Development and validation of the Pediatric Stroke Quality of Life Measure
Abstract
enAim
To develop and validate a disease-specific parent proxy and child quality of life (QoL) measure for patients aged 2 to 18 years surviving cerebral sinovenous thrombosis (CSVT) and arterial ischaemic stroke (AIS).
Method
Utilizing qualitative and quantitative methods, we developed a 75-item Pediatric Stroke Quality of Life Measure (PSQLM) questionnaire. We mailed the PSQLM and a standardized generic QoL measure, Pediatric Quality of Life Inventory (PedsQL), to 353 families. Stroke type, age at stroke, and neurological outcome on the Pediatric Stroke Outcome Measure were documented. We calculated the internal consistency, validity, and reliability of the PSQLM.
Results
The response rate was 29%, yielding a sample of 101 patients (mean age 9y 9mo [SD 4.30]; 69 AIS [68.3%], 32 CSVT [31.7%]). The internal consistency of the PSQLM was high (Cronbach's α=0.94–0.97). Construct validity for the PSQLM was moderately strong (r=0.3–0.4; p<0.003) and, as expected, correlation with the PedsQL was moderate, suggesting the PSQLM operationalizes QoL distinct from the PedsQL. Test–retest reliability at 2 weeks was very good (intraclass correlation coefficient [ICC] 0.85–0.95; 95% confidence interval 0.83–0.97) and good agreement was established between parent and child report (ICC 0.63–0.76).
Interpretation
The PSQLM demonstrates sound psychometric properties. Further research will seek to increase its clinical utility by reducing length and establishing responsiveness for descriptive and longitudinal evaluative assessment.
What this paper adds
- A pediatric stroke-specific quality of life (QoL) measurement tool for assessments based on perceptions of importance and satisfaction.
- Moderate-to-high reliability and validity established for a new clinical scale evaluating QoL among children with stroke.
- Perceived QoL measured using the Pediatric Stroke Quality of Life Measure appears lower in children with neurological impairment.
Resumen
esDesarrollo y validación de una herramienta de calidad de vida en accidente cerebrovascular pediátrico
Objetivo
Desarrollar y validar una medida parental especifica de enfermedad de calidad de vida (CDV) para pacientes de 2 a 18 años sobrevivientes a trombosis cerebral seno venosa (TASV) y accidente isquémico arterial (AIA)
Método
Utilizando métodos cualitativos y cuantitativos, desarrollamos un cuestionario de 75 items de calidad de vida de accidente cerebrovascular pediátrico (PSQLM – sigla en inglés). Enviamos el cuestionario y una medida de calidad de vida genérica estandarizada, inventario de calidad de vida pediátrico (PEDSQL) a 353 familias. Se documentaron el tipo de accidente cerebro vascular, edad del episodio y el resultado neurológico según el PSQLM. Calculamos la consistencia interna, validez confiabilidad del PSQLM.
Resultados
La tasa de respuesta fue del 29%, produciéndose una muestra de 101 pacientes (media de edad 9 años 9 meses, desviación estándar 4,30), 69 AIA (68,3%), 32 TASV (31,7%). La coherencia interna del PSQLM fue alta (chronbach a=0,94-0.97). La validez del contenido para PQSLM fue moderadamente robusta (r=0,3- 0,4; p menor 0,003), y como fue esperado la correlación con el PEDSQL fue moderado, sugiriendo que el PSQLM operacionaliza CDV diferente de PEDSQL, la fiabilidad del examen y repetición a dos semanas fue buena (coeficiente de correlación intraclase cci=0.85-0.95%, intervalo de confianza 0,83-0.97) y se estableció una buena concordancia entre el reporte parental y del niño (cci 0.63-0.76).
Interpretación
La PSQLM demuestra propiedades psicométricas sólidas. Investigaciones a futuro buscaran aumentar la utilidad clínica para reducir la duración y establecer la capacidad de respuesta para una evaluación longitudinal y descriptiva.
Resumo
ptDesenvolvimento e validação da medida de qualidade de vida para acidente vascular cerebral pediátrico
Objetivo
Desenvolver e validar uma medida de qualidade de vida (QV) a ser respondida pelos pais, que seja específica para uma doença, voltada para pacientes com idade de 2 a 18 anos sobreviventes de trombose sinovenosa cerebral (TSVC) e acidente vascular cerebral isquêmico (AVCI).
Método
Utilizando métodos qualitativos e quantitativos, nós desenvolvemos um questionário com 75 itens para Qualidade de Vida em Acidente Vascular Cerebral Pediátrico (PSQLM). Enviamos a PSQLM por correio, juntamente com uma medida padronizada genérica de QV, o Inventário Pediátrico de Qualidade de Vida (PEDSQL), para 353 famílias. O tipo de acidente, idade no momento do evento, e resultado neurológico segundo a Medida de Resultado para Acidente Vascular Cerebral Pediátrico foram documentados. Calculamos a consistência interna, validade e confiabilidade da PSQLM.
Resultados
A taxa de resposta foi de 29%, resultando em uma amostra de 101 pacientes (média de idade 9a9m[DP 4,3]; 69 AVCI [68,3%], 32 TSVC [31,7%]. A consistência interna da PSQLM foi alta (a de Cronbach=0,94–0,97). A validade de construto para a PSQLM foi moderadamente forte (r=0,3–0,4; p<0,003) e, como esperado, a correlação com o PEDSQL foi moderada, sugerindo que a PSQLM operacionaliza a QV de maneira distinta do PEDSQL. A confiabilidade teste-reteste no período de 2 semanas foi muito boa (coeficiente de correlação intraclasse [CCI] 0,85–0,95; intervalo de confiança 95% 0,83–0,97) e boa concordância foi estabelecida entre o relato dos pais e das crianças (CCI 0,63-0,76).
Interpretação
A PSQLM demonstra propriedades psicométricas adequadas. Futuras pesquisas buscarão aumentar sua utilidade clínica reduzindo o seu tamanho e estabelecendo a responsividade para avaliação descritiva e longitudinal.
What this paper adds
en
- A pediatric stroke-specific quality of life (QoL) measurement tool for assessments based on perceptions of importance and satisfaction.
- Moderate-to-high reliability and validity established for a new clinical scale evaluating QoL among children with stroke.
- Perceived QoL measured using the Pediatric Stroke Quality of Life Measure appears lower in children with neurological impairment.
This article is commented on by Steinlin on page 537 of this issue.
This article's abstract has been translated into Spanish and Portuguese.
Follow the links from the abstract to view the translations.
Abbreviations
-
- AIS
-
- Arterial ischaemic stroke
-
- CHP
-
- Centre for Health Promotion
-
- CSVT
-
- Cerebral sinovenous thrombosis
-
- ICC
-
- Intraclass correlation coefficient
-
- PedsQL
-
- Pediatric Quality of Life Inventory
-
- PSOM
-
- Pediatric Stroke Outcome Measure
-
- PSQLM
-
- Pediatric Stroke Quality of Life Measure
-
- QoL
-
- Quality of life
A stroke in infancy or childhood is especially traumatic for a child and the family because stroke is more unexpected during childhood. Population-based studies identify the annual incidence of paediatric arterial ischaemic stroke (AIS) as approximately 1.6 per 100 000 children,1 and of paediatric cerebral sinovenous thrombosis (CSVT) as 0.34 to 0.67 per 100 000 children.2 Child survivors of AIS or CSVT frequently experience neurological impairments and reduced function.3, 4 Studies of quality of life (QoL) using non-stroke-specific parent proxy and child report measures reveal varying degrees of reduced QoL in activities related to cognition, school, socialization, emotional function, and physical function.5-13 Furthermore, data are conflicting regarding the contribution of neurological outcome, socio-economic status, stroke type, and age at event to QoL. These discrepancies reflect differences in measurement approaches, how QoL is conceptualized and specific items included, whether enjoyment and importance are considered, or activities scored according to level function.14, 15 In addition, unconsidered cultural differences, exclusion of children with CSVT, variability in the primary information source utilized, and whether parent proxy or the child survivor themselves is questioned adds to the underlying discrepancies across research studies.16
While generic QoL tools are useful for comparing groups of children with different illnesses, disease-specific measurements offer superior content validity and clinical relevance. The latter are also more sensitive to longitudinal changes within individuals, a particularly important requirement in determining the outcomes of disorders that are acquired in infancy and early childhood. As learned from adult stroke populations, generic QoL measurement tools fail to assess elements of QoL related to cognition, language, and memory-issues of critical importance in stroke survivorship.17-19 A paediatric stroke-specific QoL measure would therefore be of benefit to informing research and clinical practice in this condition.
The development of disease-specific QoL tools for young patients requires attention to various conceptual and methodological issues unique to children.14, 20-23 Content must be applicable across many developmental stages and must accommodate changes in interests across early childhood through to adolescence. This can be achieved by developing separate tools for different age ranges or a single tool that allows rating of item applicability to each child. The proposed tool must also enable information gathering from primary caregivers, typically parents, who represent a necessary proxy for children too young to self-report.24, 25 Parents may be more accurate in their recall and observation of their child's QoL and may base their rating from a more fully mature perspective. However, when developing a QoL tool, it is important to validate parent proxy report against child self-report, to determine systematic bias.
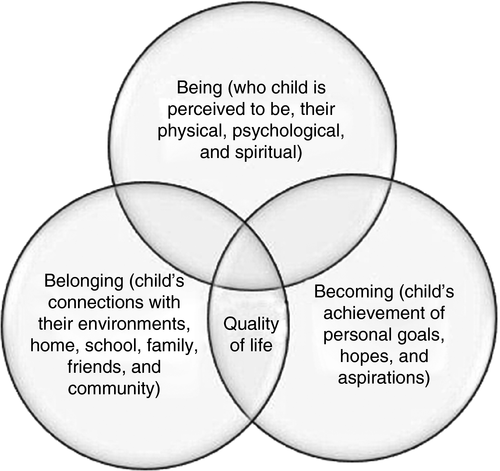
Finally, the conceptual framework upon which the tool is constructed is important to consider.26 The University of Toronto's Centre for Health Promotion (CHP) conceptual model of QoL is consistent with recent definitions of health and health promotion provided by the World Health Organization,27 and defines the term QoL as ‘the degree to which a person enjoys the important possibilities of his or her life’. The model is multidimensional, assumes that QoL is holistic in nature, and applies to all persons, across the lifespan, with and without disabilities. Measures of QoL derived from the CHP model emphasize both the relative importance of various aspects of life and the extent of the person's enjoyment of those aspects. This allows respondents to rate QoL items from an individualized perspective.28-30
This paper reports on the development and validation of the Pediatric Stroke Quality of Life Measure (PSQLM), a novel instrument for measuring the QoL of children after stroke. This study was conducted as part of the ongoing longitudinal multidisciplinary Stroke Outcome Project conducted at the Hospital for Sick Children in Toronto, Canada, since 1995. The Hospital for Sick Children ethics review board approved this project.
Method
Development of the PSQLM
The PSQLM items were developed based on qualitative content analysis derived from individual interviews with the parents of 44 child stroke survivors, and six adolescent survivors who were at least 16 years old at the time of the interview. Children with both CSVT and AIS were included; they were at least 1 year after stroke and ranged in age from 2 to 18 years. Forty-five per cent (n=20) of parents interviewed had children aged between 2 years and 5 years; 36% (n=16) had children aged between 6 years and 10 years; and 18% (n=8) had children aged between 11 years and 18 years. Interviews explored parent and child QoL perspectives and addressed theoretically derived research interests based on the CHP conceptual model of QoL. Interviewees explored parents’ personal definitions of QoL, factors that enhanced and diminished QoL for their child, and the impact of the child's stroke on QoL. Interviews were audio-recorded and transcribed in a format compatible for qualitative analysis using QSR NVivo 8 data software (QSR International Pty Ltd, Doncaster, Vic., Australia). Based on the analysis, a series of charts was created compiling emergent themes and frequency, and items and domains of concern. Items identified added to or reduced one's QoL and crossed a wide range of domains. Many of the items reflected common themes not exclusive to this population, such as family support, good health, and accessibility within the community environment. However, there were concerns seemingly unique to this population that parents described as reducing QoL, including ongoing stress associated with the stroke event and recovery, fear of recurrent strokes, and changes in their child's development and capacity to learn, pay attention, make decisions, and not being bullied by peers. Enhancing QoL was the experience of the stroke, which brought families closer together, becoming more appreciative of what it means to be healthy, having financial support, and appropriate therapies and school programmes, and opportunities to participate in sports. Additional issues identified in the paediatric stroke literature and by the institutional children's stroke medical team were included in the final analyses. Items were assigned to domains of QoL encompassed within the CHP conceptual framework for QoL,28-30 namely (1) ‘being’ (who the child is perceived to be); (2) ‘belonging’ (the child's connection to people and places); and (3) ‘becoming’ (the child's nurtured growth and development). Together these three domains encompass the conceptual framework for QoL. This framework guided our initial development of interview questions, and subsequent categorization of items into one of the three QoL domains (see Fig. 1).
After organization of the QoL items within the novel questionnaire, we pilot tested the drafted instrument with 10 parents of children with AIS/CSVT attending our institutional children's stroke clinic. Parents provided feedback on content relevance, missing issues, and question wording. The comments were used to revise the novel questionnaire, which then underwent further pilot testing with three additional parents of children with AIS/CSTV.
The final instrument, named the PSQLM, consists of 75 items, each written in statement form (see Appendices S1 and S2 [online supporting information] for items and questionnaire format). To describe the QoL experienced by the child we consider the domains and subdomains along two dimensions: importance of the area of life as perceived by the child and enjoyment experienced. A basic QoL score is determined by the interaction between importance and enjoyment scores.28-30
The instructions on the PSQLM direct parents first to check off “Not applicable” if the item does not apply to their child. All items that are checked off as not applicable (not developmentally, culturally, or age-appropriate) are not included in scoring. This process eliminated the need to produce distinct questionnaires according to age range as seen in other generic assessments.
Parents were instructed to rate each applicable item on a 5-point Likert scale separately for importance (from a score of ‘5’ [extremely important] to a score of ‘1’ [not at all important]) and enjoyment/satisfaction (from a score of ‘5’ [extremely satisfied] to a score of ‘1’ [not at all satisfied]).
Items ranked as high importance and high satisfaction (each ranked at 5/5), yield an item score of 10. Items ranked as high importance (score of 5) but low enjoyment/satisfaction yield an item score of –10. Items ranked of moderate importance (score of 3) with moderate satisfaction (score of 3) yield a QoL score of 0. An item rated as high importance (5/5) with moderate satisfaction (score of 3/5) would yield a QoL score of 0.
Overall QoL mean scores are calculated as the average of the converted QoL item scores for the total number of items that were completed (i.e. were applicable) out of the 75-item questionnaire. Subdomain scores for being, belonging, and becoming are based on the average converted QoL item scores for those items that fall within each of the three subdomains of QoL-Being, QoL-Belonging, and QoL-Becoming.
Participants
Children with AIS/CSVT were identified in the Canadian Pediatric Ischemic Stroke Registry – Toronto site. All children up to 18 years of age with a diagnosis of AIS or CSVT who had either consented (>16y) or assented (>8y) with parent consent were eligible to participate in the study if they understood written English. Diagnostic criteria were (1) for AIS, acute onset of a clinical focal deficit (or seizures alone for infants) and computed tomography or magnetic resonance imaging showing infarction conforming to an established arterial territory; and (2) for CSVT, headache, diffuse, or focal neurological deficit or seizure, and magnetic resonance venography or computed tomography venography showing thrombus within venous channels. A parent from each household and children 10 years of age and older were invited to independently complete a parent proxy or self-report version of the questionnaire respectively. We did not invite younger children (aged 2–9y) to complete the questionnaires as we had not adapted the language and instructions by creating child versions more appropriate for younger participants.
Socio-economic status calculation methods
Socio-economic data were retrieved from 2006 Canadian census data corresponding to participant postal codes using Beyond 20/20 version 7.0 (Beyond 20/20 Inc., Ottawa, Canada). Unique census subdivision identifier codes were derived from each participant's postal code using the Canadian Census Analyser Postal Code Conversion Files.31 This is necessary as the Canadian Census does not use postal codes as a geographical unit, and this step is required to allow matching of postal codes to census data, for which socio-economic status data could then be retrieved. Based on this methodology, average and median family incomes were captured for each participant based on their census subdivision.
Validation methods
The instrument validation phase consisted of a mail out of the PSQLM and the Pediatric Quality of Life Inventory (PedsQL) questionnaire. The PedsQL is a standardized, generalized pediatric QoL questionnaire for children aged 2 to 18 years.32 The PedsQL measures QoL in terms of the impact of disease on an individual's physical, emotional, and social functioning. In contrast, the PSQLM assessment is not function based as there are no questions about how well or poorly a child performs in any of the domains. We hypothesized that high correlations between these two measures would not be expected given the differences in how the term ‘quality of life’ is operationalized as a construct between measures.
Self-report and parent versions of the PSQLM were mailed to all 153 children in the study population aged 10 to 18 years, for validation with parent proxy reports. Questionnaires were premarked with unique identifications associated with the participant's clinical and demographic information, to enable matching with the database of the Canadian Registry. Families were provided a postage-paid envelope to return the questionnaires. A sample of 72 participants (randomly selected from the original sample of 353) was asked to complete two PSQLM questionnaires 14 days apart to enable test–retest reliability analysis. For those participants, a second copy of the PSQLM was enclosed in a separate sealed envelope with instructions to complete 2 weeks after they completed and mailed the first copy. Only participants who returned both the initial and retest questionnaires were included in the data analysis for test–retest reliability.
In all children with AIS/CSVT the neurological deficit after stroke was assessed with serial examinations utilizing the Pediatric Stroke Outcome Measure (PSOM) in the children's stroke clinic from 1995. The PSOM is a standardized outcome measure used by paediatric neurologists to determine the neurological deficits (sensory motor, language, cognitive) of children after ischaemic stroke.33 The most recent PSOM summary score at the time of questionnaire completion was utilized.
Psychometric analyses
Data were analysed using PASW Statistics 18, Release Version 18.0.0 (formerly SPSS, Chicago, IL, USA). Parametric statistics were used to analyse those variables that were continuous. Descriptive statistics were calculated to define demographic and clinical data, including mean, SD, and range. Independent analyses of variance were performed to identify variance in PSQLM and PedsQL according to the degree of neurological deficit measured with the PSOM.
To establish construct validity, we tested domain-specific correlations using Spearman's rho correlation coefficients (r) comparing scores between subdomains of the PSQLM and the generic PedsQL. These were: PSQLM-Belonging with PedsQL-Social functioning; PSQLM-Becoming with PedsQL-School functioning and PSQLM-Being with both PedsQL-Physical Functioning; and PedsQL-Emotional Functioning. Finally, we also tested correlations between the total PSQLM with the total PedsQL score. We hypothesized that high correlations between these two measures would not be expected given the differences in the operationalization of the construct of quality of life in the two measures.
The reliability coefficient for test–retest reliability was analysed using the intraclass correlation coefficient (ICC), which is a reflection of both the correlation and agreement between the initial test and retest scores.34 ICC was also calculated to determine reliability in ratings between children and their parent proxy.
Results
Respondents
Figure 2 shows the flow chart for the participants in the study. A total of 118 out of 353 (33%) packages were returned by mail. Of these, two were returned uncompleted with an attached note stating their child's ‘quality of life was fine’. Fifteen packages were returned unopened because of wrong addresses, leaving 101 of 353 (29%) valid returned packages.
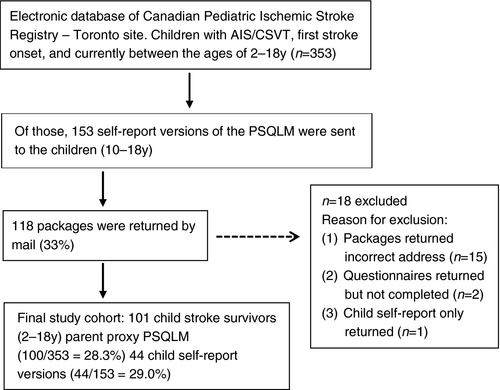
One hundred parents and, independently, 44 children (aged 10–18y) returned completed proxy or self-report versions of the PSQLM. Ninety-seven per cent of respondents completed all items on the questionnaire. Clinical and demographic characteristics of the children of parent respondents are given in Table 1.
| n (%) | |
|---|---|
| Age at stroke | |
| (1) Neonatal stroke: newborn–1mo (n=38) | 38/101 (37.6) |
| (2) Non-neonatal stroke: >1mo (n=63) | 63/101 (62.4) |
| ≥1mo and <1y | 16/63 (25.4) |
| ≥1 to <2y | 12/63 (19.0) |
| ≥2 to <5y | 18/63 (28.6) |
| ≥ 5 to <12y | 15/63 (23.8) |
| ≥12y and 18y | 2/63 (3.2) |
| Interval from stroke to QoL assessment (n=101) | |
| <1y | 1 (1.0) |
| 1–2y | 4 (4.0) |
| 2–5y | 40 (39.6) |
| >6y | 56 (55.4) |
| Stroke type (n=101) | |
| AIS | 69 (68.3) |
| CSVT | 32 (31.7) |
| Neurological deficit (PSOM final score, n=96) | |
| Good outcome | 46 (47.9) |
| No deficit (score of 0) | 31 (32.3) |
| Mild deficit (score of 0.5) | 15 (15.6) |
| Poor outcome | 50 (52.1) |
| Moderate deficit (score 1–2) | 26 (27.1) |
| Severe deficit (score 2.5–10) | 24 (25.0) |
| Combined household income ($) | |
| 10 000–25 000 | 10 (9.9) |
| 25 000–50 000 | 25 (24.8) |
| 50 000–75 000 | 16 (15.8) |
| 75 000–100 000 | 17 (16.8) |
| 100 000–150 000 | 15 (14.9) |
| >150 000 | 8 (7.9) |
- QoL, quality of life; AIS, arterial ischaemic stroke; CSVT, cerebral sinovenous thrombosis; PSOM, Pediatric Stroke Outcome Measure.
Most parent respondents were mothers (79.2%). Thirty-eight per cent (n=38/101) of the children were neonates at time of stroke. There were 69 (68%) children with arterial ischaemic-type stroke. There were 66 males (66%) and 35 (35%) females. Approximately half of the children had neurological deficits on the PSOM (52%), with moderate functional deficits in 27% and severe deficits in 25%. The mean age of the children of the parent proxy responders was 9 years and 9 months (SD 4.30). The average age of the children who completed PSQLM self-reports was 13 years and 6 months (SD 2.21). An average of 2 years 5 months had elapsed between the time the last PSOM was performed and the time of survey completion.
For test–retest reliability, 28 of 72 (39%) participants returned the initial PSQLM and 18 of 72 (25%) participants returned both the initial test and the retest. All questionnaires were completed by the same proxies initially and at retest, of which 15 of 18 (83%) were mothers. The mean age of children represented in the test–retest sample was 10 years and 9 months (SD 3.78).
PSQLM QoL scores
Descriptive statistics for the PSQLM overall QoL score and for the three subdomains of being, belonging, and becoming scores are given in Table 2. Using the scoring guidelines for the CHP's measure of QoL,28-30 scores that fell between 0.1 and 4.9 were coded as adequate QoL, greater than 5 as very good-to-excellent QoL, between 0 and –5 as poor QoL, and less than −5 as very poor QoL. Within the sample the ‘Overall PSQLM Parent Version QoL’ scores ranged from −6.69 to 9.78, and on the domains as follows: ‘being’ range −7.92 to 9.78; ‘belonging’ from −6.47 to 10.00; and ‘becoming’ from −5.91 to 10.00. These scores reflect that QoL was very good to excellent for some children, adequate for others, and poor or very poor for yet others. On the child version of the PSQLM the lower limit of the range of scores was not as severe as reported by parents. For the children overall PSQLM scores ranged between −1.91 to 9.45, with subdomains ranging from −2.39 to 10.00, suggesting that although QoL was perceived to be very good to excellent, some children did report a poor QoL. Scores on the PedsQL are interpreted on a scale of 0 to 100, with higher scores reflecting better QoL. Within our sample, PedsQL scores ranged from a low of 52.66 (SD 18.5), which reflects a moderately poor QoL, to a high of 87.17 (SD 11.18) reflecting a very good-to-high QoL.
| PSQLM subdomain | Parent proxy scores (n=100) | Child self-report scores (n=44) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Min | Max | Mean | SD | n | Min | Max | Mean | SD | |
| Being | 98 | −7.92 | 9.78 | 2.34 | 3.32 | 44 | −2.45 | 8.61 | 2.58 | 2.99 |
| Belonging | 98 | −6.47 | 10.00 | 3.53 | 3.70 | 44 | −2.39 | 9.72 | 3.91 | 3.39 |
| Becoming | 97 | −5.91 | 10.00 | 3.12 | 3.39 | 44 | −2.40 | 10.00 | 4.12 | 3.44 |
| Overall PSQLM | 99 | −6.69 | 9.78 | 3.03 | 3.28 | 44 | −1.91 | 9.45 | 3.56 | 3.14 |
- Min, minimum; max, maximum.
Mean total score on the PSQLM (F3,89=7.897, p<0.001) and PedsQL (F3,74=19.600, p<0.001) varied with the degree of neurological deficit as measured on the PSOM (Table 3). There was a trend towards decreasing scores (lower QoL) on both the PedsQL and the PSQLM with increasing neurological deficit. Although mean PSQLM scores fell within the average range (0.71–4.65), more patients with severe neurological impairment were reported to have QoL within the poor category. Mean total score on the PSQLM and PedsQL was not significantly correlated with age at stroke (p=0.422 and p=0.423 respectively).
| Neurological deficit (PSOM final score) | Mean (SD) PSQLM total score | Mean (SD) PedsQL total score |
|---|---|---|
| No deficit (0) | 4.65 (3.33) | 87.18 (11.18) |
| Mild deficit (0.5) | 3.44 (2.81) | 82.26 (14.99) |
| Moderate deficit (1–2) | 2.57 (2.36) | 72.24 (16.66) |
| Severe deficit (2.5–10) | 0.71 (3.06) | 52.66 (18.5) |
- There was a significant effect of neurological deficit on mean scores on the PSQLM (F3,89=7.897; p<0.001) and PedsQL (F3,74=19.600; p<0.001).
Reliability
As shown in Table 4, agreement between child-reported and parent-reported QoL scores based on 43 dyads (79.2% mothers) was moderate to excellent with ICCs ranging from 0.64 to 0.76. Test–retest reliability was excellent, with ICCs ranging from 0.91–0.94 (Table 5).
| PSQLM subdomain | Agreement (ICC) | |
|---|---|---|
| ICC | CI | |
| Being | 0.760 | 0.560–0.870 |
| Belonging | 0.639 | 0.337–0.840 |
| Becoming | 0.743 | 0.527–0.860 |
| Overall PSQLM | 0.758 | 0.555–0.869 |
- ICC, intraclass correlation coefficient; CI, confidence interval.
| PSQLM subdomain | n | ICC | CI |
|---|---|---|---|
| Being | 18 | 0.939 | 0.840–0.977 |
| Belonging | 18 | 0.914 | 0.774–0.967 |
| Becoming | 18 | 0.937 | 0.836–0.976 |
| Overall QoL score | 18 | 0.944 | 0.852–0.979 |
- Intraclass correlation coefficients (ICC) with confidence intervals (CIs) for quality of life (QoL) scores recorded on the PSQLM on two occasions, 2wks apart (n=18).
Internal consistency was excellent, with all ICCs exceeding 0.90 for the entire instrument (Cronbach's α=0.979, standardized α=0.986), and for each subdomain (being: α=0.954, standardized α=0.965; belonging: α=0.958, standardized α=0.969; becoming α=0.948, standardized α=0.964).
Validation
Construct validity was examined by Spearman's rho correlation coefficients (r). Results showed moderate correlations of PSQLM scores with domain-specific PedsQL scores, consistent with our a priori hypothesis that high correlations were not expected given the marked differences between measures in the operationalization of QoL. Specifically, correlations were, for belonging and PedsQL-Social functioning r=0.302 (p=0.003); for becoming and PedsQL-School functioning r=0.406 (p<0.001); for being and PedsQL-Physical Functioning r=0.375 (p<0.001); for being and PedsQL Emotional Functioning r=0.385 (p<0.001); and for overall QoL score and the PedsQL total score r=0.406 (p<0.001).
Content validation of questionnaire items was examined through consensus on validity of the selected items by parents of child stroke survivors and experts in the field. It was also assured by examination of the consistency of items within the three subdomains and overall PSQLM scores.
Discussion
In this study we developed a novel questionnaire of QoL for child stroke survivors and determined its validity and reliability. The themes identified through in-depth semi-structured interviews with parents of child stroke survivors and affected adolescents enabled the incorporation of a wide range of novel themes, and provided strong construct validation for the items included in the measure. Paediatric stroke is a relatively recent field of study and is not yet well understood by the public or health care personnel. Items included in the new measure are highly relevant to young age at the time of stroke and suggest a possible role for the PSQLM in other acquired focal brain disorders acquired during childhood. The concerns regarding other people's understanding of paediatric stroke, and the stress associated with the possibility of a recurrent incident are also highly relevant to the target disease, paediatric stroke. To our knowledge, these and many other disease-specific items in the PSQLM are not represented in generic measures of QoL.
The results on the PSQLM showed that mean overall QoL scores in this sample fell within the adequate range, as defined in the CHP guidelines and referred to in the ‘Results’ section above. Although there are no normative data as yet to compare these results to, the fact that the low range of scores reported by the children were not as low as reported by the parents suggests that children may perceive their own QoL to be better than their parents. Similar results have been reported in other studies. A distinct feature of the PSQLM is that each profile reveals an individualized assessment based on perceptions of importance and satisfaction. As a clinical tool the results may reveal large discrepancies for some patients between items that are important and their perceived enjoyment. It is these discrepancies that should be flagged by clinicians followed by further discussion with families and children for individualized support and the establishment of family-centred goals.
We classified the questionnaire items into domains consistent with the CHP model for QoL, namely being, belonging, and becoming. We also considered each individual's rating of importance and satisfaction in scoring each QoL item. This, along with the wide scope of items we included, provides a highly relevant approach across individuals with items of high importance, but poor satisfaction indicated the most significantly impaired QoL. This approach allows us to accommodate variability among individuals of varying ethnic, education, maturational, and socio-economic factors in a study group or clinical practice.
Initial findings comparing the PSQLM with neurological outcome shows that perceived QoL appears lower in some children with severe neurological impairment. It is not clear whether multiple neurological deficits equate with a lower perceived QoL, or if specific areas of poor neurological outcome (e.g. severe deficits in sensory motor) correlate with reduced QoL.
As a descriptive measure the development of the PSQLM was theory-driven, and shows good face and content validity and high internal consistency. The CHP theoretical model upon which the measure is based considers QoL in terms of importance and satisfaction. It is the ability of the PSQLM to quantify the discrepancy for items being highly important yet providing little satisfaction that characterizes the unique features of this measure. When administered at a group level, the identification of domains that are most frequently problematic provides important information for programme planning.
Our decision to construct a new measure of QoL, specific to child survivors of stroke, was based on our assumptions that no criterion standard existed. Current generic measures did not address QoL from a client-centred perspective; the importance of items are not considered when rating enjoyment and satisfaction. Furthermore, we found that concerns of parents specific to the needs of child survivors of stroke were not included in generic measures. Some of these items pertained specifically to coping and the stress associated with a sudden stroke during childhood, fear of recurrence, concern over limited finances, supports for therapies, school, and social well-being. Other issues reflected concerns described in other studies of QoL for typically developing and disabled participants. As a parent proxy measure of QoL, the items included demonstrate high relevance for child survivors. Further research requires validation of items for children, using child-friendly methods (i.e. puppetry, visual art, small-group activities) designed to elicit the thoughts of young people in terms of their own lives.
Construct validity showed moderate correlations of PSQLM scores with domain-specific PedsQL scores consistent with our a priori hypotheses; the two assessments approach the measurement of QoL from different perspectives, and, as such, moderate correlations support the fact that the PSQLM measures aspects of QoL not assessed in the PedsQL.
We observed that the internal consistencies for items in each subscale, as well as the entire instrument were highly acceptable. The PSQLM also demonstrated moderate-to-excellent parent proxy interrater agreement with paired child ratings. However, consistent with the findings of previous investigations, examination of mean QoL scores showed parents tended to rate their children's QoL as poorer than the children themselves.6 Thus, both parent proxy and, where feasible, child-reported PSQLM assessments remain independently important in evaluating QoL in childhood stroke.
Our findings suggest that preliminary test–retest results demonstrate very good stability of the instrument and consistency in the scores over time. This satisfies the critical psychometric property of reliability required for all measurement tools, in particular those that assess subjective constructs. The high reliability coefficient obtained on analysis provides evidence that the test scores, measured on different occasions, are reproducible and consistent over a 14-day interval. However, the response rate obtained for this component of the study (14.4%) was low and the results may not be representative of the total population. Participants may have forgotten to complete the retest questionnaire, which may explain the higher response rate for the initial copy, or there may have been a general lack of interest in participating in the study. The lack of representation at the extremes of the age ranges (i.e. 2–6y and 14–18y) also decreases the generalizability of the study. Finally, the mean retest interval for the study was larger than the expected interval of 14 days. As such, changes in scores may reflect true changes in QoL and not the reliability of the measure. Further studies with follow-up telephone calls may yield a larger sample size and age range, all required to further validate test–retest.
This satisfies the critical psychometric property of reliability required for all measurement tools, in particular those that assess subjective constructs. The high reliability coefficient obtained on analysis provides evidence that the test scores, measured on different occasions, are reproducible and consistent over a 14-day interval.
Although internal consistency and parent proxy and child agreements are strong for the PSQLM, several limitations caution the acceptance of our study's results. First, despite our attempt to maximize the response, our response rate was 29%. Participants may have anticipated that response would be too time consuming or otherwise inconvenient. Despite the low response rate, the study sample remains generally representative of the population of children with ischaemic stroke: demographic characteristics are similar to previously described samples.2, 9 The proportion of children with poor neurological outcome was slightly higher than previously described samples (i.e. 52.1% vs 41% reported previously),2 suggesting a mild respondent bias towards children with poorer neurological outcome. However, as children at all ranges of outcome were well represented in our sample, the impact on our study objective – reliability/validity testing – is likely minimal.
Although strong agreement between parent and child respondents was found, original questionnaire items were derived from interviews with parents and only a small group of adolescent stroke survivors. Therefore, the PSQLM may most accurately represent issues of concern to parents. Future studies could identify issues important to childhood stroke survivors by conducting an item generation phase with children. The resulting child-specific instrument would then be useful either as a primary measure for children able to self-report or as a complement to the parent proxy PSQLM.
The current version of the PSQLM is lengthy, particularly for use with repeated longitudinal assessments and research. It should be noted that the 75 items represent the developmental needs from toddlers to late adolescents (2–18y). When completed individually many items are excluded as they are not age-appropriate. Unlike other generic measures of QoL for children, the PSQLM, in its present form, does not include age-specific modules, thus reducing the number of items per age group
Future development of the PSQLM will focus on selectively reducing the number of items to increase the clinical utility of this questionnaire. Approaches for retaining only the most salient and independently informative questions will include elimination of items consistently rated as ‘not important’. Other methods may include the ‘clinical impact’ method of item reduction,35 or, if response data can be collected on sufficient additional populations, a factor analyses approach. Further research is also required to establish the responsiveness of the measure to document clinically significant change over time for use in interventional studies geared at improving QoL.
In summary, we have developed the first disease-specific QoL measure in childhood stroke and demonstrated its reliability and validity. The determination of QoL after childhood stroke is of paramount importance in order to clarify priority QoL treatment targets and inform the development of appropriate interventions. The PSQLM demonstrates sound psychometric properties as a comprehensive, descriptive assessment of QoL after paediatric stroke.
Acknowledgements
The authors have stated that they had no interests that might be perceived as posing a conflict or bias.




