Natural orifice transluminal endoscopic surgery (NOTES) for clinical management of intra-abdominal diseases
Abstract
Clinical research on natural orifice transluminal endoscopic surgery (NOTES) has been increasingly reported over the past 5 years and more than 1200 patients have received various NOTES procedures. The present article reviews the clinical practice of NOTES for the treatment of intra-abdominal diseases, and was carried out through systematic search with specific keywords in major databases for NOTES-related clinical literature. The last date of the search was 15 August, 2012. Transvaginal cholecystectomy is the commonest NOTES procedure reported, and its clinical feasibility and safety was established through prospective case series and randomized trials. There is a regional difference in NOTES development with the majority of NOTES fromCaucasian countries being transvaginal cholecystectomy and most reports from Asian countries being NOTES-related procedures. Safe closure of gastrointestinal access remains challenging, and novel endoscopic instruments are essential to enhance future development of NOTES.
Introduction
Natural orifice transluminal endoscopic surgery (NOTES), a concept of managing surgical conditions using a flexible endoscope, emerged as a novel development combining minimal invasive surgery and endoscopy. The aim of NOTES is not only to achieve no scarring, but to enhance postoperative recovery with reduction in pain and disturbance to immunological and physiological functions.1, 2 The feasibility of transgastric endoscopic peritoneoscopy (TG-Per) has been examined in pigs using ordinary endoscopic instruments.1 Numerous NOTES procedures have been investigated in animal experiments including cholecystectomy, hysterectomy, hernia repair and obesity surgery. However, translation of these experiences into human NOTES has been difficult. Rao and Reddy reported the success of the first transgastric appendectomy,3 and currently over 1200 human NOTES procedures have been reported.4-9 The present article focuses on reviewing the clinical development of NOTES for the management of abdominal surgical diseases.
Methods
An electronic literature search was conducted on databases including MEDLINE, EMBASE, Cochrane controlled trials registry (CENTRAL) and Google Scholar to identify publications on clinical abdominal NOTES procedures. The last date of search was 15 August, 2012. The following keywords were used: natural orifice transluminal endoscopic surgery OR NOTES OR natural orifice surgery; transluminal OR transgastric OR transvaginal OR transanal OR transrectal OR transcolonic. Boolean operator ‘AND’ was used for combination of two searching sentences. After the initial search, reference lists of articles were browsed to further identify eligible studies. Criteria for studies to be recruited were: (i) clinical study on human natural orifice transluminal endoscopic surgery (NOTES) or NOTES-related procedures; (ii) study focused on intra-abdominal NOTES procedures; (iii) study reported details of NOTES procedure and perioperative outcomes, including postoperative complications and mortality; (iv) studies published in English.
All the studies included were categorized on level of evidence according to the criteria of Oxford Centre for Evidence-Based Medicine 2011 (http://www.cebm.net). Procedure-related complications were classified by a four-level grading system.10 Levels 1 and 2 were categorized as minor complications, and levels 3 and 4 were categorized as major complications. Literature searching, data assessment and judgment of severity of complications were conducted by two authors (PWYC and LL) independently, and disagreements were discussed until a consensus was reached.
Results and Discussion
Overview of clinical applications of NOTES
Figure 1 shows a list of publications on clinical NOTES published from 2007 to 2012. The first clinical NOTES procedure was reported in 2007 when two prospective series examined the feasibility and safety of transvaginal cholecystectomy.11, 12 Over the past decade, NOTES has been translated into clinical procedures including transvaginal endoscopic cholecystectomy (TV-Chole), TG-Per and transgastric endoscopic cholecystectomy (TG-Chole).5, 7, 13-15
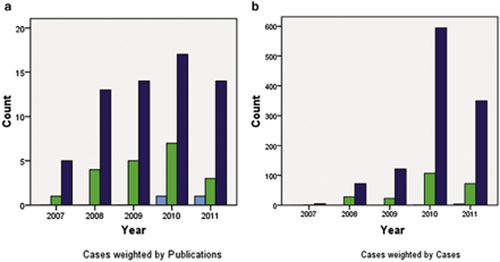
Clinical studies of human intra-abdominal natural orifice transluminal endoscopic surgery (NOTES) conducted from 2007 to 2011. (a) No. publications; (b) no. patients in each year of publication.  , TR-NOTES, transrectal NOTES;
, TR-NOTES, transrectal NOTES;  , TG-NOTES, transgastric NOTES;
, TG-NOTES, transgastric NOTES;  , TV-NOTES, transvaginal NOTES.
, TV-NOTES, transvaginal NOTES.
Transgastric NOTES
Transgastric NOTES (TG-NOTES) is the second most common clinical procedure reported (Fig. 1). TG-NOTES was initially the preferred approach by endoscopists and surgeons as the stomach usually harbors minimal flora and renders minimal risk of intra-peritoneal contamination. Upon literature search, however, only 20 clinical studies were published on TG-NOTES. These procedures included TG-Per,2, 7, 8, 15, 16 cholecystectomy,2, 3 appendectomy, fallopian tube ligation3, 17 and gastrojejunostomy.18
Clinical experience in transgastric NOTES
TG-NOTES for peritoneoscopy
A total of 103 patients underwent TG-Per in 11 clinical studies3-9, 19-22 (Table 1). Indications for TG-Per were staging peritoneoscopy for carcinoma of the pancreas, carcinoma of the stomach and patients undergoing morbid obesity surgery. After peritoneoscopy, most of the gastrotomies were included as part of the surgical procedure or used for gastrojejunostomy to eliminate risk of leakage.7, 8, 21, 22 Nine patients had closure of gastrotomy using endoclips (seven cases) or T-tags (two cases).3, 5, 8, 9 Four patients sustained abdominal wall injuries and five had liver injury during opening of gastrotomy.22 One patient developed major complications with pneumothorax as a result of injury to the left lung from T-tag puncture.8 Although all these complications were successfully managed, the risk of transgastric NOTES should not be underestimated. Apparently, these complications were related to creation or closure of gastrotomy suggesting better access and closure methods should be developed.17 Narula et al. compared the accuracy of diagnostic laparoscopy to transgastric peritoneoscopy.21 Ten patients with pancreatic cancer underwent both diagnostic laparoscopy and TG-Per independently to detect peritoneal metastasis. The mean time for TG-Per was 18 min and that for laparoscopy was 7.2 min. The findings were consistent between the two groups with eight patients diagnosed with operable cancer and two with unresectable malignancy. Two studies reported the combination of diagnostic laparoscopy and TG-Per for surgical decision.4, 6 Thorough examination and biopsy of upper abdominal quadrants especially over the right lobe of the liver was inadequate with TG-Per. Nikfarjam et al. explored the optimal site for creation of gastrotomy in eight patients.7 Gastrotomy was created in the gastric body, lesser curvature, greater curvature, fundus and antrum. The right upper and lower quadrants were well visualized with TG-Per in all cases. Observation of the left upper quadrant, especially over the spleen, was difficult unless the gastrotomy was created over the greater curvature. These studies illustrate that TG-Per is limited by the design of the endoscope, location of gastrotomy, as well as the method of secure closure.
| Author (Ref.) | Country | Publication year | No. cases | NOTES (Pure/Hybrid) | Operative time mean (min) | Gastrotomy closure | Success rate (%) | Complications (cases, n) | Biopsy | |
|---|---|---|---|---|---|---|---|---|---|---|
| Minor | Major | |||||||||
| TG-Per | ||||||||||
| Zheng et al.9 | China | 2011 | 5 | Mixed | 98 | Clips | 100 | 0 | 0 | Yes |
| Nau et al. 22 | USA | 2011 | 40 | Pure | 18 | N/N | 100 | 9b | 0 | No |
| Park & Bergstrom8 | Sweden | 2010 | 2 | Pure | N/A | T-tag | 100 | 0 | 1c | No |
| Nikfarjam et al.7 | USA | 2010 | 8 | Hybrid | N/A | N/N | 100 | 0 | 0 | No |
| Nau et al.6 | USA | 2010 | 20 | Hybrid | 21 | N/N | 100 | 0 | 0 | Yes |
| Lee et al.5 | Korea | 2010 | 1 | Pure | 30 | Clips | 100 | 0 | 0 | Yes |
| Narula et al.21 | USA | 2009 | 10 | Hybrid | 18 | N/N | 100 | 0 | 0 | No |
| Steele et al.20 | USA | 2008 | 3 | Hybrid | 4a | N/N | 100 | 0 | 0 | Yes |
| Rao et al.3 | India | 2008 | 3 | Pure | N/A | Clips | 100 | 0 | 0 | Yes |
| Hyder et al.19 | USA | 2008 | 1 | Hybrid | N/A | N/N | 100 | 0 | 0 | No |
| Hazey et al.4 | USA | 2008 | 10 | Hybrid | 25 | N/N | 100 | 0 | 0 | Yes |
| TG-Chole | ||||||||||
| Horgan et al.23 | USA | 2011 | 4 | Hybrid | 270 | g-Prox | 100 | 0 | 0 | N/A |
| Zorron et al.15 | Multi-country | 2010 | 29 | Hybrid | 111 | Lap. | 86.2 | 2d | 5e | N/A |
| Salinas et al.24 | USA | 2010 | 27 | Hybrid | 137 | Lap. | 96.3 | 0 | 4f | N/A |
| Dallemagne et al.2 | France | 2009 | 5 | Hybrid | 150 | Lap. | 100 | 0 | 0 | N/A |
| TG-App | ||||||||||
| Zorron et al.15 | Multi-country | 2010 | 14 | Hybrid | 136 | Lap. | 92.9 | 2g | 1h | N/A |
| Park & Bergstrom8 | Sweden | 2010 | 1 | Hybrid | 150 | T-tag | 100 | 0 | 0 | N/A |
| Horgan et al.25 | USA | 2009 | 1 | Hybrid | 150 | g-Prox and Lap. | 100 | 0 | 0 | N/A |
| Rao et al.3 | India | 2008 | 10 | Pure | N/A | Clips | 80 | 2i | 0 | N/A |
- a Does not include time taken to create gastrotomy.
- b Nine cases of burn injury.
- c One case of pneumothorax because T-tag was placed into the left thoracic wall.
- d One case of esophageal hematoma and one case of umbilical port infection.
- e Included epiploic bleeding, esophageal laceration, perforation, mediastinitis, and postoperative peritonitis.
- f Included bleeding, esophageal laceration, perforation, and abdominal sepsis.
- g One case of appendix vessel bleeding and one case of ileus.
- h One case of abdominal wall injury.
- i One case of burn injury and one case of postoperative ileus.
- g-Prox, g-ProxTM Tissue Approximation Device (USGI Medical, Inc., San Clemente, CA, USA); Lap., gastrotomy was closed by laparoscopy; Mixed, included two cases of hybrid TG-Per and three cases of pure TG-Per; N/A, not available; N/N, gastrotomy was resected or used for gastrojejunostomy; NOTES, natural orifice transluminal endoscopic surgery; TG-App, transgastric endoscopic appendectomy; TG-Chole, transgastric endoscopic cholecystectomy; TG-Per, transgastric endoscopic peritoneoscopy.
Transgastric endoscopic cholecystectomy
Cholecystectomy is one of the commonest surgical procedures carried out worldwide and, naturally, TG-Chole became a targeted procedure. In order to carry out safe cholecystectomy, essential steps included exposure of Calot's triangle, and secure control of the cystic duct and artery. After review of the literature, the majority of TG-Chole required at least one transabdominal port which renders the procedure a hybrid laparoscopic-endoscopic cholecystectomy. Gastrotomies were created through endoscopic methods under direct visualization from laparoscopy and closed with laparoscopic suturing. Gallbladder >2 cm generally required retrieval through an abdominal port, as retrieval of a large gallbladder through the esophagus can be difficult.15, 24 Four pilot studies reported 65 cases of TG-Chole which confirmed the feasibility and safety2, 15, 23, 24 (Table 1). Another large-scale multi-center study involving 16 centers from nine countries included 362 patients who underwent various NOTES procedures.15 Of these, 29 patients had hybrid TG-Chole. The mean operative time was 111 min and hospital stay was 38 h. There were three cases of conversion, one to open cholecystectomy and two to laparoscopic cholecystectomy because of bleeding from gastroepiploic vessels and hindrance of dissection from large gallstones, respectively. In two patients with large gallstones where the gallbladder failed to be removed through the esophagus, one was stuck at the proximal esophagus for 150 min whereas another sustained esophageal perforation. Salinas et al. reported 27 patients who had TG-Chole between 2007 and 2009.24 Gastrotomy was created by modified percutaneous endoscopic gastrotomy (PEG) technique. The mean operative time was 137 min, and patients resumed diet immediately after surgery and were discharged 2 h later. The overall morbidity was 18.5% (5/27) with no mortality. Hemorrhage over the greater curvature occurred during gastrotomy in one patient and required conversion to open surgery for hemostasis. These studies illustrated that although TG-Chole is feasible, failure of specimen retrieval through the esophagus can lead to catastrophic complications. Moreover, a transgastric approach to the gallbladder is difficult as endoscopic dissection was done only in the retroverted position.
Transgastric endoscopic appendectomy and other interventions
Four clinical studies with 26 cases of TG-App have been reported3, 8, 15, 25 (Table 1). Similar to TG-Chole, most appendectomies were carried out in a hybrid fashion. Rao et al. reported the first case series of TG-App where eight of ten cases were done by using a pure transgastric approach.3 Park and Bergstrom reported three cases of acute appendicitis diagnosed by TG-Per, and one of them had appendectomy by using a hybrid TG-App approach.8 Although two patients sustained minor complications, one patient had a major complication of abdominal wall injury related to the creation of gastrotomy. Because of the difficulty in manipulating the transgastric endoscope to the right iliac fossa, two cases were converted to open surgery. Horgan et al. explored the feasibility of TG-App in two patients using a novel incisionless operating platform (IOP).25 Postoperative clinical outcomes were excellent without complications. The authors commented that a flexible multi-tasking operating platform is essential for carrying out transgastric NOTES.
Summary of complications related to transgastric NOTES
Among the reported clinical studies, the commonest complications from transgastric NOTES were injury to adjacent organs and esophageal laceration (Table 2). There were 10 injuries to the anterior abdominal wall during gastrotomy, indicating the risk of blind creation for gastric access.15, 22 Numerous measures were proposed to minimize risk of injury to adjacent organs, including creation of pneumoperitoneum prior to gastrotomy as well as transgastric puncture under endoscopic ultrasonographic guidance.26 Prior creation of PEG followed by transgastric access would be another safe method without the use of laparoscopy. There was no report on leakage from gastrotomy, as the majority of these were closed by laparoscopic suturing or included as part of the surgical procedures.6, 15, 24 Although numerous methods of gastrotomy closure have been developed, most were investigated in preclinical studies only.27 Esophageal perforation is a serious complication related to retrieval of the gallbladder.15 Preoperative ultrasonic measurement of gallstone size may predict the success of specimen extraction through the esophagus.28 With the limited number of clinical studies, transgastric NOTES in humans should be practiced with caution.
| Key steps of transgastric NOTES | Potential complications | Possible reasons | Cases (n) (Ref.) | Methods potentially contributing to reduced risk |
|---|---|---|---|---|
| (A) Passing endoscope through esophagus and extraction of specimen via esophagus | Esophageal hematoma, laceration and perforation, mediastinitis | Narrow space of esophagus, large specimen (diameter >2 cm), no suitable endoscopic instruments for procedure | 615, 21 | Ultrasound assessment of specimen size, small specimen (diameter <2 cm), optimal instruments for NOTES, laparoscopic assistance (hybrid fashion) |
| (B) Gastrotomy creation and closure |
(I) Creation of gastrotomy: burn injury of abdominal wall or adjacent organs, bleeding of gastric vessel, bowel injury. (II) Closure of gastrotomy: gastric leakage, injury of surrounding organs |
Blind creation and closure of gastrotomy, no suitable instruments for secure creation and closure of gastrotomy, no criteria for selection of optimal puncture site, intra-abdominal adhesion | 133, 8, 15, 21, 22, 24 | Ultrasound for identification of suitable puncture site, laparoscopic assistance (hybrid fashion), no closure of gastrotomy by gastrojejunostomy, creation of pneumoperitoneum, no history of abdominal surgery, suitable endoscopic instruments |
| (C) Cholecystectomy/Appendectomy | Bile leakage, bleeding, injury of visceral organs | No optimal endoscopic instruments/platform for use | 215, 24 | Laparoscopic assistance (hybrid fashion), multi-tasking platform, suitable endoscopic instruments |
| (D) Peritoneal infection | Localized or diffused peritonitis, peritoneal abscess | Gastrointestinal contents into peritoneum via gastrotomy during operation, gastric leakage | 115 | Prophylactic antibiotics, gastric irrigation, antiseptics and sterilization of endoscopy and all instruments |
- NOTES, natural orifice transluminal endoscopic surgery.
Transvaginal NOTES
Transvaginal surgery has been carried out by gynecologists for more than 100 years. Compared to other accesses, transvaginal NOTES achieves an excellent alignment to the supracolic compartment, and closure of transvaginal access can be done under direct visualization. More than 60 clinical studies have been reported on transvaginal NOTES, including peritoneoscopy, cholecystectomy, appendectomy and nephrectomy29, 30 (Fig. 1).
Clinical experience in transvaginal NOTES
Transvaginal endoscopic cholecystectomy
Forty-three studies have been reported on TV-Chole3, 11-15, 24, 25, 30-64 (Table 3). Transvaginal cholecystectomy has been exponentially increasing from nine cases in 2007 to 375 cases in 2011.35, 63 Because of the lack of a multi-tasking platform and specific instruments, only 11 cases were carried out as pure transvaginal NOTES.3, 32, 33, 50, 52, 57 The majority received a transvaginal port inserted through the posterior fornix. In a technical review, transvaginal access was mostly used for the introduction of a flexible endoscope for carrying out gallbladder dissection and extraction.30, 31, 34, 40, 41, 49, 56-58 However, ligation of the cystic duct and artery was done using surgical clips, as endoclips were not designed to completely occlude a tubular structure.
| Study (Ref.) | Country | Publication year | No. cases (n) | NOTES (Hybrid/Pure) | Mean operative time (min) | Clip application | Success rate (%) | Complications (n) | Hospitalization | |
|---|---|---|---|---|---|---|---|---|---|---|
| Minor | Major | |||||||||
| Zorron et al.14 | Brazil | 2008 | 4 | Hybrid | 77 | End. | 100 | 0 | 0 | 2 days |
| Forgione et al.46 | Italy | 2008 | 3 | Hybrid | 136 | Lap. | 100 | 0 | 0 | 2 days |
| Rao et al.3 | India | 2008 | 3 | Pure | N/A | End. | 100 | 0 | 0 | N/A |
| Ramos et al.13 | USA | 2008 | 32 | Hybrid | 38 | Lap. | 97 | 0 | 0 | 6 h |
| Rossi et al.47 | Italy | 2008 | 3 | Hybrid | 97 | Lap. | 100 | 0 | 0 | N/A |
| Zornig et al.48 | Germany | 2008 | 20 | Hybrid | 62 | Lap. | 100 | 0 | 0 | 2 days |
| Asakuma et al.49 | France | 2009 | 10 | Hybrid | 116 | Lap. | 100 | 0 | 0 | 2 days |
| de Sousa et al.32 | Brazil | 2009 | 4 | Pure | 210 | End. | 100 | 0 | 0 | 1 day |
| Navarra et al.36 | Italy | 2009 | 6 | Hybrid | 52 | Lap. | 100 | 0 | 0 | 1 day |
| Noguera et al.31 | Spain | 2009 | 15 | Hybrid | 90 | Lap. | 100 | 1 | 0 | 20 h |
| Gumbs et al.52 | USA | 2009 | 4 | Mixed | 209 | Lap. & End. | 100 | 0 | 0 | 23 h |
| Palanivelu et al.37 | India | 2009 | 8 | Hybrid | 148.5 | End. | 75 | 0 | 1 | 4 days |
| Linke et al.53 | Switzerland | 2010 | 102 | Hybrid | 62.3 | Lap. | 98 | 7 | 1 | 3.3 days |
| Salinas et al.24 | USA | 2010 | 12 | Hybrid | 147 | Lap. | 100 | 0 | 1 | 3 h |
| Federlein et al.41 | Germany | 2010 | 117 | Hybrid | 61 | Lap. | 98 | 2 | 3 | 2.8 days |
| Zorron et al.15 | Multi-country | 2010 | 240 | Mixed | 96 | N/A | 100 | 14 | 3 | 1.9 days |
| Pugliese et al.54 | Italy | 2010 | 18 | Hybrid | 75 | Lap. | 100 | 0 | 1 | 2.2 days |
| Hackethal et al.42 | Germany | 2010 | 13 | Hybrid | 88 | Lap. | 92 | 0 | 0 | N/A |
| Kilian et al.59 | Germany | 2011 | 15 | Hybrid | 68 | Lap. | 100 | 0 | 1 | 3 days |
| Cuadrado-Garcia et al.56 | Spain | 2011 | 25 | Hybrid | 90 | Lap. | 100 | 2 | 0 | 1 day |
| Hensel et al.58 | Germany | 2011 | 80 | Hybrid | 80 | Lap. | 100 | 0 | 2 | 3 days |
| Niu et al.60 | China | 2011 | 43 | Hybrid | 87 | Lap. | 100 | 0 | 0 | 2.7 days |
| Zornig et al.35 | Germany | 2011 | 100 | Hybrid | 52 | Lap. | 100 | 0 | 1 | 2.1 days |
| Roberts et al.61 | USA | 2011 | 20 | Hybrid | 71 | Lap. & End. | 100 | 0 | 0 | 1 day |
| Santos et al.64 | USA | 2012 | 7 | Hybrid | 162 | Lap. & End. | 100 | 1 | 0 | 1 day |
| Linke et al.62 | Germany | 2012 | 27 | Hybrid | 59 | N/A | 100 | N/A | N/A | N/A |
| Noguera et al.63 | Spain | 2012 | 20 | Hybrid | 65 | End. | 100 | 1 | 0 | 1 day |
- a Case reports are not included in this table.
- Lap. & End., clipping cystic duct and artery by using endoscopy (End.) or laparoscopy (Lap.); Mixed, both hybrid and pure TV-Chole were carried out; N/A, not available for article; NOTES, natural orifice transluminal endoscopic surgery; TV-Chole, transvaginal endoscopic cholecystectomy.
A randomized controlled trial was conducted comparing conventional laparoscopic, hybrid transvaginal and hybrid trans-umbilical cholecystectomy in 60 patients.63 The operative time was significantly longer for the transvaginal group compared to the laparoscopic and trans-umbilical groups (64.85 vs 59.80 vs 47.04 min for TV-Chole vs trans-umbilical group vs laparoscopic group). There was no conversion for transvaginal cholecystectomy, whereas one case in the trans-umbilical group converted to the laparoscopic group as a result of difficult dissection. There was no difference between the three groups in terms of postoperative pain and recovery. Another prospective match-pair study compared hybrid transvaginal against conventional laparoscopic cholecystectomy in 216 patients.35 The mean operative time was 52 min for the transvaginal group and 35 min for the laparoscopic group (P < 0.001). Average hospital stay was 2.1 days for the transvaginal group and 2.3 days for the laparoscopic cholecystectomy group. One patient developed pelvic abscess after transvaginal cholecystectomy and required laparoscopic drainage. Postoperative interview at 3 to 10 months showed that transvaginal access did not affect sexual intercourse. A prospective study compared TV-Chole against single-port and laparoscopic cholecystectomy in 51 patients.59 Although the operative time of TV-Chole was significantly longer, patients who underwent TV-Chole had less pain after operation. A survey on perception of laparoscopic and TV-Chole indicated that only 4% of females preferred TV-Chole, mostly worrying about disturbance of sexuality and fertility.65 Clinical application of TV-Chole is limited by gender and general scepticism in carrying out surgery through the vagina. The majority of TV Chole were reported in Western countries, illustrating a potential cultural influence on NOTES development.
Transvaginal endoscopic appendectomy and other interventions
Only a few cases of transvaginal appendectomy have been reported.15, 66, 67 Palanivelu et al. reported two cases of hybrid transvaginal appendectomy and one case of pure transvaginal appendectomy in 2008.67 The mean operative time was 103.5 min and hospital stay was 2 days. Other transvaginal NOTES procedures included hernia repair, nephrectomy, splenectomy, and sleeve gastrotomy.68-72 In 2008, Ramos et al.13 reported four cases of hybrid sleeve gastrotomy for morbid obesity using a 10-mm 45-degree rigid bariatric laparoscope passing through a 12-mm transvaginal trocar and two transabdominal ports. Operative time ranged from 90 to 100 min and all patients were discharged on postoperative day 2. Transvaginal obesity surgery might have an advantage over the laparoscopic approach as insertion of a laparoscopic port through the obese abdominal wall could be difficult.
Summary of the complications related to transvaginal NOTES
Forty patients (approximately 4.5%) sustained complications from transvaginal cholecystectomy, including 29 minor and 11 major complications (Table 4). Of the major complications, five had bile leakage and two had bowel injuries.15, 24, 37, 41, 54 Most of the bile leakage required re-operation. Refinements in surgical techniques and instrumentations in transvaginal NOTES may help to prevent these complications.
| Study (Ref.) | Complications (cases, n) | Treatment | |
|---|---|---|---|
| Minor | Major | ||
| Noguera et al.31 | Mild hematuria (1 case) | 0 | Conservative treatment |
| Palanivelu et al.37 | 0 | Bile leakage (1 case) | Conservative treatment |
| Linke et al.53 | Minor gynecological complication (4 cases), urinary retention and urinary tract infection (3 cases) | Small umbilical access hernia (1 case) | Re-operation and conservative treatment |
| Salinas et al.24 | 0 | Colon injury (1 case) | Re-operation |
| Federlein et al.41 | Vaginal bleeding (1 case) and slight rectal trauma (1 case) | Perforation of urinary bladder (1 case), bleeding in the fossa vesicae felleae (1 case) and bile leakage (1 case) | Re-operation and conservative treatment |
| Zorron et al.15 | Intraoperative cystic artery bleeding (5 cases), vaginal laceration (3 cases), intra-abdominal hypertension (2 cases), dyspareunia (1 case), urinary tract infection (2 cases) and vaginal granuloma (1 case) | Bile leakage (2) and bowel serosal laceration (1 case) | Intraoperative laparoscopic treatment, re-operation and conservative treatment |
| Pugliese et al.54 | 0 | Bile leakage (1 case) | Nasobiliary drainage |
| Kilian et al.59 | 0 | Bilioma as a result of aberrant bile duct (1 case) | Re-operation |
| Cuadrado-Garcia et al.56 | Mild hematuria (1 case) and urinary tract infection (1 case) | 0 | Conservative treatment |
| Hensel et al.58 | 0 | Urinary bladder injury (1 case) and delayed vaginal wound bleeding (1 case) | Intraoperative laparoscopic repair and postoperative suturing |
| Zornig et al.35 | 0 | Douglas pouch abscess (1 case) | Re-operation |
Transrectal NOTES
Clinical experience in transrectal NOTES
Compared with transgastric and transvaginal NOTES, transrectal NOTES (TR-NOTES) is the least investigated in both animal and clinical trials as there is a risk of fecal contamination (Fig. 1). However, transrectal access allows perfect orientation to supracolic organs. In addition, the transanal endoscopic operation (TEO) platform device was available for transanal endoscopic microsurgery (TEM).73 TEO was originally designed for dissection of lower rectal cancers below the peritoneal reflection with conventional laparoscopic instruments. Recent cadaveric studies and individual clinical cases demonstrated the feasibility of using the TEO device to carry out transanal rectosigmoidectomy.73-76 Whiteford et al.73 carried out three cases of TR-NOTES sigmoidectomy in cadavers. The study established critical steps in TR-NOTES sigmoidectomy using the TEO device, including transanal mobilization of sigmoid, en-bloc lymphadenectomy, primary colorectal anastomosis and specimen retrieval. In 2010, the first clinical case of laparoscopy-assisted TR-NOTES total mesorectal excision for early rectal cancer was reported.74 The whole procedure took 4.5 h and postoperative recovery was uneventful. Tuech et al. reported another case of TR-NOTES for rectal cancer located 3 cm above the dentate line using a novel Endorec trocar (Aspide Médical, La Talaudière, France).76 The procedure took 5 h and the length of specimen was 20 cm. The patient recovered uneventfully. Other TR-NOTES procedures such as umbilical hernia repair77 and appendectomy78 have been explored in cadaver models.
Clinical NOTES-related procedures
NOTES-related procedures are complex endoluminal procedures that evolved from the concept of NOTES. In Asia, clinical NOTES procedures can be subclassified into Pure/Hybrid NOTES and NOTES-related procedures. As a result of cultural variances and differences in disease prevalence, the acceptance of transvaginal NOTES procedures is much lower in Asian countries. The high prevalence of upper gastrointestinal diseases has led to a significant development of NOTES-related procedures. Inoue et al. first carried out peroral endoscopic myotomy (POEM) in 17 patients with achalasia.79 All the steps of POEM were achieved using ordinary endoscopic instruments, which included a mucosal entrance and development of a long submucosal tunnel, endoscopic myotomy, as well as closure of the entrance using clips. Currently, more than 250 cases of POEM have been carried out in Japan. POEM was quickly adopted from other Asian countries.80, 81 Because of the high prevalence of upper gastrointestinal cancers, another established NOTES-related procedure is endoscopic full-thickness resection (EFTR). Cho et al. reported carrying out EFTR and laparoscopic lymph node dissection in 14 patients.82 These patients were contraindicated for treatment by endoscopic submucosal dissection (ESD) alone as the majority were submucosal carcinomas. EFTR were successfully carried out with clear resection margins, and the defect was closed by laparoscopic suturing. This approach avoided gastrectomy and improved postoperative recovery. Zhou et al. carried out EFTR for treatment of gastric submucosal tumors without laparoscopic assistance in 26 patients.83 All the tumors were completely resected, and the mean size of tumors was 2.8 cm. The remnant gastric wall defect was closed by ordinary endoclips. However, EFTR has a risk of peritoneal dissemination and seeding of the tumor. Inoue et al. reported the technique of CLEAN-NET where the serosa and muscle layer are selectively dissected with a laparoscopic approach and the gastric mucosa is preserved as a barrier.84 The techniques of non-exposure dissection were developed to prevent peritoneal dissemination during full-thickness resection.85 EFTR cannot address potential regional lymph node dissemination when treating gastric submucosal adenocarcinoma. Abe et al. combined laparoscopic lymph node resection with laparoscopic and EFTR of submucosal gastric cancers.86 These techniques served as potential treatments for submucosal gastric adenocarcinoma with adequate oncological clearance while preserving the stomach, which will improve patients' quality of life.
Technological and devices developments for NOTES
Closure of gastrointestinal access
Over 20 devices27 have been tested for closure of gastrointestinal access. Yet, the standard method and device for closure has not been defined. A few trials used endoscopic clips or T-tags for closure of gastrotomy.3, 5, 8, 9 Endoclips were not considered secure as indicated by low bursting pressure after closure in ex vivo studies (<20 mmHg).87, 88 An ideal closure device should safely pass into the gastrointestinal tract and achieve full-thickness closure. Potential devices that can achieve full-thickness gastrointestinal closure include Eagle Claw (Olympus R&D, Tokyo, Japan) and Over-the-scope clip (Ovesco Endoscopy, Tübingen, Germany). Chiu et al. reported closure of gastrotomy using Eagle Claw VII in 10 porcine models after transgastric tubal ligation. All the gastrotomies were successfully closed, and postmortem examinations showed no evidence of leakage.17
Research on peritoneal infection after NOTES
One of the important risks for NOTES is the introduction of bacteria through the gastrointestinal access. Narula et al.89 assessed peritoneal bacterial load and contamination in 50 patients undergoing gastrotomy as a part of laparoscopic Roux-en-Y procedure. Samples from gastric and peritoneal aspirates before and after gastrotomy were sent for bacterial culture. Results indicated that transgastric manipulation could contaminate the abdominal cavity but the contamination did not result in peritonitis or abscess. Similar results were obtained from 10 transgastric peritoneoscopies without gastric decontamination.21 Despite minimal peritoneal contamination upon transgastric NOTES, most authors prefer a preventive protocol including prophylactic antibiotics, gastric irrigation with antibiotics solution, and disinfection of the endoscope and instruments.7, 24, 90, 91
Spatial orientation and multi-tasking platform
Unlike laparoscopic surgery, access for NOTES may not be in coaxial alignment to the pathology. Compared to transvaginal NOTES, upside-down images and disorientation during TG-NOTES to the supracolic compartment remains a genuine challenge. Disorientation in the operative field would not only result in difficulty of manipulation but also in a higher risk of complications.92 Three-dimensional (3D) images might enhance the appreciation of depth for more accurate navigation during NOTES. This could be a feature integrated into the design of a novel multi-tasking platform.93-95 Holler et al. designed an innovative Multisensor-Time-of-Flight (MUSTOF) endoscope with a real-time 3D surface model integrated into the imaging system.96
Numerous ingenious designs of multi-tasking platforms, including EndoSAMURAI (Olympus Medical Systems, Co., Tokyo, Japan) and the TransPort™ Multi-lumen Operating Platform (USGI Medical, San Clemente, CA, USA)97, 98 were able to provide two manipulating arms for dissection and suturing. Sun et al. reported the development of an endoscopic robotic system: Master And Slave Transluminal Endoscopic Robot (MASTER).94, 99 Recently, a multicenter clinical trial was conducted on the use of MASTER to carry out gastric ESD in five patients.100 This clinical study showed that the MASTER robotic endoscope greatly enhanced the performance of ESD and shortened the operative time.
From clinical evidence, it appears that cholecystectomy and appendectomy are easier to establish through the transvaginal approach. Perhaps a single-incision laparoscopic surgery (SILS) port can be modified for TV-NOTES, as SILS ports have achieved adequate sealing to maintain peritoneal insufflation and accommodate multiple ports for instrumentation.101, 102
Conclusions
Clinical trials on NOTES have been increasingly conducted in the past 5 years. Transvaginal cholecystectomy is the commonest reported NOTES procedure, while POEM is increasingly carried out worldwide as an important NOTES-related procedure. Despite few reports on transrectal NOTES, it has significant potential, as preliminary data support its feasibility and safety in carrying out transanal colorectal resection. Although there are a large number of NOTES and NOTES-related clinical procedures confirming the feasibility and safety of such an approach, the performance of pure NOTES necessitates major technological advancements as well as good clinical indications. At present, pure NOTES using conventional endoscopic instruments cannot simulate surgical resection done by laparoscopic instruments, and a hybrid endolaparoscopic approach is a logical step forward. The future development of NOTES will depend on innovation and technological development in endoscopic instruments and multi-tasking platforms.
Conflict of Interests
Authors declare no conflict of interests for this article.