The colon does not reach! A technical note with tricks to avoid colorectal anastomoses under tension
Abstract
Aim
We describe two options for colorectal anastomosis suitable in cases when the colon would reach the pelvis under tension.
Method
Deloyers procedure and the retro-ileal colorectal anastomosis are presented, focusing on practical tips and tricks to perform them. Insights on patients who underwent the procedures are provided to demonstrate the advantages and feasibility of the techniques.
Results
Each step of both techniques is detailed. Ten patients underwent Deloyers procedure and nine underwent retro-ileal anastomosis at our unit. A minimally invasive approach was attempted in 13 patients, of whom five required conversion to open surgery due to the technical complexity of the abdominal procedure. Colorectal anastomosis was successfully performed in all patients. There were no major intra-operative complications, although five patients had postoperative complications requiring further treatment.
Conclusions
Both techniques are effective in patients at risk of receiving a colorectal anastomosis under tension, and a minimally invasive approach can be used. However, owing to the complexity of surgery in this group of patients, the perioperative morbidity is not negligible. Careful postoperative management is advisable, and patients should be informed of the risks. In expert hands, the outcomes are acceptable, avoiding an ileorectal anastomosis and its constraints.
INTRODUCTION
Reconstruction of bowel continuity after extended left colectomy or repeated colon resections can be challenging, as the colon stump may not reach the rectum with an adjusted tension.
The main indications for this setting are metachronous colorectal cancer, synchronous left colon cancer, intra-operative left colon ischaemia, and Hartmann's reversal after extended colon resection. At times, the only alternative is complete or total colectomy and ileorectal anastomosis, although it has been associated with variable rates of morbidity, bowel dysfunction and impaired quality of life [1, 2].
We herein present our case series of challenging colorectal surgeries with useful restoration techniques to preserve the ileocaecal valve, thereby conferring better functional outcomes compared with ileorectal anastomosis.
MATERIALS AND METHODS
A case series of patients who underwent a Deloyers procedure (n = 10) or a retro-ileal anastomosis (n = 9) in a single centre is presented. Patient data, operative notes and postoperative follow-up were reviewed prospectively between February 2019 and February 2023.
Technical features
Extended left colectomy involves resection of at least the splenic flexure and the descending and sigmoid colon. Patients were placed in a modified Lloyd-Davies position. Four trocars were placed according to the body habitus: the camera port was inserted in the midline above the umbilicus, two 5-mm trocars were inserted 4–5 cm to the left and right of the midline equidistant from the camera port, and a 12-mm trocar was placed suprapubic in the midline. The patient was placed in the Trendelenburg position with a right-side tilt. Left-side colorectal resection was completed through a medial-to-lateral approach, proceeding with ligation of the inferior mesenteric artery and vein and mobilization of the descending colon and the splenic flexure. The greater omentum was detached from the transverse colon and the mesocolon was resected from left to right until the middle colic pedicle was identified. Attending to the particularities of each case, we ligated the middle colic vessels root or just the left branch depending on the margins and the suitability of the proximal transverse colon left, which defines the restorative technique. Afterwards, the patient position was shifted to a left-side tilt, and the small bowel and left colon were displaced towards the upper abdomen.
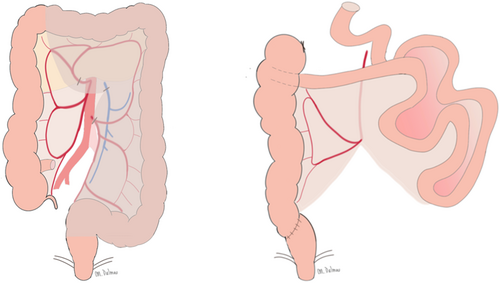
Deloyers technique
A Deloyers procedure was performed when the middle colic pedicle was ligated, and the transverse colon was discarded. The right colon was mobilized, and the hepatic flexure was taken down. The colectomy was completed at the level of the ascending colon through a Pfannenstiel incision, and a 29- or 31-mm anvil of a circular (EEA) stapler was placed. After re-establishing the pneumoperitoneum, an intracorporeal counterclockwise rotation of the right colon along the axis of the ileocolic vessels and a colorectal end-to-end stapled anastomosis were performed. In all cases, an appendectomy was performed before right colon mobilization to avoid the risk of acute appendicitis in an upper right quadrant position (Figure 1). Video S1 gives a demonstration, as previously reported [3].
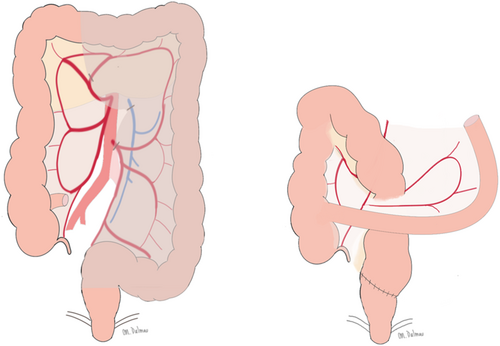
Retro-ileal pull-through technique
When the right branch of the middle colic pedicle and the proximal transverse colon could be preserved, the remnant colon usually reached the pelvis with excess tension. In those cases, a retro-ileal anastomosis was performed. The colectomy was completed at the level of the mid-transverse colon through a middle-right para-umbilical incision and a 29- or 31-mm anvil of a circular (EEA) stapler was placed. After re-establishing the pneumoperitoneum, the ileocolic mesentery root was exposed, creating a passage of 3–4 cm in the avascular plane under the ileocolic artery and between two ileal branches. The proximal transverse colon passed through to reach the rectum, and a colorectal end-to-end stapled anastomosis was performed. Finally, the defect between the mesocolon and ileal mesentery was closed to avoid an internal hernia (Figure 2).
Video S1 gives a step-by-step demonstration.
RESULTS
Colon cancer was the main indication that led to a left extended colectomy in 11 cases: four cases of metachronous left colon cancer after a previous colon resection, four cases of synchronous colon cancer (transverse and sigmoid), and four primary left colon cancer near splenic flexure ( two cases of left colon cancer and two cases of transverse colon cancer).
Moreover, a restoration technique was needed in five cases after Hartmann reversal, two cases of extended diverticular disease and one case of a rectovaginal fistula. In this series, there were no cases of left colectomy with intra-operative colonic hypoperfusion leading to an extended left colectomy. The patient characteristics are reported in Table 1.
| Variables | N (%) |
|---|---|
| Agea | 67.32 ± 12.2 |
| Sex (male) | 13 (68.4%) |
| BMIb (kg/m2) | 26.4 ± 4.3 |
| ASA grade | |
| ASA I | 1 (5.3%) |
| ASA 2 | 11 (57.9%) |
| ASA 3 | 7 (36.8%) |
| No. comorbidityb | |
| 0–1 | 12 (63.2%) |
| 2–4 | 6 (32.6%) |
- Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index.
- a Average (standard deviation).
- b Comorbidity: cardiovascular disease, neurological, chronic obstructive pulmonary disease, thromboembolic disease, cirrhosis and chronic kidney disease.
Among the 13 patients who underwent a laparoscopic approach, intracorporeal circular stapler anastomosis was feasible in eight cases, whereas the remainder were converted into an open approach due to technical complexity, mainly in the resection part. An open approach was observed in six cases, and none of the patients was diverted with a loop ileostomy. There were no significant intra-operative complications such as ischaemia of the remaining colon, failure to perform the anastomosis or significant blood loss.
Five patients developed postoperative complications requiring reintervention (Table 2). One 80-year-old patient with retro-ileal anastomosis had rectal bleeding leading to a haematoma and anastomotic leakage (AL), requiring reoperation with endoscopic drainage placement (endosponge) to heal the defect and final closure in a second intervention by the transanal minimally invasive surgery approach. Two patients had an AL: a 58-year-old patient with a Deloyers procedure who was reoperated with anastomotic reinforcement and diverted with a loop ileostomy, which was removed after 12 months, and an 82-year-old patient with retro-ileal anastomosis who developed abdominal sepsis and underwent a complete colectomy and terminal ileostomy on the seventh postoperative day. During a prolonged intensive care unit stay, he remained in multiple organ failure for 3 weeks dependent on the ventilator and requiring tracheostomy, renal replacement therapy and cardiovascular support, and finally died. Furthermore, an 84-year-old patient presented with four synchronous colon tumours, one of them occlusive in the transverse colon requiring prosthesis placement, and liver metastasis. He underwent an elective left extended colectomy with Deloyers anastomosis and was discharged in the sixth postoperative day without issues. One month later he presented with occlusive symptoms and a CT scan showed anastomotic partial occlusion. He was reoperated showing anastomosis torsion with dehiscence and diffuse peritonitis, so a complete colectomy and terminal ileostomy was performed. The patient recovered uneventfully and was discharged on the seventh postoperative day. Finally, an 82-year-old man presented with synchronous transverse colon cancer and infected sigmoid cancer with bilobar liver metastasis and underwent a Deloyers procedure following a laparoscopic left extended colectomy. On the fifth postoperative day he was reoperated due to suspected abdominal sepsis. An exploratory laparoscopy demonstrated abundant sero-haemorrhagic ascites and ruled out ischaemia, perforation or AL. He experienced a rapid general decline, an abdominal and thoracic CT scan that showed intestinal pneumatosis 10 cm from the duodenojejunaljunction and he died 1 day later from multiorgan failure with intercurrent liver failure.
| Outcome | Deloyers (n = 10) | Retro-ileal (n = 9) | Total (n = 19) |
|---|---|---|---|
| Conversion | 0/5 (0%) | 5/8 (62.5%) | 5/13 (38.4%) |
| Complications | |||
| Small bowel obstruction | 4 (40%) | 4 (44.4%) | 8 (42.1%) |
| Anastomosis torsion | 1 (10%) | 0 (0%) | 1 (5.3%) |
| Anastomosis leak | 2 (20%) | 2 (22.2%) | 4 (21.1%) |
| Reintervention | 3 (30%) | 2 (22.2%) | 5 (26.3%) |
| CCIa | 25.7 ± 31.2 | 21.9 ± 34.2 | 23.9 ± 31.8 |
| Dischargea (days) | 11.6 ± 9.8 | 7.9 ± 7.6 | 9.8 ± 8.8 |
| Follow-upa (months) | 22.2 ± 9.8 | 31.0 ± 16.1 | 26.6 ± 16.1 |
| Mortality 90 days | 1 (10%) | 1 (11.1%) | 2 (10.5%) |
- Abbreviation: CCI, Charlson Comorbidity Index.
- a Average (standard deviation).
The overall complication burden of the cohort was Charlson Comorbidity Index 23.9 ± 31.8 with an average hospital stay of 9.8 ± 8.8 days. Patients were followed up for 26.6 ± 16.1 months on average without significant complications.
DISCUSSION
Reconstruction of bowel continuity becomes a challenge after an extended left colectomy, especially when performed after a previous colectomy. Ileorectal or ileoanal anastomosis or even a terminal colostomy are common approaches to tackle the situation, despite their inherent disadvantages in terms of bowel function and physical impact on the patient's life. These old techniques described above have been overlooked for decades, although they do represent alternatives to ileorectal anastomosis, since the ileocaecal valve and distal ileum loop are preserved, ensuring a functional colon transit [1].
In 1964, Deloyers [2] described the anastomosis between the right colon and the rectum, after complete mobilization and counterclockwise rotation of the right colon, allowing for a tension-free colorectal anastomosis [4]. Although it was first indicated in ulcerative colitis, megacolon and chronic constipation, lately it has been used for a wide range of indications and has proven to be a feasible solution for both open and laparoscopic extended left colon resection with inadequate residual length for standard colorectal anastomosis. Concurrently, the retro-ileal pull-through technique was first described by André Toupet in 1961 and later performed by Rombeau et al. [5] in 11 patients affected by extended diverticulitis, splenic colon cancer and severe radiation of the descending colon [5]. The technique consists of creating a passage in an avascular plane in the terminal ileum mesentery where the proximal transverse colon passes through to reach the rectum.
In the last decade, a rebound of case series using these techniques for a variety of indications has been observed, demonstrating them to be alternative solutions for both open and laparoscopic extended left colon resections with inadequate colon length for standard colorectal anastomosis.
Previous reports demonstrated the feasibility of Deloyers procedure as a low morbidity technique [6-8] with 3.4%–10% AL [9, 10] compared to conventional colorectal and ileorectal anastomosis (5%–13.2%) [11]. The main technical disadvantage is creating torsion of the vascular ileocolic pedicle, increasing the risk of ischaemia. This was reported in a single case of intra-operative ischaemia of the remaining colon, which required total colectomy with ileorectal anastomosis [10]. In order to diminish compression of the ileocolic pedicle, Kontovounisio et al. [8] proposed a modification adding a caecopexy and right colon fixation to the right paracolic gutter. Moreover, to avoid potential vascular torsion of the ileocolic pedicle, an antiperistaltic caecorectal anastomosis may become a potential alternative to treat selective patients after a left extended colectomy. Although it is widely described to treat colonic inertia, satisfactory perioperative functional outcomes have been noted in patients with colon cancer in terms of bowel movements and stool consistency [12].
Few series of retroileal anastomosis have been reported, all associated with low morbidity, and a single case of anastomotic leak (3%) described in a 28-case report by Nafe et al. [13]. Furthermore, Kent et al [14] described this technique as a feasible tension-free alternative for coloanal anastomosis. Although creation of a mesoileon window has a potential risk of stenosis or internal hernia, no complications related to the surgical procedure were encountered in the literature. To minimize the risk, Sileri et al [15]. proposed colon fixation to the border of the mesenteric passage and narrowing the residual gap to avoid internal hernias through the mesenteric window.
Regarding functional results, these techniques had satisfactory perioperative and long-term outcomes with a median of two bowel movements per day [1, 6, 8, 9, 16] favourably compared with five daily defaecations after ileorectal anastomosis [17].
This series includes a considerable number of cases performed by two relatively uncommon procedures. The Deloyers technique was used when the middle colic and right colic pedicle needed to be ligated, whereas the retro-ileal pull-through technique was performed when part of the transverse colon could be preserved. Both techniques were feasible with a laparoscopic approach, although a higher conversion rate was observed in the retro-ileal anastomosis group where four out of five patients had a background of a previous colectomy for synchronous cancer or other abdominal surgeries. The risk of conversion in colorectal surgery has been related to several perioperative factors, such as history of previous abdominal surgery, liver disease, obesity or metastatic cancer. Also, compared with right colectomy, the highest risk of conversion exists in a proctectomy procedure (OR 2.82; P = 0.01) followed by a transverse colectomy (OR 1.88; P = 0.01) [18]. The increased technical complexity is inherent to the extended left colectomy indication, which usually entails cases with prior colectomies.
Although the perioperative morbidity in this cohort is not negligible, note that patients who required a reoperation had an American Society of Anesthesiologists score over 3, were overweight (body mass index ≥25) and four out of five were aged over 80. All these risk factors have been associated with higher rates of complications and mortality [19] Careful postoperative management is advisable in this subset of high risk patients, who should be informed about the higher risks.
The main complication that led to reoperation in this series was AL. The occurrence of AL often has a multifactorial cause. Most of them can no longer be changed at the time of surgery. However, there are a few factors that can be influenced, such as compromised tissue perfusion at the anastomosis site. In this series, the air leak test and inspection of the resection doughnuts was addressed in all cases, whereas the use of indocyanine green fluorescence angiography to assess the anastomotic perfusion was only done in selected cases. Considering that the Deloyers and retro-ileal pull-through techniques are alternatives to prevent high tension anastomosis after an extended left colectomy, which is a rare procedure, routine use of indocyanine green fluorescence angiography is recommended to decrease AL rates [20].
The use of one technique over the other should be based on the length of transverse colon, patient body habitus and surgeon expertise in colorectal surgery, aiming to preserve as much colon as possible, assuring appropriate flow and a tension-free anastomosis. In expert hands, the laparoscopic approach is feasible; otherwise a higher risk of conversion could be expected. In general practice, if these techniques are not convenient, a total colectomy with ileosigmoid or ileorectal anastomosis is a good alternative.
CONCLUSION
These techniques are feasible and have acceptable functional outcomes and therefore should be considered by colorectal surgeons facing an extended left colectomy. However, due to the technical complexity of these patients, potential perioperative morbidity should be assessed and carefully balanced. Prospective studies are needed to compare technical and functional outcomes to total colectomy with ileorectal anastomosis.
AUTHOR CONTRIBUTIONS
MD has contributed to the conception and design, interpretation of data and drafting of the manuscript. GP and MMG have been involved in drafting the manuscript and have given final approval to the version published. EEB and MA have revised the manuscript and participated in its design. All authors have read and approved the final manuscript.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




