylphenols, and bisphenols that can operate as oestrogen agonists and androgen antagonists,6 and phthalates, known for their anti-androgenic properties.28 Their ability to act on sex hormone receptors can partly explain the neurodevelopmental disturbances.
However, while separately the effects of EDCs on neurodevelopment on one hand, and hormonal signalling on the other hand, are well established, direct links between the endocrine mode of action and the neurodevelopmental outcomes in the same studies are hardly assessed. Furthermore, EDCs' impact on neurodevelopment cannot be limited to the few endocrine pathways mainly addressed in the literature given their widespread biological activity in the body. There are many more contributing pathways that are starting to be established as EDC targets; the hypothalamus–pituitary–adrenal axis, the retinoic acid pathway, and the peroxisome proliferator-activated receptors are also involved in neurodevelopment and might be targets of EDCs mediating neurodevelopmental effects as well.29, 30
CONCLUSION
Humans are constantly exposed to a large number of EDCs, and current evidence from epidemiological studies posit a clear link between exposure to EDCs and neurodevelopmental adversity. This link is also supported by numerous in vivo and in vitro studies. However, there are some inconsistencies in epidemiological findings, and our understanding of underlying mechanisms is still limited. Using more holistic approaches, for instance bridging observational human and experimental data and a stronger focus on chemical mixtures mimicking real-life exposures, could be important steps to overcome these limitations. Nevertheless, the current state of the science provides enough evidence to call for more restrictive use of EDCs in order to prevent human exposure during sensitive phases such as brain development.
ACKNOWLEDGMENTS
We acknowledge the financial support from Centre for Women's Mental Health during the Reproductive Lifespan—WOMHER and the funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No 825759.
CONFLICT OF INTEREST STATEMENT
The other authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.