Wearable technology to monitor hand movement during constraint-induced movement therapy for children with cerebral palsy
K9
E Sabelhaus1, B Goodwin2, K Bjornson3, K Pham4, W Walker5, K Steele6
1Seattle Children's Hostpital, Whatcom Center for Early Learning, Seattle, WA, USA; 2University of Washington, Seattle, WA, USA; 3Pediatrics, Seattle Children's Research Institute, University of Washington, Seattle, WA, USA; 4Seattle Children's Hospital, University of Washington, Seattle, WA, USA; 5University of Washington School of Medicine, Seattle Childrens Hospital, Seattle, WA, USA; 6University of Washington Mechanical Engineering, Seattle, WA, USA
Background and Objective(s): Constraint-Induced Movement Therapy (CIMT) is an evidence based treatment for children with hemiplegic cerebral palsy (CP). While CIMT has been shown to improve hand function in CP, the protocol and results are often variable and its long-term impact on hand use in daily life remains unclear [1–2]. The goal of this research was to quantify hand use in clinical and home environments before, during, and after CIMT. We hypothesized that paretic hand use would increase during CIMT, with enhanced bimanual use in activities of daily living after CIMT.
Study Design: Case Series.
Study Participants & Setting: 8 children with hemiplegic cerebral palsy undergoing CIMT (age: 3 yr 5 m - 9 yr 2 m, 4 boys/4 girls) and 5 typically-developing (TD) children (age: 2 yr 8 m - 9 yr 10 m, 1 boy/4 girls) were recruited from a pediatric tertiary care facility.
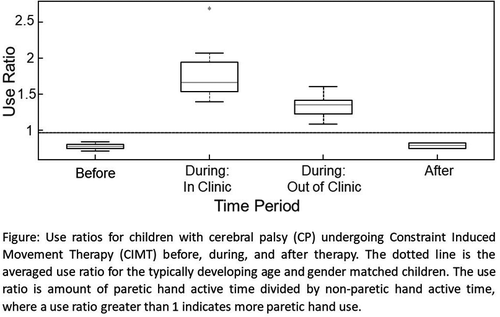
Materials/Methods: Per the institution's CIMT protocol, the non-paretic hand of each child in the CP cohort was placed in a cast for three weeks. Unilateral hand training of the paretic hand occurred 2 hours/day, 4 days/week. Bimanual training occurred 2 hours/day once a week. The CP cohort wore ActiGraph GT9X Link (ActiGraph Corp., Pensacola, FL) tri-axial accelerometers on both wrists for 3 consecutive days during 3 time periods: 1-week before, during, and 6–8 weeks after CIMT. Functional tests (grip strength and Box & Blocks) and the Canadian Occupational Performance Measure (COPM) were conducted before and after CIMT. The TD cohort did not receive any therapy, but wore the Actigraph accelerometers on both wrists for 3 consecutive days at home, spaced to align with the CP cohort time periods. Accelerometry data was analyzed via a use ratio; amount of paretic hand active time divided by non-paretic hand active time [3], where a use ratio greater than 1 indicates more paretic hand use.
Results: Paretic hand use increased both in clinic and at home during CIMT compared to pre-therapy values (use ratio: pre=0.77±0.04; during (in clinic)=1.77±0.36; during (home environment)=1.33±0.14). Comparatively, the TD use ratio (home environment) was 0.96±0.04. After CIMT, the CP cohort scored higher on paretic hand functional measures: grip strength increased by 7.5±4.9 lbs., the number of blocks transferred in 60 seconds increased by 3.5±6.6 blocks, and COPM scores increased 5±2.8 points. However, 6–8 weeks after CIMT ended, paretic hand use returned to pre-CIMT levels (use ratio: pre=0.77±0.04; post=0.79±0.06).
Conclusions/Significance: CIMT increased paretic hand use during the therapy period, both in and out of the clinic. However, the subsequent return to pre-intervention bimanual hand use measured by accelerometry data indicates that further interventions (i.e. a larger dose of CIMT) or strategies may be needed to maintain increased daily paretic hand use after CIMT.
References:
[1] DeLuca et al. (2017) Pediatr Rehabil
[2] Brauers et al. (2017) Pediatr Rehabil
[3] Lang et al. (2017) JoVE