Ventilation/perfusion SPECT in children: Feasibility, impact on clinical decision-making and interrater agreement
Ronan M. G. Berg and Jann Mortensen contributed equally to this study and share last authorship.
Abstract
Introduction
It remains to be established whether it provides any clinical or diagnostic benefits to perform ventilation/perfusion (V/Q) scintigraphy as a single photon emission computed tomography in children. Here, we report our experience with this modality, evaluate its impact on clinical decision-making and assess its interrater agreement.
Methods
All V/Q scintigraphies performed in children over a 1-year period were identified, and patient files were reviewed. Two nuclear medicine physicians, blinded to patient data and each other's readings, interpreted all scintigraphies.
Results
A total of 20 planar and SPECT V/Q scintigraphies were identified. In 17/20 cases (85%), the results of the scan were found to directly inform clinical decision-making. SPECT mainly ruled out the presence of ventilation and perfusion defects that were suspected on planar scintigraphy. In terms of interrater agreement, Cohen's ϰ coefficients for planar ventilation and perfusion scintigraphy were 0.34 and 0.38 (fair agreement), respectively, while the corresponding values for SPECT were 0.42 and 0.61 (moderate to substantial agreement).
Conclusion
It is both feasible and clinically meaningful to perform V/Q SPECT in children. In this patient group, V/Q SPECT furthermore seems to have better interrater agreement than planar scintigraphy.
1 INTRODUCTION
It is well established that performing ventilation-perfusion (V/Q) scintigraphy as a single photon emission tomography (SPECT) is superior to conventional planar scintigraphy for diagnosing both pulmonary embolism and several non-embolic pulmonary disorders in adults (Gutte et al., 2010; Mortensen and Berg, 2019), but studies on the clinical value of paediatric V/Q-SPECT are scarce (Sanchez-Crespo, 2019). Hence, no existing guidelines on V/Q scintigraphy recommend SPECT in children (Bajc et al., 2019; Ciofetta et al., 2007). Most studies performed in children have been performed without SPECT and SPECT/CT, but have early on been the fundament for performing lung scintigraphies in children (Gordon and Helms, 1982; Gordon et al., 1981).
In the present study, we report on the experience of conducting V/Q scintigraphy as a SPECT supplemented with a low-dose CT (ldCT) of the chest as an add-on to the V/Q planar scintigraphy in children referred to our department for various indications. We compared the results of V/Q SPECT-ldCT with those of a concomitantly obtained conventional V/Q planar scintigraphy, both in terms of findings, impact on clinical decision-making and interrater agreement.
2 MATERIALS AND METHODS
2.1 Design
We retrospectively identified all paediatric patients (age 0−18 years) that were referred to the Department of Clinical Physiology and Nuclear Medicine, Rigshospitalet for a V/Q scintigraphy over a 1-year period in 2013.
2.2 Institutional approval
At the time of this study, no institutional approval was required for retrospective studies according to Danish legislation.
2.3 Scan protocols and reconstruction methods
Approximately 82.7 (range, 22−166) MBq 99mTc macro-aggregated albumin (MAA) was injected intravenously, using the EANM calculator (European Association of Nuclear Medicine, 2019) (effective dose from 82.7 MBq [99mTc]Tc-MAA is 2.8 mSv for a 5-year-old), while concurrently inhaling 81mKr gas for 15 min from a 450 (range, 300−600) MBq 81Rb/81mKr generator during both planar and SPECT imaging as both examinations were part of the routine clinical protocol. In steady state with the used air flow rate of 1−2 L/min, there is 63 MBq in the lungs (Camps et al., 1988). This is dosimetrically equivalent to a single administration of 3 GBq 81mKr without exhalation yielding an effective dose of 0.26 mSv for a 5-year-old (Bajc et al., 2019). Anterior, posterior and oblique projections (three camera positions) were recorded on a two-headed Precedence gamma camera (Philips) with low-energy general-purpose (LEGP) parallel-hole collimators (de Nijs et al., 2021) and a 256 × 256 matrix. V/Q SPECT and ldCT were performed in the same session using the same scanner, which included an MDCT scanner (16-slice Brilliance). The use of LEGP collimators causes a small signal from septal penetration of the 190 keV photons from 81mKr (de Nijs et al., 2021). Since the maximal septal penetration is ~15% (~2% for 99mTc), this is expected to only have a small influence on the spatial resolution of the ventilation images. 81mKr was also administered during the SPECT acquisition. After 81mKr inhalation was started (again) the SPECT-acquisition was first started after it was ensured that the live ventilation image on the scanner showed a stable ventilation image. The SPECT projections were acquired in a 64 × 64 matrix with 9.3 mm isotropic pixel size. Energy windows with 20% full width were set at 140.5 keV for 99mTc and 190.5 keV for 81mKr.
The CT protocol consisted of one acquisition with the patients scanned in supine position and as a ldCT scan (140 kV, 20 mAs/slice, 16 × 1.5 collimator, 0.5 s rotation time and pitch of 0.813) that was used for attenuation correction of V/Q SPECT data and obtained during tidal breathing. Reconstructed CT images had a 512 × 512 matrix size with an isotropic pixel size of 1.17 mm and a 5 mm slice thickness.
2.4 Special considerations for patient cooperation
With the parents in the room actively participating under instructions, the child was placed in supine position and a simultaneously performed double isotope ventilation-perfusion-study with 81mKr and [99mTc]Tc-MAA. The planar perfusion-ventilation study is performed with six projections (three camera positions) with collection of 1 000 000 and 500 000 counts in anterior and posterior planes on the perfusion and ventilation images, respectively. In oblique positions (LAO/RPO and RAO/LPO), 600 000 and 300 000 counts sufficient in the perfusion and ventilation images, respectively.
After 81mKr inhalation was started (again) the SPECT-acquisition was first started after it was ensured that the live image on the scanner showed a stable ventilation image. The SPECT acquisition consisted of 64 projections (32 for each head), 12 s per projection using the same MAA-dose and collimators. The SPECT acquisition was reconstructed iteratively with the Astonish algorithm (4 iterations and 16 subsets), which included scatter correction with a scatter kernel, resolution recovery and CT-based attenuation correction. The reconstructed voxel size corresponded to the pixel size of the acquisition.
In the younger child, the feed and rest procedure is followed by the ‘Cortsen-procedure’ (ad modum Cortsen); at the sleeping well-positioned child the catheter for 81mKr inhalation is placed in one nostril, using a finger or cotton buds for closing the other nostril and with a pacifier in the mouth—as shown at Figure 1a,b. The same inhalation method is also used for children with the need for sedatives or general anaesthesia. If the child has a stuffy nostril a nasal oxygen catheter can also be used.
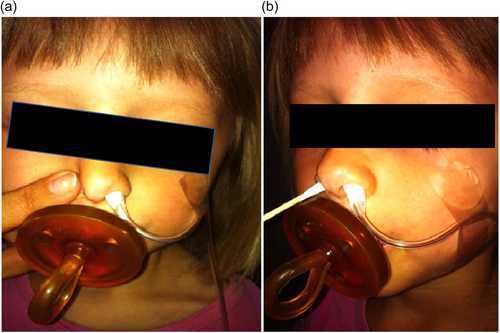
In older children and if the child is able to cooperate the nose clip is placed over the nose and the mouthpiece is placed in the mouth for inhalation, as in adults Figure 2.

2.5 Medical file review
Referral diagnosis, indications for the ventilation-perfusion scintigraphy and the impact on clinical decision-making were verified and extracted from the patients' medical files by two of the authors (L. B., M. L. M.).
2.6 VQ scintigraphy readings
All VQ scintigraphies were consensus read by a junior and senior nuclear medicine physician (M. L. M. and J. M./L. B., respectively) who reported ventilation and perfusion defects on each planar V/Q scintigraphy and SPECT-ldCT. They furthermore reported to which extent the ldCT aided in the interpretation of the V/Q SPECT. The images are read with both AC and non-AC corrected scans when a defect was identified. This reading was the basis for clinical decision-making.
For the assessment of interrater agreement of planar V/Q scintigraphy versus SPECT-ldCT, two experienced senior nuclear medicine physicians, specialized in nuclear pulmonology (J. M.) and in paediatric nuclear medicine (L. B.), respectively reread all V/Q scintigraphies, blinded to patient data, outcomes and each other's readings. Furthermore, they did not have access to the planar scintigraphies and the SPECT-ldCT from the same case at the same time. They rated each lobe for the presence or absence of a defect on both ventilation and perfusion scintigraphies.
2.7 Statistics
Continuous data are presented as median (IQR), while categorical data are presented in %. Cohen's ϰ coefficient (with 95% CI) was calculated on the basis of defects in each lobe, considering values of 0 as no agreement, above 0 but ≤0.20 as slight, 0.21−0.41 as fair, 0.41−0.60 as moderate, 0.61−0.80 as substantial and 0.81−1.00 excellent agreement (Landis and Koch, 1977). The analyses were performed using SAS statistical software version 9.2 (SAS Institute Inc.).
3 RESULTS
3.1 Patient characteristics
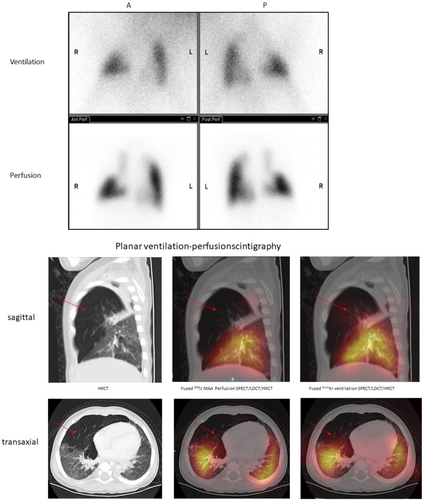
A total of 20 consecutive V/Q scintigraphies were performed in 19 children during the study period, and apart from one planar ventilations scintigraphy that failed, all planar and SPECT-ldCT scans were successfully completed without any need for sedatives. A representative planar V/Q scintigraphy with the corresponding SPECT-ldCT is provided in Figure 3. Seven (37%) of the children were female and 12 (63%) were male. The median age at the time of the scan was 4 years and 5 months (IQR 2 years and 3 months to 13 years and 4 months). Eight children were referred to investigate whether pulmonary stenosis was present after surgical intervention (cases 1−8), four of whom had tetralogy of Fallot (cases 3 and 6−8). Three were referred due to congenital lobar emphysema (cases 9, 11 and 12), one of whom had the scan repeated after surgery, four due to suspected pulmonary embolism (cases 16−19) and four due to other conditions (Table 1).
| Case no | Age (years) | Sex | Indication |
|---|---|---|---|
| 1 | 1.5 | Female | Suspected pulmonary artery stenosis after surgically corrected pulmonary artery sling |
| 2 | 9.3 | Male | Suspected pulmonary artery stenosis after surgically corrected situs inversus |
| 3 | 3.1 | Male | Suspected pulmonary artery stenosis after surgically corrected tetralogy of Fallot with pulmonary atresia |
| 4 | 8.3 | Male | Suspected pulmonary artery stenosis after surgically corrected d-transposition of the great arteries with coarctation of the aorta and ventricular septal defect |
| 5 | 3.9 | Male | Suspected pulmonary artery stenosis after surgical closure of patent ductus arteriosus |
| 6 | 3.4 | Male | Suspected pulmonary artery stenosis after surgically tetralogy of Fallot with pulmonary atresia and major aortopulmonary collateral artery |
| 7 | 13.0 | Male | Suspected pulmonary artery stenosis after surgically corrected tetralogy of Fallot with pulmonary atresia and coarctation of the aorta |
| 8 | 6.0 | Female | Suspected pulmonary artery stenosis after surgically corrected tetralogy of Fallot with ventricular septal defect |
| 9 | 1.1 | Male | Regional lung function before surgery for congenital lobar emphysema |
| 10 | 14.7 | Male | Acquired emphysema after respiratory distress syndrome as a neonate |
| 11a | 0.3 | Female | Regional lung function before surgery for congenital lobar emphysema |
| 11b | 1.1 | Female | Regional lung function before surgery for congenital lobar emphysema |
| 12 | 0.2 | Male | Regional lung function before surgery for congenital lobar emphysema |
| 13 | 2.5 | Male | Congenital pulmonary airway malformation |
| 14 | 3.9 | Male | Regional lung function before surgery due to chronic Pseudomonas aeruginosa infection |
| 15 | 5.0 | Female | Functional distribution before surgery due to cystic fibrosis |
| 16 | 16.4 | Female | Follow-up for previous pulmonary embolism (Factor V Leiden mutation and gestagen-containing contraceptive pills) |
| 17 | 17.5 | Male | Suspected pulmonary embolism following trauma with lung contusion |
| 18 | 14.1 | Male | Suspected pulmonary embolism following thrombotic thrombocytopenic purpura |
| 19 | 16.4 | Male | Suspected pulmonary embolism because chronic pulmonary hypertension |
3.2 Reading and interpretation
Ventilation and perfusion defects as identified on planar scintigraphy and SPECT are reported in Table 2. Ventilation defects were noted on 15 of the 20 (75%) planar ventilation scintigraphies and on 16 of the 19 (84%) SPECT scans. Ventilation defects were noted in a median of 3 (IQR 2−4) lobes on planar scans and 3 (IQR 1−4) lobes on SPECT. SPECT did not lead to changes in the interpretation of 5 (26%) of the planar ventilation scintigraphies, while SPECT ruled out suspected ventilation defects in 9 (47%) of the planar ventilation scintigraphies and revealed new defects in 5 (26%) cases. Perfusion defects were noted on 17 of the 20 (85%) planar perfusion scintigraphies and on 19 of the 20 (95%) SPECT scans. Perfusion defects were noted in a median of 4 (IQR 2−4) lobes on planar scans and 3 (IQR 2−4) lobes on SPECT. SPECT did not lead to any changes in the interpretation of 8 (40%) of the planar perfusion scintigraphies, while SPECT ruled out suspected perfusion defects in another 8 (40%) of the planar perfusion scintigraphies and revealed new perfusion defects in 4 (20%) cases.
| Ventilation | Perfusion | |||
|---|---|---|---|---|
| Case no | Planar | SPECT | Planar | SPECT |
| 1 | 2 | 2 | 2 | 2 |
| 2 | 4 | 1 | 3 | 3 |
| 3 | 3 | 0 | 4 | 4 |
| 4 | 0 | 0 | 0 | 0 |
| 5 | 3 | 4 | 3 | 3 |
| 6 | 5 | 4 | 5 | 4 |
| 7 | 2 | 1 | 5 | 3 |
| 8 | 2 | 3 | 2 | 2 |
| 9 | 4 | 4 | 4 | 4 |
| 10 | 4 | 5 | 4 | 5 |
| 11a | 5 | 3 | 4 | 3 |
| 11b | 4 | 3 | 5 | 3 |
| 12 | 3 | 1 | 3 | 1 |
| 13 | 4 | 2 | 4 | 2 |
| 14 | 5 | 4 | 5 | 4 |
| 15 | 4 | N/A | 5 | 5 |
| 16 | 0 | 0 | 3 | 1 |
| 17 | 0 | 1 | 0 | 1 |
| 18 | 4 | 5 | 1 | 4 |
| 19 | 0 | 0 | 0 | 5 |
- Abbreviation: SPECT, single photon emission tomography.
In 17 cases (85%), at least one of the readers found that ldCT specifically aided in the interpretation of V/Q SPECT, either in identifying the cause of a scintigraphic defect, such as regional hyperinflation, an infiltrate, atelectasis or pleural effusion (9 cases, 45%) or to exclude false positive defects due to interlobar fissures or for a better delineation of lobes or segments (8 cases, 40%).
3.3 Impact on clinical decision-making
V/Q scintigraphy was found to influence clinical decision-making in 17 (85%) cases, of which this was specifically based on the results of V/Q SPECT-ldCT in 10 (50% of total). Of the 8 children referred due to pulmonary stenosis, 2 (cases 2 and 6) were found to have an abnormal functional distribution between the right and left lung, and on this basis, surgical balloon dilatation was performed. Five others were found to have equal functional distribution between the right and left lung, and balloon dilatation was therefore not pursued. In all these cases, a similar conclusion was reached based on planar scintigraphy and V/Q SPECT-ldCT. In one child (case 7), the V/Q scintigraphy was performed as a baseline scan for potential use in future evaluations and it therefore did not have any direct clinical impact.
Four V/Q scintigraphies were performed in 3 children with congenital lobar emphysema; in three children, it was performed to evaluate the need for surgery as well as for surgical guidance. On this basis, a decision was made to perform surgery in two cases (cases 9 and 12) and not to do it in one case (case 11), please see Figure 3 (case 9). In all these cases, SPECT-ldCT specifically identified the location and extent of the emphysematous lesions.
In the four children referred due to suspected pulmonary embolism, the diagnosis was verified in one case (case 16) and ruled out in three (cases 17−19). Pre-emptive anticoagulation therapy was therefore maintained in the former and discontinued in the latter three. In all cases, the final diagnosis was based on SPECT-ldCT and not on planar scintigraphy.
In two children (cases 14 and 15), the V/Q scintigraphy was performed to evaluate whether surgery with the removal of lung tissue was feasible, and both cases were consequently referred to surgery. SPECT-ldCT, but not planar scintigraphy, specifically identified the location and extent of the lesions. In one child (case 13), V/Q-scintigraphy was used as a supplement to several other imaging modalities for a comprehensive evaluation of airway and lung tissue function and structure, and did not affect clinical decision-making per se.
The Modum Cortsen procedure was well-tolerated by all children, and sedatives were only used in 5%, despite a median age of 4 years.
3.4 Interrater agreement
For identifying ventilation defects, planar scintigraphy provided an interrater agreement rate of 65%, while it was 67% for SPECT. The corresponding ϰ-values were 0.34 (95% CI: 0.17−0.51) and 0.42 (0.25−0.59). The interrater agreement rate for identifying perfusion defects on planar scintigraphy was 68%, while it was 80% for SPECT, with resultant ϰ-values of 0.38 (95% CI: 0.19−0.56) and 0.61 (95% CI: 0.46−0.76), respectively.
4 DISCUSSION
In the present study we found that V/Q SPECT-ldCT in children; (1) both ruled out suspected defects and unveiled new defects in several cases when compared to planar V/Q scintigraphy, (2) was critical to clinical decision-making in most cases, and (3) yielded a moderate to substantial interrater agreement, while planar V/Q scintigraphy yielded only fair interrater agreement.
According to our findings, V/Q SPECT-ldCT was entirely feasible in children, as it was completed and of diagnostic quality in all children studied. Concerns have previously been raised that a V/Q SPECT may take too long for it to be feasible in children, at least if sedatives are to be avoided. A V/Q SPECT-ldCT takes longer (15 min) than a conventional planar V/Q scintigraphy (2−5 min), and since we conducted the planar scintigraphy and the SPECT-ldCT in succession, the total protocol took up to 20 min everything included. Despite that, the procedure was well-tolerated by all children, and sedatives were only used in 5%, despite a median age of 4 years. This likely reflects that we have a dedicated nuclear paediatric team of medical technologists and physicians at our department, who nurture both the child and their parents throughout the scan, and furthermore that the 81mKr breathing technique ‘ad modum Cortsen’ is well-tolerated.
This study highlights an important limitation in the interpretation of planar imaging compared to SPECT-ldCT. While we report a substantial proportion of ventilation and perfusion defects seen on planar imaging that were not confirmed on SPECT-ldCT, this phenomenon warrants further explanation. Planar scintigraphy can detect defects that, upon further assessment with SPECT and ldCT, may be attributable to anatomical changes such as atelectasis or other parenchymal alterations. For example, atelectasis may result in reduced or absent perfusion due to reflex vasoconstriction in response to diminished alveolar oxygen tension, leading to redirected blood flow. Similarly, reduced or absent ventilation in collapsed lung regions may appear as diminished tracer uptake. SPECT-ldCT, particularly with its integration of ldCT, provides additional anatomical context that can clarify the cause of these defects and alter their interpretation. However, SPECT-ldCT imaging also has limitations, including the potential amplification of noise due to shorter acquisition times per projection compared to planar imaging and the use of smoothing filters during reconstruction, which may obscure regions with low or absent tracer uptake. These factors highlight the need for careful consideration when interpreting findings and underscore the complementary roles of planar imaging and SPECT-ldCT in pulmonary V/Q scintigraphy.
The impact of V/Q SPECT-ldCT on clinical decision-making varied depending on the referral diagnosis. V/Q SPECT-ldCT has previously been highlighted as having the potential of being notably useful in the context of tetralogy of Fallot with pulmonary stenosis (Sanchez-Crespo, 2019). However, we did not find this to be the case, since the main clinical question is this context was the right-left functional distribution, which is validly estimated by planar scintigraphy alone. In contrast, and in accordance with previous studies (Thacker et al. 2015; Bajc et al., 2019; Sanchez-Crespo, 2019), we found that the advantages of the 3D visualization of ventilation and perfusion had a notable impact on clinical decision-making in cases where a regional assessment of lung function distribution on the lobar or segmental level is warranted. Other studies have also proposed V/Q SPECT as potentially useful for assessing postsurgical functional distribution in neonates with congenital diaphragmatic hernia (Sánchez-Crespo et al., 2008; Sanchez-Crespo, 2019), but no children were referred with this indication in the present study period.
The seemingly superior interrater agreement of V/Q SPECT when compared to planar scintigraphy supports its clinical use in children, but these findings must be interpreted with caution, due to potential recall bias. Although the senior nuclear medicine physicians reviewed the planar and SPECT images for the same case at separate times, it is possible that some cases were remembered, which could have influenced the comparison. Additionally, the methodology used to assess interrater agreement may not fully mitigate this bias. A potentially more robust approach would have been to use two independent groups of nuclear medicine physicians with similar experience, each assessing only one imaging modality.
Even though the readings of the scans in this study (2021) are performed 8 years after the clinical reading of the V/Q scintigraphies and the SPECT-ldCT (2013), the same scan can possibly, in certain cases, have been read by the same physician and therefore the risk of recall bias exist, though it must be very low due to the long period in between the readings.
Compared to conventional V/Q planar scintigraphy, SPECT-ldCT does expose the child to the additional radiation from the ldCT, which is approximately 0.5 mSv, but the more accurate and reliable assessment of the distribution of ventilation and perfusion with notable impact on clinical decision-making documented here, does, in our opinion, justify this. The largest radiation dose (effective dose for 5-year-olds) is caused by the single injection of [99mTc]Tc-MAA (no additional radiation dose), which according to the ICRP128 publication is approximately 2.8 mSv for 82.7 MBq. Radiation dose from 81mKr in this study with both SPECT and planar imaging is typically 0.26 mSv.
In conclusion, V/Q SPECT-ldCT is both feasible and clinically meaningful for several indications in children and according to our findings it provides both more accurate and reliable results than conventional planar V/Q scintigraphy.
AUTHOR CONTRIBUTIONS
Lise Borgwardt and Mette Louise Mørk coordinated the study and acquired the data. Ronan M. G. Berg analysed and interpreted the data and drafted the manuscript. Jann Mortensen acquired and interpreted the data. Lise Borgwardt conceived and designed the research, acquired and interpreted the data. Robin de Nijs verified scanning parameters and performed activity and radiation dose calculations. All authors made critical revisions and read and approved the final manuscript.
ACKNOWLEDGEMENTS
We would like to acknowledge technologist Annette Cortsen who developed the procedure—‘ad modum Cortsen’—for performing lung scintigraphies with SPECT-ldCT in children without sedatives. During this work, Dr. R. M. G. Berg was supported by a post.doc. grant from Copenhagen University Hospital—Rigshospitalet. The Centre for Physical Activity Research (CFAS) is supported by TrygFonden (grants ID 101390, ID 20045, ID 125132 and ID 177225). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




