Botulinum toxin A injections and occupational therapy in children with unilateral spastic cerebral palsy: a randomized controlled trial
Abstract
Aim
To investigate the effects of repeated botulinum toxin A (BoNT-A) injections combined with occupational therapy, including a splint, compared with occupational therapy alone on hand function in children with unilateral spastic cerebral palsy (USCP), in all International Classification of Functioning, Disability and Health (ICF) domains.
Method
This was a randomized controlled study, population-based and evaluator-blinded for primary outcome (October 2004 to September 2010). Twenty children (14 males; median age 3y 1mo) with USCP, recruited at a rehabilitation centre in Sweden, were assigned to one of two parallel groups using concealed allocation. In the course of one year, 10 children received occupational therapy, while 10 received repeated BoNT-A plus occupational therapy (BoNT-A/OT). Primary outcome (Assisting Hand Assessment [AHA]), and secondary outcome measures (range of movement [ROM], and Canadian Occupational Performance Measure), were measured at baseline, 3, 6, 9, and 12 months.
Results
AHA revealed a superior effect in the BoNT-A/OT group at 12 months: 6 out of 10 improved compared with 1 out of 10 in the occupational therapy group (p<0.03). A 95% Peskun exact confidence interval for the difference in proportions is given as 0.01 to 0.81. Secondary outcomes improved in both groups.
Interpretation
Repeated BoNT-A/OT appeared superior to occupational therapy alone for bimanual performance in young children with USCP. Active ROM and goal performance improved in both groups.
What this paper adds
- Botulinum toxin A, as an adjunct to occupational therapy, demonstrated superior outcomes for bimanual performance, while both groups improved in active ROM and goal performance.
- The effects increased and were sustained after repeated injections.
- The results, interpreted according to the smallest detectable difference, suggest a relevant effect.
This article is commented on by Russo on pages 702–703 of this issue.
Abbreviations
-
- AHA
-
- Assisting Hand Assessment
-
- BoNT-A/OT
-
- Botulinum toxin A plus occupational therapy
-
- COPM
-
- Canadian Occupational Performance Measure
-
- ICF-CY
-
- International Classification of Functioning, Disability and Health for Children and Youth
-
- ROM
-
- Range of movement
-
- SDD
-
- Smallest detectable difference
-
- USCP
-
- Unilateral spastic cerebral palsy
Hand function is central to the performance of many activities in daily life, involving the integration of the sensorimotor, visual, and cognitive systems. A child explores and interacts with their environment from early life and these systems progressively develop throughout childhood.1 Early damage to the brain, as in cerebral palsy (CP), may disturb the development of these skills.2 CP occurs in 2 per 1000 live births in western Sweden.3 More than one-third of the children have unilateral spastic CP (USCP).4
The performance of bimanual activities can be hampered by physical, cognitive, and perceptual factors. In USCP, one hand often has a reduction in the range and speed of movement, strength, coordination, sensation, and muscle tone, which reduces the ability to grasp and manipulate with the impaired hand.5 In the International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY), these factors are considered in the domain of body function/structure.6 However, these prerequisites are not the only determinants of the performance of an activity. The child's ability to participate in life situations is influenced by the demands of the activity. This is captured in the activity/participation domain of the ICF-CY, where the execution of the task is defined as ‘activity’ and the involvement in life situations is ‘participation’.
Occupational therapy is often designed to span all ICF domains. Interventions targeting range of movement (ROM) and bimanual activities are based on the principles of motor learning and cognitive-based motor intervention, and are effective in different settings. Occupational therapy is also used in combination with other interventions.7
One such intervention that is used to change factors in the body function/structure domain is injecting botulinum toxin A (BoNT-A) into selected muscles, resulting in a temporary reduction in spasticity. As the negative impact of spasticity decreases, occupational therapy may be more effective. In a Cochrane Review in 2010, a high level of evidence was found to support the use of BoNT-A as an adjunct to managing the upper limbs in children with spastic CP.7 It concluded that BoNT-A should be accompanied by occupational therapy and that further research was needed to evaluate repeated injections. Only a few studies have investigated the effects of repeated BoNT-A injections in combination with occupational therapy.8, 9 The importance of choosing instruments that are sufficiently responsive, covering all ICF domains, has been pointed out,9 and the present study is designed with this in mind. The concept of the smallest detectable difference (SDD) was also considered in the interpretation of the results.
The aim of this study was to evaluate and compare the effectiveness of repeated BoNT-A plus occupational therapy (BoNT-A/OT) versus occupational therapy alone on hand function in children with USCP. This is the first-year result of a 4-year study.
Method
Trial design
The study was a population-based, descriptive study with a parallel, randomized controlled design, with allocation ratio 1:1. The study was approved by the regional ethical review board at the University of Gothenburg and the Swedish Medical Products Agency and was registered with the Current Controlled Trials (ISRCTN84681422).
Participants
Children were recruited from the habilitation centres in Västra Götaland County, Sweden. Parents gave written consent before enrolment in the study.
Inclusion criteria were USCP with spasticity, typically distributed in the pronator muscles, thumb muscles, and elbow flexors, interfering with bimanual activity at age 18 months to 10 years.
Exclusion criteria were intellectual disability interfering with the intervention programme, upper limb dystonia, previous upper limb surgery and/or BoNT-A injections, or impaired hand function that was too mild and not appropriate for BoNT-A intervention.
Data were collected at the Regional Rehabilitation Centre, Västra Götaland, Sweden.
Interventions
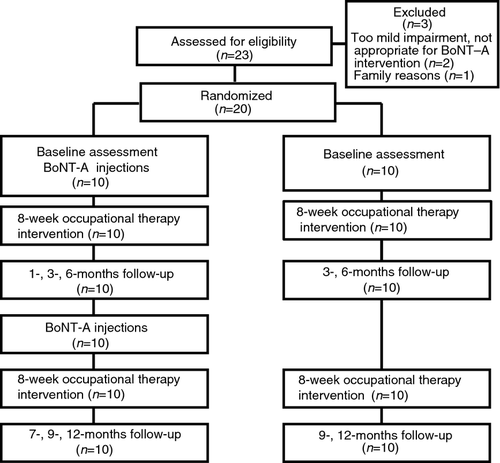
Both groups received occupational therapy, including a splint, and one group was additionally treated with BoNT-A (Fig. 1). BoNT-A injections were carried out 2 weeks before the two blocks of therapy. After the 8-week blocks of intervention, families were instructed to resume their usual therapy, but refrain from other interventions for upper limb.
Botulinum toxin
BoNT-A injections (Botox, Allergan Norden AB, Upplands Väsby, Sweden) were made under general anaesthesia or nitrous oxide sedation after local anaesthetic EMLA cream (AstraZeneca, Södertälje, Sweden) was applied to injection sites. Injections were guided with neuromuscular electric stimulation, using Teflon-coated Botox needles (37mm, 27gauge) diluted to 100 units per millilitre (U/mL). Doses per muscle: biceps brachii 15–30U/mL, brachialis 10–15U/mL, m. brachioradialis 10–15U/mL, pronator teres 10–20U/mL, pronator quadratus 5–20U/mL, adductor pollicis 5–10U/mL, and flexor pollicis brevis 3U/mL. Doses were calculated according to size of the muscle, body weight, and degree of spasticity.10
Occupational therapy home programme
Both groups participated in two 8-week blocks of therapy involving the implementation of a home programme and a weekly session with an occupational therapist. Bimanual training (56h in 8wk) of repetitive task practice and goal-directed activities was conducted combined with manual stretching (once a day) and the use of a static circular splint (8h per night). The splint was individually made, with the elbow flexed, the forearm in supination, and the thumb between radial and volar abduction. When 90° of passive supination was not possible, the splint was adapted 10° less from the child's maximum ROM (Fig. S1, supporting information online). The approach was in accordance with the programme by Novak.11 A logbook was used to document the treatment.
Outcome measures
Classifications according to House et al.12 and Zancolli et al.13 were performed at baseline. Neuroimaging was retrieved from register data.3, 4 Assessments were carried out at baseline, 3, 6, 9, and 12 months in both groups (Fig. 1). In addition, the maximum effect of BoNT-A was assessed at 1 and 7 months, and the parents were interviewed regarding adverse events.
Primary outcome measurement
ICF domain: activity/participation
The Assisting Hand Assessment (AHA) aims to measure the spontaneous use of the impaired hand during activities that require bimanual handling in children with unilateral upper limb impairment. It is a standardized, criterion-referenced test for children aged 18 months to 12 years. A play session is videotaped and scored according to how effectively the child uses the impaired hand in 22 items such as ‘reaches’, ‘changes strategy’, and ‘releases’.14, 15
Secondary outcome measurements
ICF domain: body function/structure
Active and passive ROM in elbow extension and supination of the forearm was measured in sitting position, with a standardized medical goniometer following standard procedures.16
ICF domain: activity/participation
The Canadian Occupational Performance Measure (COPM) is a client-centred instrument that helps identify problems in occupational performance and select goals in life situations. The COPM is responsive to change and has good validity and reliability. Scores are obtained for performance and satisfaction with performance, on a 0 to 10 rating scale.17, 18 Difficulties completing self-care, school/preschool, or leisure activities, such as putting on socks, are identified. In this study, the parents chose two goals, in relation to the injected muscles, the child's developmental level, and being potentially achievable within 8 weeks. It was conducted at baseline and at 6 months, and re-rated at 3 and 9 months.
Sample size
The study was population-based; the participants represented 20% of all children with USCP from their birth-year cohorts in the CP register of western Sweden. Based on clinical records and register information3, 4 of a total of 104 children with USCP, 19 had a cognitive impairment, 26 were already treated with BoNT-A or had undergone hand surgery, 36 were not appropriate for BoNT-A because of a mild impairment, and three exhibited signs of dystonia in addition to spasticity.
Randomization
The allocation sequence was generated by a third party who randomly mixed 20 envelopes containing group affiliation, which thereafter were sequentially numbered. Simple randomization was used. The envelopes were sealed and opaque, to achieve allocation concealment. As children were enrolled, the next envelope in the sequence was opened by the chief investigator (KH).
Blinding
Participants were aware of the group affiliation. The occupational therapist assessing primary outcome was blinded to group allocation and order of assessments.
Baseline measurements were performed on the day the child received BoNT-A, hence, it was not possible to blind assessors of secondary outcomes to group allocation. Secondary outcome measurements were performed by two occupational therapists, aware of the child's intervention but blinded to the previous results.
Statistics
Non-parametric tests were chosen, based on the small sample, and the fact that the majority of the variables were not normally distributed according to the Shapiro–Wilk test.
The primary outcome measurement was the proportion of children achieving an improvement in AHA score larger than the SDD between baseline and 12 months. The differences in number of improved children between the groups at 12 months were estimated with the N−1 χ2 test. In addition a 95% confidence interval (CI) for the difference in proportions was calculated, using the Peskun exact method. As a key secondary analysis, changes within the groups were analysed with a Wilcoxon signed-rank test with the 95% CI of the difference in medians at baseline and after 12 months. Descriptive statistics were used for baseline data and secondary outcome.
Missing data were managed by imputing the means of the measurements before and after the missing value for each individual child. The level of statistical significance was set at p<0.05. Statistical calculations were not adjusted for multiplicity.
Primary outcome measure
Raw AHA scores were converted into AHA units, which are logit-based, interval-level data.19 The primary objective was to compare between the groups. This was analysed according to the N−1 χ2 test, after dichotomising the AHA, that is five or more AHA units or fewer than five. SDD of 5 (0.97 logits)19 AHA units or more exceeded the error variance within the measure.
Secondary outcome measures
A change in ROM of more than 10° was regarded as a significant change based on a reliability study by Armstrong.20 Comparisons between the groups were made, after dichotomizing the ROM variable to more than 10° or 10° or fewer. A change in the COPM score of two points is a recommended cut-off for clinically significant change, based on several responsiveness studies.21 This variable was therefore dichotomized for two or more, or fewer, points.
Descriptive statistics were used to study the relationship between change in active supination and AHA units.
Results
Recruitment
Twenty-three children were assessed for eligibility (Fig. 1).3 Twenty children (14 males, 6 females; median age of 3y 1mo) were randomly assigned to one of two groups, with 10 children in each group. All the participants completed the study between October 2004 to September 2010. All BoNT-A injections were performed as scheduled.
Baseline data
There were no significant differences between the groups regarding baseline characteristics, including classification by House et al.12 and Zancolli et al.13 However, although not statistically significant, the BoNT-A/OT group started at lower levels in the case of AHA and ROM active supination. The distribution of neuroimaging results was similar to that of the total group of children with USCP in the area (Table 1).4
| Groups | ||
|---|---|---|
| BoNT-A/OT | Occupational therapy | |
| Baseline characteristics | (n=10) | (n=10) |
| Sex, females/males | 3/7 | 3/7 |
| Median age, mo | 35 | 37 |
| Affected side, right/left | 4/6 | 3/7 |
| House functional system | ||
| 1 | 6 | 8 |
| 2 | 3 | 2 |
| 3 | 1 | 0 |
| 4 | 0 | 0 |
| Zancolli system | ||
| 1 | 7 | 8 |
| 2A | 1 | 1 |
| 2B | 2 | 1 |
| 3 | 0 | 0 |
| Neuroimaging characteristics | ||
| Normal findings | 1 | 0 |
| Basal ganglia lesion | 2 | 0 |
| Cortical/subcortical lesion | 3 | 5 |
| Periventricular white-matter lesion | 3 | 4 |
| Maldevelopment | 0 | 1 |
| Baseline measures median (Q1; Q3a) | ||
| AHA (score in units) | 51 (43; 69) | 55 (46; 65) |
| ROM (degrees) | ||
| Forearm supination, (affected hand) | ||
| Active | −10 (−65; 0) | 25 (−20; 62) |
| Passive | 88 (75; 90) | 88 (75; 90) |
| Elbow extension (affected hand) | ||
| Active | −8 (−10; 0) | −28 (−63; −20) |
| Passive | 0 (−3; 0) | 0 (0; 0) |
| COPM (number of goals) | 20 | 20 |
- aLower and upper quartile. AHA, Assisting Hand Assessment; BoNT-A/OT, botulinum toxin A plus occupational therapy; COPM, Canadian Occupational Performance Measure; ROM, range of movement.
Numbers analysed
All children attended the weekly clinic-based treatment sessions for 8 weeks and the home programmes were followed (56h in 8wk), according to the logbooks. All primary outcome assessments were performed, except for one child at 7 months. Secondary outcome measures had missing values for all assessments in active supination in one child. Active elbow extension differed between the groups at baseline; however, there were missing data regarding this variable in 6 out of 20 children at baseline.
Outcomes
Primary outcome
ICF domain: activity/participation
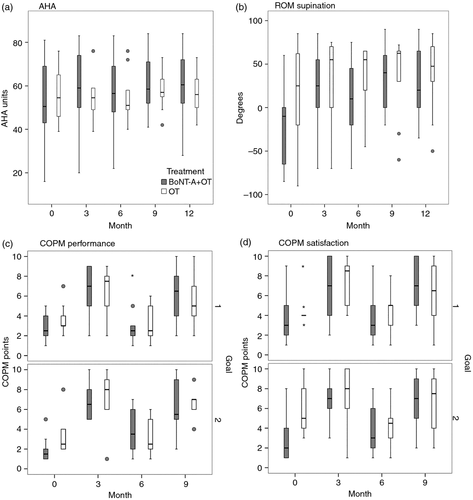
The BoNT-A/OT group improved compared with the occupational therapy group at 12 months. The AHA score increased by a median of 7.5 AHA units from baseline to 12 months in the BoNT-A group (95% CI 2.5–12.0) and with a median of 0 AHA units in the occupational therapy group (95% CI −3.5 to 8.0) (Fig. 2, Fig. S2a, b [supporting information online], Table 2). There were no missing values. Improvement was found in 6 out of 10 participants by ≥5 AHA units in BoNT-A/OT group and in 1 out of 10 in the occupational therapy group (p<0.03). A 95% CI of the difference in the proportion of improved patients was given as 0.01 to 0.81.
| Measure | Group | Baseline | 1mo | 3mo | 6mo | 7mo | 9mo | 12mo | Median differencea |
|---|---|---|---|---|---|---|---|---|---|
| Primary outcome | |||||||||
| AHA | BoNT-A/OT | 51 (16 to 81) | 51 (16 to 84) | 59 (20 to 83) | 57 (22 to 83) | 52 (32 to 84) | 59 (41 to 84) | 61 (28 to 84) | 7 |
| Occupational therapy | 55 (39 to 76) | 55 (39 to 76) | 51 (40 to 76) | 57 (42 to 73) | 56 (42 to 73) | 1 | |||
| Secondary outcome | |||||||||
| ROM | |||||||||
| Active supination forearm | BoNT-A/OTb | −10 (−85 to 60) | 0 (−85 to 85) | 25 (−70 to 85) | 10 (−70 to 75) | 55 (−50 to 83) | 40 (−20 to 90) | 33 (−35 to 90) | 22 |
| Occupational therapy | 25 (−90 to 85) | 55 (−70 to 75) | 55 (−45 to 65) | 63 (−60 to 72) | 48 (−50 to 85) | 15 | |||
| Passive supination forearm | BoNT-A/OT | 88 (55 to 90) | 90 (50 to 90) | 90 (60 to 90) | 90 (45 to 90) | 90 (75 to 90) | 90 (70 to 90) | 90 (50 to 90) | 0 |
| Occupational therapy | 88 (50 to 90) | 90 (60 to 90) | 85 (50 to 90) | 0 (50 to 90) | 90 (70 to 90) | 0 | |||
| Active extension elbow | BoNT-A/OTc | −8 (−30 to 0) | −10 (−28 to 0) | −14 (−25 to 0) | −8 (−22 to 0) | −5 (−20 to 0) | −5 (−50 to 0) | −3 (−15 to 0) | 5 |
| Occupational therapyd | −28 (−75 to −5) | −15 (−33 to −5) | −15 (−45 to 0) | −13 (−40 to 0) | −13 (−35 to 0) | 22 | |||
| Passive extension elbow | BoNT-A/OT | 0 (−5 to 0) | 0 (−5 to 0) | 0 (−10 to 0) | 0 (−15 to 0) | 0 (−5 to 0) | 0 (−15 to 0) | 0 (−10 to 0) | 0 |
| Occupational therapy | 0 (−25 to 0) | 0 (−5 to 0) | −3 (−15 to 0) | 0 (−12 to 0) | 0 (−12 to 0) | 0 | |||
- aMedian difference of 12mo scores minus baseline. bMissing value from one child at baseline, 1, 3, 9, and 12mo. c(n=4) and d(n=2) missing data at baseline.
The scores for AHA items ‘proceeds’, ‘changes strategy’, ‘reaches’, and ‘releases’ increased at 12 months in the BoNT-A/OT group compared with baseline and, in the occupational therapy group, the score for ‘orients objects’.
Five of the six children in the BoNT-A/OT group who improved ≥5 AHA unit, also improved in active supination and reached 0°, all increasing by 25° or more. In the occupational therapy group, 1 out of 10 improved, increasing by 35°, but did not reach 0° (Fig. S3a, b], supporting information online).
Secondary outcomes
ICF domain: body function/structure
In ROM active supination, both groups improved. At 12 months, 9 out of 9 participants in the BoNT-A/OT group and 6 out of 10 in the occupational therapy group had improved by >10°. The active supination increased by a median difference of 22° in the BoNT-A/OT group and 15° in the occupational therapy group from baseline to 12 months (Fig. 2, Table 2).
In ROM passive supination, at 12 months, 3 out of 10 participants in the BoNT-A/OT group and 1 out of 10 in the occupational therapy group had improved by >10°.
In ROM active extension of the elbow, at 12 months, 1 out of 6 in the BoNT-A/OT group and 6 out of 8 in the occupational therapy group had improved by >10°.
In ROM passive extension of the elbow, at 12 months, 0 out of 10 in the BoNT-A/OT group and 1 out of 10 in the occupational therapy group had improved by >10° (Table 2).
Missing baseline data for active elbow extension: BoNT-A/OT (n=4) and occupational therapy (n=2).
ICF domain: activity/participation
In COPM, both groups had improved after each treatment block at 3 and 9 months (Fig. 2).
In performance, both the BoNT-A/OT group and the occupational therapy group improved. At 3 months, the first goal improved by 7 out of 10 for the BoNT-A/OT group versus 8 out of 10 for the occupational therapy group; and the second goal by 10 out 10 versus 8 out of 10. At 9 months, the first goal improved by 7 out of 10 versus 7 out of 10; and the second by 8 out of 10 versus 7 out of 10.
In satisfaction, both the BoNT-A/OT group and the occupational therapy group improved. At 3 months, the first goal improved by 7 out of 10 for the BoNT-A/OT group versus 7 out of 10 for the occupational therapy group; and the second by 10 out of 10 versus 6 out of 10. At 9 months, the first goal improved by 7 out of 10 versus 6 out of 10 and the second by 8 out of 10 versus 6 out of 10 (Fig. 2).
The most frequent goals, 64 out of 80, prioritised by parents in the COPM were related to self-care, followed by play, mobility, and leisure. The goals were similar for both groups; however, play-related goals were only found in the BoNT-A/OT group (9/40).
Safety
There were no adverse events after the BoNT-A injections reported at parent interviews 1 month after injection or documented in medical files.
Discussion
This population-based randomized controlled study demonstrated that BoNT-A/OT, as well as occupational therapy alone, result in improvement in active ROM and goal performance in young children with USCP. The patients receiving BoNT-A/OT had superior outcomes compared with occupational therapy alone for bimanual performance. Thus, only the combined treatment model resulted in improvements in all ICF domains. The results were analysed to reflect the SDD, the smallest amount of change that can be seen above the threshold of error expected in the measurement. A change larger than the SDD level was considered relevant in the current study. Measuring the minimal clinically important difference is desirable, but also more complicated. The SDD of the AHA19 was established by the author. Active supination was considered to be a change of more than 10°, according to Armstrong et al.20 A difference of two points is considered to be a clinically relevant change for the COPM according to Law et al.18 and Carswell et al.21 This concept provided an opportunity to detect a relevant change in all ICF domains.
Repeated injections combined with training appeared to have a positive effect. Lowe et al. reported similar findings.8 Active supination was increased immediately after the first block of intervention, in both groups, to some extent maintained at the start of block two. Starting at a higher point in the second block of intervention, a maximum effect was seen at 9 months, mostly maintained at 12 months. No similar finding of increased active supination has been reported previously. The use of a night splint, designed to stretch the pronator muscles and used several hours per night may have contributed to the beneficial effect, especially in those who did not receive BoNT-A. A similar result was seen in the AHA in the BoNT-A/OT group in terms of increased bimanual ability. The AHA scores increased in the BoNT-A/OT group and were maintained after 12 months. At 6 months, the scores were higher compared with baseline and, consequently, the participants started at a higher level in the second block. Their score still increased in the last block, indicating increasing performance over time and results lasting longer than the effects of the drug. The child with CP needs time to learn effective strategies finally to reach the autonomous stage.1 It can be speculated that the decrease in muscle tone after BoNT-A provided the window of opportunity the child needed to facilitate the use of the impaired hand and perform bimanual activities of enhanced quality, while, in the occupational therapy group, the absence of improvement was the result of sustained muscle tone. Other studies show unchanged results22 after occupational therapy, but also improvement.23 The study design often differs, making comparisons difficult.9 The majority had a maximum passive ROM at baseline, and a ceiling effect therefore occurred.
Five of the six participants in the BoNT-A/OT group, who maintained their improvements in the AHA score at 12 months, also improved in active supination. This is consistent with the statement by Braendvik et al., suggesting that active supination is a contributory factor in the performance of bimanual activity.24 Six participants in the BoNT-A/OT group and three in the occupational therapy group were unable to actively supinate the forearm to 0° at baseline. Therefore, three more children had the opportunity to reach 0° in the BoNT-A/OT group. This may be one of many reasons explaining improvements in the AHA score in this group.
Both groups improved in individual goal achievement measured by the COPM. Goal-setting was essential in the clinical decision-making.25 The parents prioritized the majority of their goals in the self-care category, consistent with other studies.9 The children were too small to be able to select goals themselves that were sustainable over time.
Goal-directed training increased performance, regardless of the therapy model. Increased ability in a larger number of activities was also enhanced by improving the overall bimanual skills. In the current study, this occurred only when BoNT-A was added.
Limitations of this study were the small sample, the simple randomization, and the partially unblinded design, where participants were aware of their group allocation. Only 20% of the total group with USCP in this geographical area were eligible to be part of the study, according to our detailed knowledge also of those who were not included. The small study size limits generalization of the results. The improvement in active ROM and goal performance in the occupational therapy group is difficult to interpret because of the lack of a non-treated control group; however, this was not considered to be ethical. Moreover, it is important to note that the difference in active supination between the groups at baseline may have been of clinical importance.
To study the effects of early interventions on a long-term basis, the participants will be monitored for 3 years.
Everyday life includes a variety of activities requiring bimanual ability. This small study compared the effectiveness of BoNT-A/OT versus occupational therapy alone for young children with unilateral CP. Both interventions demonstrated improvements in active ROM and goal performance, but BoNT-A, as an adjunct to occupational therapy, demonstrated a superior effect on bimanual performance. BoNT-A/OT may be considered when the objective is to improve bimanual ability in daily life.
Acknowledgements
We sincerely thank the participating children and families, occupational therapists Kristina Olsson and Karin Lindh, and the occupational therapists at the habilitation centres. Göran Carlsson PhD and Catrin Wessman PhD who assisted with statistical calculations. This study was funded by the Norrbacka-Eugenia, the Folke Bernadotte and the Petter Silfverskiöld Memorial Foundations, the Sunnerdahl Handikappfond, and the Research and Development Boards for Gothenburg & Södra Bohuslän and Västra Götaland. The authors have stated they had no interests that might be perceived as posing a conflict or bias.