WEO Newsletter and Contents
The mission of the WEO Outreach Committee is to expand endoscopic services to populations in need worldwide. To do so, the Committee, chaired by Dr. James DiSario, strives to introduce, re-introduce and/or supplement endoscopic equipment, services, training and education in areas of need, and to promote WEO activities in the region.
Donations of endoscopic equipment and supplies are solicited from industry, foundations, and other organizations. Collaboration with national and international medical associations is sought. Eligible recipient sites must have limited or no endoscopic services available for underserved populations. Absolute requirements are that the facility serves the public, there is one or more trained endoscopists available, there is appropriate spaced and facilities for proper use of the donated equipment, there are nursing and technical personnel available who are, or can be trained for endoscopy support, and there is a committed budget for supplies, accessories and maintenance. Sites that provide endoscopic training are strongly preferred. Candidate sites are identified by the Committee and our industry sponsors, and must submit an application, which is reviewed by the committee. Once a donation is made, one or more WEO representatives will travel to the site to review the facility, participate in an inaugural ceremony, and provide an educational program. The recipients must agree to comply with WEO guidelines, file annual reports of endoscopic utilization and outcomes, and continue participation with WEO activities. There are currently 10 Outreach Centers in Latin America and Africa (Fig. 1).

Professor Bougouma and staff of the WEO Outreach Center in Burkina Faso.
The WEO Africa Program is an Outreach Sub-committee chaired by Professor Ibrahim Mostafa to represent the special needs and interests of African endoscopy including enhancing and expanding endoscopic services, education, and training. Other Outreach activities include the Program for Endoscopic Trainers (PET) with the initial meeting held in Hyderabad, India in January 2013. This provides training in teaching skills for endoscopy educators in a retreat environment. Future programs are anticipated. The WEO/Pentax symposia on ‘How to Get Published in the International Endosocopy Literature’ was held in San Diego, California in during Digestive Disease Week in May 2012, and at the XXXIII Pan American Congress in Panama City, Panama in November 2012. There have also been two live demonstration and hands-on courses held in under the direction of Dr. Carlos Robles-Medranda June 2012 and 2013 at the Outreach Center in Guayaquil, Ecuador.
Center of Excellence
This month WEO highlights the endoscopy unit at the Prince of Wales Hospital in Hong Kong, China, one of the founding members of the WEO Centers of Excellence Group. The Prince of Wales Hospital is the teaching hospital of the Faculty of Medicine of The Chinese University of Hong Kong. They are responsible for nurturing healthcare professionals and spearheading medical research. So far, over 5,000 healthcare professionals have been trained. The hospital and the university work in close collaboration to provide patients with comprehensive service of the highest quality. Each year the Endoscopy Unit helps organize an international workshop on therapeutic endoscopy as well as several research projects under the auspices of WEO.
The following video was captured at the 1995 course. In this video, Dr Peter Cotton, MD (Charleston, SC, USA) places a plastic stent into an obstructed bile duct. Dr Cotton goes through this basic therapeutic ERCP procedure step-wise, offering the trainee and experienced endoscopist alike hints on smooth and effective plastic biliary stent placement. It particularly demonstrates the importance of coordination between the endoscopist and an experienced nurse or technician.
Follow this link to view the video:
http://www.worldendo.org/weo-video-201302.html
Endoscopic terminology – MST at work (the iPEN initiative)
The standardization of endoscopic nomenclature is a vital element in the work to improve communication of endoscopic findings, between endoscopists, as well as to the referring physician. The Minimal Standard Terminology project was started to facilitate this process, and has recently gained momentum through the increased efforts by WEO. This is the WEO initiative for Proper Endoscopic Nomenclature (iPEN) which will encourage all endoscopists to use the same descriptive MST language to report their findings. The complete documentation of the terminology is available at the WEO website.
Lars Aabakken
Chairman, Committee of Documentation and Stadardization
Image of the month
Gallstone (Fig. 2)
| Ductal pathology: Stone | |
|---|---|
| Attribute | Attribute value |
| Location | Lower common bile duct |
| Number | Multiple |
| Size | 18mm |
| Obstructing | No |
|
Comments: The filling defect seen in the distal common bile duct is most likely a stone (calculus). However, tumor is also in the differential diagnosis. If the filling defect can be shown to be mobile (on fluoroscopy or serial static images), then it cannot be a fixed lesion like a tumor. Blood clot can occasionally masquerade as a stone, and is mobile. However, the presence of blood or blood clot exiting the duodenal papilla (hemobilia) is a big clue to this rare finding. Other rare biliary filling defects include parasites, such as Fasciola hepatica, bile duct varices and mucus from mucus-secreting biliary tumors |
|
| Submitted by | Lars Aabakken |
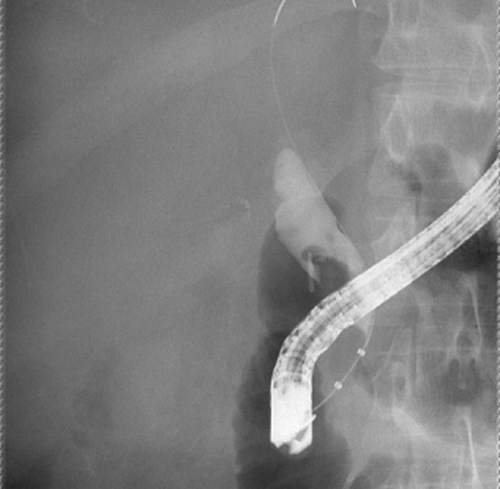
Image of the month.
Syllabus: True Confessions by The Expert
By John Baillie
This article is abstracted from ENDOFEST meeting of the American Society for Gastrointestinal Endoscopy (ASGE)
A popular topic at the annual ENDOFEST meetings of the American Society for Gastrointestinal Endoscopy (ASGE) has been ‘True Confessions by The Expert’. Everyone likes to hear about experts' disasters, which usually have an important learning point or two. In the attached presentation, I present two ERCP-related cases. The first shows the dangers of performing procedures on patients you don't know, and the second reminds us to think outside the box when the imaging and laboratory findings don't ‘fit’ the expected diagnosis. Mea culpa!
Please follow this link to view the presentation:
http://www.worldendo.org/assets/newsletters/201310/baillie_true_confessions.pdf
Brainteaser
By John Baillie
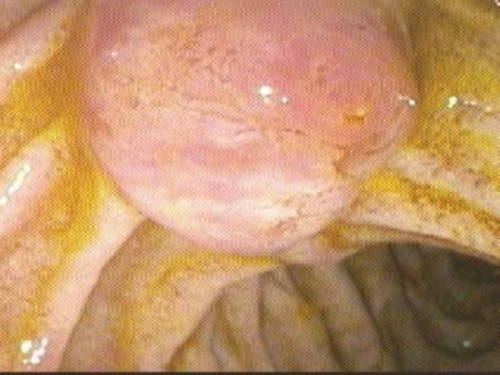
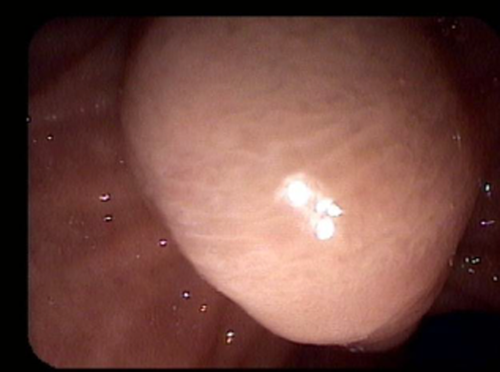
The smooth, symmetrical swelling seen in Figure 3 was an incidental finding in a 30 year old female undergoing endoscopy (EGD) for abdominal pain. The figure was captured using a video duodenoscope. The abnormality was found on the medial wall of the second part of the duodenum.
Brainteaser.
- a) ‘Windsock’ (everted) diverticulum
- b) Ampullary adenoma
- c) Swollen duodenal papilla due to an obstructing stone
- d) Choledochocele (Type III choledochal cyst)
Answer: (D) Choledochocele (Type III choledochal cyst)
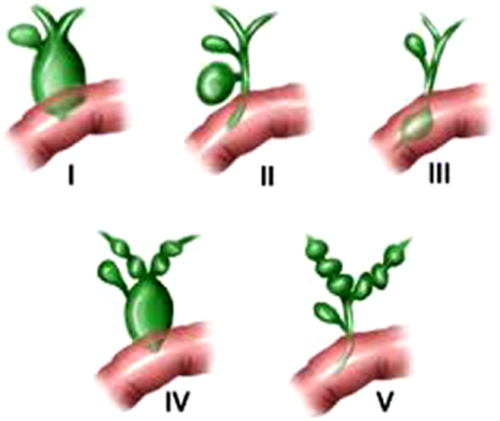
A symmetrical, smooth-surfaced mass protruding into the second part of the duodenum from the expected position of the main duodenal papilla is most likely to be a choledochocele, a Type III choledochal cyst in the Todani Classification (Fig. 4). An ampullary adenoma has a more ‘frondy’ (surface-structured) appearance (Fig. 5). Choledochal cysts are associated with risk of cholangiocarcinoma (primary bile duct cancer), but the risk is lowest in those with the Type III variety (choledochocele). These lesions are often amenable to therapeutic endoscopy: incision of the cyst using a needle knife papillotome often normalizes previously impaired flow of bile and pancreatic juice.