Gel-immersion-assisted endoscopic injection sclerotherapy under observation with Texture and Color enhancement imaging for esophageal varices
Abstract
Watch a video of this article.
BRIEF EXPLANATION
Intravascular endoscopic injection sclerotherapy (EIS), an effective treatment for esophageal varices (EVs), is technically more challenging than endoscopic variceal ligation (EVL).1 In conventional EIS, gas insufflation reduces the EV diameter, making the puncture harder and less precise. To address this issue, gel immersion EIS (GI-EIS) has recently been developed.2-4
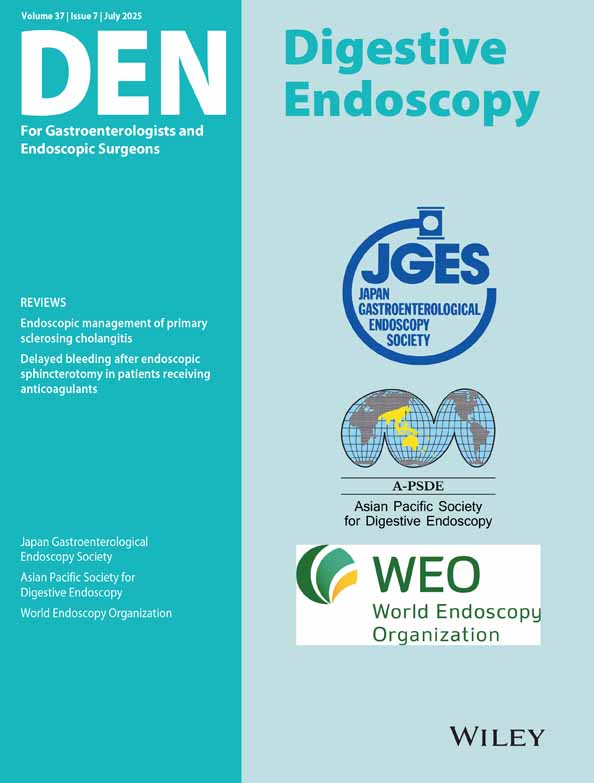
GI-EIS offers several advantages. Retaining the gel within the esophageal lumen ensures a clear and stable endoscopic field while reducing the esophageal wall tension, preserving the variceal diameter, and facilitating sclerosing agent injection (Figure 1). However, reduced mucosal tension surrounding EVs can sometimes make them appear less prominent, posing challenges in selecting the optimal puncture site.
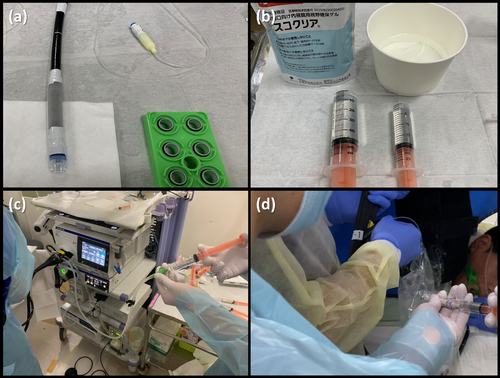
To overcome this limitation, we hypothesized that EIS using texture and color enhancement imaging (TXI) would improve EV visibility and ameliorate the precision of puncture point selection compared with white-light imaging. TXI (Mode 1) optimizes three key image factors – texture, brightness, and color – thereby improving lesion contrast and visualization.5 Based on this concept, we developed GI-EIS under TXI observation, referred to as “GI-EIS under TXI” (Video S1).
We conducted GI-EIS under TXI in 15 prophylactic cases between September 2023 and October 2024. The high success rate (93.3%) of GI-EIS under TXI can be attributed to the synergistic effects of gel immersion and TXI-enhanced imaging. The gel-immersion maintained the variceal diameter by preventing luminal collapse, while TXI improved visualization of the varices by enhancing texture and contrast. This allowed for precise puncture site selection. Additionally, gel-immersion suppressed peristalsis and minimized esophageal wall tension. These factors collectively contributed to the successful injection (Figure 2).
Authors declare no conflict of interest for this article.
ACKNOWLEDGMENTS
We thank Dr. Jun Nakamura, Dr. Minami Hashimoto, Dr. Ryoichiro Kobashi, Dr. Mitsuru Otsuka, Dr. Daiki Nemoto, and Professor Hiromasa Ohira for their invaluable contributions to postoperative patient management and insightful advice on article preparation. We also thank the entire medical staff at the Department of Endoscopy, Fukushima Medical University Hospital, for their dedicated assistance with the endoscopic procedures.