Anti-TNF therapy is not associated with an increased risk of post-colectomy complications, a population-based study
Abstract
Aim
Previous studies have raised concerns that the use of anti-tumour necrosis factor (anti-TNF) therapy in patients with ulcerative colitis (UC) undergoing surgery may increase the risk of postoperative complications. We have taken a population-based approach to investigate whether there is an association between anti-TNF therapy and postoperative complications in UC patients undergoing subtotal colectomy.
Method
Hospital Episode Statistics (HES) data and procedural coding were used to identify all patients in England between April 2006 and March 2015 undergoing subtotal colectomy for UC. Patients were grouped into those who received anti-TNF therapy within 12 or 4 weeks of surgery and those who did not. The incidence of postoperative complications was evaluated by HES coding and compared between groups.
Results
In all, 6225 UC patients underwent subtotal colectomy. 753 patients received anti-TNF therapy within 12 weeks prior to surgery (418 within 4 weeks). There was no difference in postoperative complications between groups although groups were not comparable for age and comorbidities. Logistic regression with complications as the outcome variable did not show any significant association between anti-TNF therapy and complications. Colectomy performed during an unplanned admission (vs planned admission) and smoking were associated with complications.
Conclusion
This large population-based study does not demonstrate any association between preoperative anti-TNF therapy and postoperative complications in UC patients undergoing subtotal colectomy. The only variables associated with complications were colectomy performed during an unplanned admission and smoking.
What does this paper add to the literature?
Our study consists of a large population of all ulcerative colitis patients undergoing subtotal colectomy over 10 years in England to investigate an association between anti-tumour necrosis factor (anti-TNF) and postoperative complications. Unlike previous studies, we considered only one operation (subtotal colectomy) and assessed preoperative anti-TNF therapy within two time frames (4 and 12 weeks).
Introduction
Anti-tumour necrosis factor (anti-TNF) agents have been licensed in Europe since 2006 for the treatment of moderate to severe ulcerative colitis (UC), in patients who have had an inadequate response to, or are intolerant to, conventional therapy including corticosteroids, mercaptopurine or azathioprine 1. The pivotal ACT1 and ACT2 randomized placebo-controlled trials demonstrated that the anti-TNF agent infliximab, irrespective of any concurrent conventional therapy, approximately doubled the rates of the clinical response, clinical remission, steroid-free remission and mucosal healing compared with placebo 2.
There is evidence, however, of increased risk of serious infections in UC patients using anti-TNF agents compared to non-users 3. There has been concern regarding the potential septic postoperative complications attributable to the preoperative use of such potent immunomodulatory agents. One study demonstrated no increased risk of septic complications for UC patients undergoing surgery who received preoperative anti-TNF therapy compared to anti-TNF-naïve patients, although there did seem to be an increased risk of septic complications for those patients receiving anti-TNF therapy combined with cyclosporine A 4. Other studies investigating the risks of preoperative anti-TNF therapy have been confined to patients undergoing restorative proctocolectomy. Use of anti-TNF therapy has been shown to be an independent risk factor for anastomotic leak and two studies have demonstrated an increased risk of septic complications in anti-TNF treated patients undergoing restorative proctocolectomy compared to anti-TNF-naïve patients 5, 6. On the other hand, a meta-analysis has not demonstrated any association between preoperative use of anti-TNF agents and postoperative complications 7. The Crohn's and Colitis Foundation of America (CCFA) has issued a position statement stating that preoperative anti-TNF therapy may be associated with postoperative complications and that, while subtotal colectomy should be considered safe, one-stage proctocolectomy is contraindicated 8.
Anti-TNF agents may be used as rescue therapy to avoid colectomy in patients presenting with severe to moderately severe UC not responding to corticosteroids, as opposed to the traditional rescue agent, cyclosporine A. A randomized double-blind placebo-controlled trial demonstrated that anti-TNF rescue therapy more than halved the colectomy rate at 3 months compared with placebo 9. Nevertheless, a significant proportion of patients with refractory UC will fail to respond to anti-TNF agents necessitating urgent colectomy and exposing patients to the immunomodulatory effects of anti-TNF therapy in the immediate postoperative period 10.
Within the National Health Service (NHS) in England, all hospital admissions and operations are recorded in a national database. The use of anti-TNF agents is also recorded. The primary aim of this study was to compare postoperative complications for patients with UC undergoing subtotal colectomy, grouped by the preoperative use of anti-TNF agents, using data from national datasets.
Method
Hospital Episode Statistics (HES) data were used to identify patients undergoing a subtotal colectomy for UC. HES are data maintained by NHS Digital providing details of all NHS funded admissions to hospitals in England. Within the NHS in England, the anti-TNF agents infliximab, adalimumab and golimumab are classified as high cost drugs, the use of which must be coded to obtain funding using the Office of Population Censuses and Surveys (OPCS) Classification of Interventions and Procedures code, version 4.
Study population
All patients with a diagnosis of UC (International Classification of Disease, ICD-10 code K51) undergoing subsequent subtotal colectomy (OPCS-4 codes H05.2, H05.3, H05.8, H05.0, H29) between 1 April 2006 and 31 March 2015 made up the study population. The search was restricted to after 2006 as there was limited coding of anti-TNF therapy prior to this time. The following demographic data were extracted from HES as these variables were considered to be confounding factors for postoperative complications: age group, gender, Index of Multiple Deprivation (IMD), Charlson comorbidity score, smoking status, surgical approach, surgery occurring during an unplanned admission, and surgery within the same spell as the diagnosis of UC. Surgical approach was defined as either laparoscopic, laparoscopic converted to open or open. A planned admission, as defined by HES, is an admission where the decision to admit can be separated in time from the actual admission. An unplanned or emergency admission is one that is unpredictable and at short notice because of clinical need 11. The IMD is an official relative measure of deprivation for small areas in England made up of seven separate domains 12. The Charlson comorbidity index is a marker of comorbidity and was derived from HES secondary diagnosis codes as described previously 13, 14.
Anti-TNF therapy
Patients were defined as receiving anti-TNF therapy by the presence of the OPCS-4 code X92.1 occurring 12 or 4 weeks prior to the date of subtotal colectomy, termed ‘cases’. Patients not receiving anti-TNF therapy within this time frame were defined as the controls. These two groups of patients were compared for differences in postoperative complications.
Postoperative complications
A number of different postoperative complications were extracted (cardiovascular, pulmonary, gastrointestinal, neurological, renal/endocrine, infectious and wound problems) by way of ICD-10 diagnoses occurring within 30 days of the date of subtotal colectomy. This list of complications was chosen as it has been used previously in the context of colectomy for UC 15. The ICD-10 codes for the individual postoperative complications are listed in Appendix S1.
Comparisons between categorical data were tested for statistical significance using the chi-squared test. Associations with postoperative complications were examined with univariate and multivariate logistic regression, adjusting for anti-TNF therapy along with demographic variables. All data analysis was performed using STATA SE v14 (StataCorp LP, College Station, Texas, USA). P values < 0.05 were considered to be statistically significant.
Results
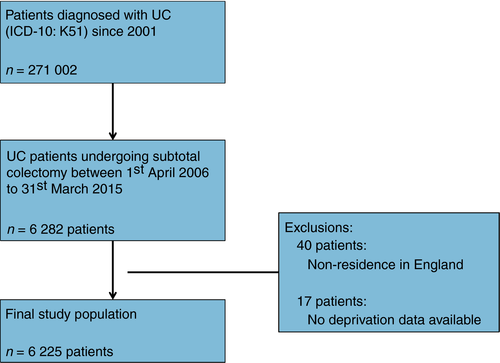
A total of 271 002 patients with UC were identified from HES data containing the ICD-10 code K51 since 2001. 6282 of these patients underwent subtotal colectomy within the stated time period. Forty patients were excluded as their recorded residence was outside England and a further 17 were excluded due to missing IMD or age, leaving a final study population of 6225 patients (see Fig. 1). 753 patients (12.1%) received anti-TNF therapy in the 12-week period prior to colectomy. A smaller group of 418 patients (6.7%) received anti-TNF therapy in the 4-week period prior to colectomy.
Patient demographics
The cases and controls were not comparable for all the retrieved demographic data (see Table 1). Patients receiving anti-TNF prior to colectomy were younger with fewer comorbidities than controls. Patients receiving anti-TNF were also more likely to undergo laparoscopic as opposed to open surgery. Colectomy was more likely to be an unplanned procedure for patients receiving anti-TNF within 4 weeks prior to colectomy compared to controls. There was no difference between groups in terms of gender, ethnicity or social deprivation.
| Variable | Anti-TNF therapy within 12 weeks of surgery | Anti-TNF therapy within 4 weeks of surgery | ||||
|---|---|---|---|---|---|---|
| Cases | Controls | P value | Cases | Controls | P value | |
| Total | 753 | 5472 | 418 | 5807 | ||
| Age group | ||||||
| < 18 | 66 (8.76%) | 218 (3.98%) | < 0.001 | 36 (8.61%) | 248 (4.27%) | < 0.001 |
| 18–30 | 253 (33.60%) | 1247 (22.79%) | 134 (32.06%) | 1366 (23.52%) | ||
| 31–50 | 255 (33.86%) | 1887 (34.48%) | 145 (34.69%) | 1997 (34.39%) | ||
| 51–70 | 155 (20.58%) | 1534 (28.03%) | 89 (21.29%) | 1600 (27.55%) | ||
| > 70 | 24 (3.19%) | 586 (10.71%) | 14 (3.35%) | 596 (10.26%) | ||
| Gender | ||||||
| Male | 441 (58.57%) | 3173 (57.99%) | 0.763 | 243 (58.13%) | 3371 (58.05%) | 0.973 |
| Female | 312 (41.43%) | 2299 (42.01%) | 175 (41.87%) | 2436 (41.95%) | ||
| Ethnicity | ||||||
| White | 683 (90.70%) | 4936 (90.20%) | 0.908 | 380 (90.91%) | 5239 (90.22%) | 0.675 |
| Asian | 39 (5.18%) | 301 (5.50%) | 19 (4.55%) | 321 (5.53%) | ||
| Other/unknown | 31 (4.12%) | 235 (4.29%) | 19 (4.55%) | 247 (4.25%) | ||
| Deprivation | ||||||
| 1 (most deprived) | 115 (15.27%) | 959 (17.53%) | 0.451 | 62 (14.83%) | 1012 (17.43%) | 0.214 |
| 2 | 162 (21.51%) | 1123 (20.52%) | 89 (21.29%) | 1196 (20.60%) | ||
| 3 | 163 (21.65%) | 1120 (20.47%) | 98 (23.44%) | 1185 (20.41%) | ||
| 4 | 168 (22.31%) | 1151 (21.03%) | 96 (22.97%) | 1223 (21.06%) | ||
| 5 (least deprived) | 145 (19.26%) | 1119 (20.45%) | 73 (17.46%) | 1191 (20.51%) | ||
| Charlson score | ||||||
| 0 | 611 (81.14%) | 4049 (73.99%) | < 0.001 | 345 (82.54%) | 4315 (74.31%) | < 0.001 |
| 1–4 | 99 (13.15%) | 788 (14.40%) | 47 (11.24%) | 840 (14.47%) | ||
| ≥ 5 | 43 (5.71%) | 635 (11.60%) | 26 (6.22%) | 652 (11.23%) | ||
| Smoking status | ||||||
| Smoker | 24 (3.19%) | 208 (3.80%) | 0.404 | 14 (3.35%) | 218 (3.75%) | 0.673 |
| Non-smoker | 729 (96.81%) | 5264 (96.20%) | 404 (96.65%) | 5589 (96.25%) | ||
| Surgical approach | ||||||
| Laparoscopic | 188 (24.97%) | 875 (15.99%) | < 0.001 | 100+a | 960 (16.53%) | < 0.001 |
| Laparoscopy converted to open | 7 (0.93%) | 80 (1.46%) | a | 85 (1.46%) | ||
| Open | 558 (74.1%) | 4517 (82.6%) | 313 (74.88%) | 4762 (82.00%) | ||
| Colectomy as unplanned date | ||||||
| Yes | 442 (58.70%) | 3178 (58.08%) | 0.339 | 304 (72.73%) | 3316 (57.10%) | < 0.001 |
| No | 311 (41.30%) | 2294 (41.92%) | 114 (27.27%) | 2491 (42.90%) | ||
| Colectomy during spell of UC diagnosis | ||||||
| Yes | 114 (15.14%) | 1358 (24.82%) | < 0.001 | 100 (23.92%) | 1372 (23.63%) | 0.890 |
| No | 639 (84.86%) | 4114 (75.18%) | 318 (76.08%) | 4435 (76.37%) | ||
- a Where numbers of patients are < 10, the data have been removed to prevent patient identification.
Postoperative complications
Overall there was no significant difference in the proportion of cases and controls experiencing complications within 30 days following surgery. This was true whether anti-TNF therapy had been administered within 12 weeks prior to surgery (12.4% vs 12.0%, P = 0.696) or within 4 weeks prior to surgery (12.9% vs 12.0%, P = 0.571). Table 2 shows a comparison of specific postoperative complications. The only factors significantly associated with postoperative complications by univariate analysis were performing colectomy as an unplanned procedure and smoking status. There was a trend to increased postoperative complications with increasing comorbidity (see Table 3).
| Complication | Cases, n (%) | Controls, n (%) | P value |
|---|---|---|---|
| Anti-TNF therapy within 12 weeks of surgery | |||
| Any complication | 94 (12.4) | 656 (12.0) | 0.696 |
| Gastrointestinal | 55 (7.3) | 349 (6.4) | 0.333 |
| Wounds | 16 (2.1) | 122 (2.2) | 0.855 |
| Infections | 35 (4.7) | 270 (4.9) | 0.733 |
| Renal/endocrine | a | 115 (2.1) | 0.095 |
| Cardiovascular | a | 95 (1.7) | 0.415 |
| Pulmonary | a | 50 (0.9) | 0.289 |
| Neurological | a | 8 (0.1) | 0.294 |
| Anti-TNF therapy within 4 weeks of surgery | |||
| Any complication | 54 (12.9) | 696 (12.0) | 0.571 |
| Gastrointestinal | 31 (7.4) | 373 (6.4) | 0.426 |
| Wounds | 10 (2.4) | 128 (2.2) | 0.801 |
| Infections | 19 (4.5) | 286 (4.9) | 0.728 |
| Renal/endocrine | a | 118 (2.0) | 0.399 |
| Cardiovascular | a | 100 (1.7) | 0.42 |
| Pulmonary | a | 52 (0.9) | 0.375 |
| Neurological | a | 8 (0.1) | 0.448 |
- a Where numbers of patients are < 10, the data have been removed to prevent patient identification.
| Variable | OR (95% CI) | P value |
|---|---|---|
| Use of preoperative anti-TNF therapy | Within 12 weeks | |
| No | 1 (baseline group) | – |
| Yes | 1.05 (0.83–1.32) | 0.696 |
| Use of preoperative anti-TNF therapy | Within 4 weeks | |
| No | 1 (baseline group) | – |
| Yes | 1.09 (0.81–1.47) | 0.571 |
| Age group | ||
| < 18 | 1 (baseline group) | – |
| 18–30 | 1.43 (0.97–2.10) | 0.073 |
| 31–50 | 1.03 (0.70–1.52) | 0.871 |
| 51–70 | 0.84 (0.57–1.25) | 0.389 |
| > 70 | 0.77 (0.49–1.21) | 0.258 |
| Gender | ||
| Male | 1 (baseline group) | – |
| Female | 0.90 (0.77–1.05) | 0.166 |
| Ethnicity | ||
| White | 1 (baseline group) | – |
| Asian | 0.72 (0.43–1.05) | 0.087 |
| Other/unknown | 0.95 (0.65–1.39) | 0.792 |
| Deprivation | ||
| 1 (most deprived) | 0.81 (0.63–1.05) | 0.109 |
| 2 | 0.92 (0.72–1.16) | 0.484 |
| 3 | 1.08 (0.86–1.36) | 0.499 |
| 4 | 0.90 (0.71–1.14) | 0.377 |
| 5 (least deprived) | 1 (baseline group) | – |
| Charlson score | ||
| 0 | 1 (baseline group) | – |
| 1–4 | 1.08 (0.78–1.50) | 0.629 |
| ≥ 5 | 1.26 (0.97–1.65) | 0.081 |
| Smoking status | ||
| Smoker | 1.60 (1.13–2.26) | 0.008 |
| Non-smoker | 1 (baseline group) | |
| Surgical approach | ||
| Laparoscopic | 1.16 (0.96–1.42) | |
| Laparoscopic converted to open | 0.86 (0.43–1.73) | 0.129 |
| Open | 1 (baseline group) | 0.680 |
| Colectomy as unplanned date | ||
| No | 1 (baseline group) | – |
| Yes | 1.38 (1.18–1.62) | < 0.001 |
| Colectomy during spell of UC diagnosis | ||
| No | 1 (baseline group) | – |
| Yes | 0.93 (0.78–1.12) | 0.444 |
- The outcome variable was any postoperative complication.
A multivariate logistic regression model was performed using any postoperative complication as the outcome variable with the use of anti-TNF therapy within 12 or 4 weeks preoperatively and all demographic variables listed in Table 1 as the covariates. Performing the colectomy as an unplanned procedure and smoking were the only variables that were statistically significantly associated with postoperative complications (see Table 4). The logistic regression model was then performed using gastrointestinal complications and infectious complications as the outcome variable. Again, colectomy as an unplanned procedure was significantly associated with these postoperative complications while smoking was only associated with gastrointestinal complications. Interestingly, laparoscopic as opposed to open surgery was associated with gastrointestinal complications. Performing colectomy during the same spell as the UC diagnosis was found to be significantly associated with fewer postoperative infectious complications (see Appendix S2).
| Variable | OR (95% CI) | P value | OR (95% CI) | P value |
|---|---|---|---|---|
| Preoperative anti-TNF therapy | Within 12 weeks | Within 4 weeks | ||
| No | 1 (baseline group) | – | 1 (baseline group) | – |
| Yes | 0.94 (0.74–1.19) | 0.585 | 0.95 (0.70–1.28) | 0.716 |
| Age group | ||||
| < 18 | 1 (baseline group) | – | 1 (baseline group) | – |
| 18–30 | 1.31 (0.89–1.94) | 0.177 | 1.31 (0.89–1.94) | 0.174 |
| 31–50 | 0.95 (0.64–1.40) | 0.796 | 0.95 (0.65–1.41) | 0.811 |
| 51–70 | 0.78 (0.52–1.17) | 0.222 | 0.78 (0.52–1.17) | 0.230 |
| > 70 | 0.70 (0.44–1.13) | 0.144 | 0.71 (0.44–1.13) | 0.150 |
| Gender | ||||
| Male | 1 (baseline group) | – | 1 (baseline group) | – |
| Female | 0.87 (0.75–1.02) | 0.091 | 0.87 (0.75–1.02) | 0.092 |
| Ethnicity | ||||
| White | 1 (baseline group) | – | 1 (baseline group) | – |
| Asian | 0.69 (0.47–1.02) | 0.062 | 0.69 (0.47–1.02) | 0.063 |
| Other/unknown | 0.93 (0.63–1.37) | 0.702 | 0.93 (0.63–1.37) | 0.705 |
| Deprivation | ||||
| 1 (most deprived) | 0.79 (0.61–1.03) | 0.081 | 0.79 (0.61–1.03) | 0.082 |
| 2 | 0.90 (0.71–1.14) | 0.379 | 0.90 (0.71–1.14) | 0.379 |
| 3 | 1.06 (0.84–1.34) | 0.627 | 1.06 (0.84–1.34) | 0.626 |
| 4 | 0.88 (0.69–1.37) | 0.303 | 0.88 (0.69–1.12) | 0.303 |
| 5 (least deprived) | 1 (baseline group) | – | 1 (baseline group) | – |
| Charlson score | ||||
| 0 | 1 (baseline group) | – | 1 (baseline group) | – |
| 1–4 | 0.99 (0.71–1.39) | 0.966 | 0.99 (0.71–1.39) | 0.959 |
| ≥ 5 | 1.04 (0.78–1.39) | 0.782 | 1.04 (0.78–1.39) | 0.785 |
| Smoking status | ||||
| Smoker | 1.56 (1.10–2.21) | 0.014 | 1.56 (1.10–2.21) | 0.013 |
| Non-smoker | 1 (baseline group) | – | 1 (baseline group) | – |
| Surgical approach | ||||
| Laparoscopic | 1.16 (0.95–1.43) | 0.145 | 1.16 (0.95–1.42) | 0.148 |
| Laparoscopic converted to open | 0.89 (0.44–1.79) | 0.744 | 0.89 (0.44–1.79) | 0.745 |
| Open | 1 (baseline group) | – | 1 (baseline group) | – |
| Colectomy as unplanned date | ||||
| No | 1 (baseline group) | – | 1 (baseline group) | – |
| Yes | 1.48 (1.25–1.76) | < 0.001 | 1.49 (1.25–1.76) | < 0.001 |
| Colectomy during spell of UC diagnosis | ||||
| No | 1 (baseline group) | – | 1 (baseline group) | – |
| Yes | 0.84 (0.69–1.01) | 0.068 | 0.84 (0.69–1.01) | 0.070 |
- The outcome variable was any postoperative complication.
Discussion and Conclusions
This is the largest study to date investigating postoperative complications following subtotal colectomy related to preoperative use of anti-TNF therapy. We have not been able to demonstrate any difference in postoperative complications attributable to the use of anti-TNF therapy in the 12 or 4 weeks prior to surgery. There were differences between the control and case groups as described but we were still unable to demonstrate an association between anti-TNF therapy and postoperative complications after statistically adjusting for demographic variables in a logistic regression model.
The potential association between anti-TNF therapy and surgical complications is controversial. A meta-analysis of 13 studies including 2933 patients did not show any such association 7, yet some studies have shown an increased risk of infectious complications and anastomotic leak from surgery associated with the preoperative use of anti-TNF therapy 4-6, 16, 17. The results of these studies have led the CCFA to advise against one-stage proctocolectomy in patients receiving anti-TNF therapy 8. Interestingly, anti-TNF therapy has also been associated with postoperative small bowel obstruction in paediatric patients 18. A potential association between anti-TNF therapy and postoperative infectious complications is not limited to UC patients. Some studies report an increased risk of infectious complications following gastrointestinal surgery in patients with Crohn's disease 19-22. There is similar controversy regarding a potentially increased risk of infectious complications following orthopaedic surgery for patients with rheumatoid arthritis receiving anti-TNF therapy 23.
One complicating issue may be the timing of anti-TNF therapy. The half-life of anti-TNF agents lies between 8 and 14 days and is effectively cleared from the serum by 8–10 weeks. The majority of studies investigating the association between anti-TNF and postoperative complications have defined use of anti-TNF as within 12 weeks of surgery 8. Differences in individual pharmacokinetics of anti-TNF agents may make it impossible to recommend a universal time period of anti-TNF cessation prior to surgery. A study of 123 patients with Crohn's disease and 94 with UC found an association between postoperative infectious complications, morbidity and readmission with preoperative serum anti-TNF drug levels. This association was only found for the Crohn's disease patients, but was possibly underpowered to show such an association in UC patients 20.
There is a paucity of guidelines to recommend an optimum time period between anti-TNF therapy and surgery to minimize postoperative complications. Urgent surgery for patients with UC may be required in acute disease and therefore the World Gastroenterological Organization stated that, if surgery is necessary for inflammatory bowel disease, it should not be postponed due to recent anti-TNF use 24. In rheumatoid arthritis patients awaiting joint surgery, it is recommended that cessation of therapy be weighed against the risk of a rheumatoid flare but, if therapy is to be stopped, cessation for 3–5× the half-life of the anti-TNF agent would be ideal 25. In practical terms for anti-TNF agents, this represents cessation of at least 4 weeks. For this reason, in our study we investigated the use of anti-TNF therapy within both 12- and 4-week periods prior to surgery.
The obvious confounding factor, associated both with the use of preoperative anti-TNF therapy and with postoperative complications, is the severity of UC at the time of operation. Unfortunately, we were unable to capture any data relating to UC severity in our study. Although severity scoring systems for UC exist 26, these data are not coded within HES. A few studies have managed to investigate the association of anti-TNF with postoperative complications and adjust for disease severity 5, 27-30. Some of these studies reported an increased risk of postoperative complications with anti-TNF therapy 5, 6, 29 while the others reported no such association 27, 28, 30. The design of our study also prohibits knowledge of the dose and timing of concomitant corticosteroids and other immunosuppressants in addition to anti-TNF therapy. HES data do not include any information regarding the use of such medications. Capture of data regarding steroid and other medication use necessitates access to individual health records at a local level which is outside the scope of our study. Preoperative corticosteroid use is associated with infectious postoperative complications and anastomotic leak 31, 32. Other confounding factors for which no data could be captured include body mass index, nutritional status as measured by body mass index or > 10% weight loss over 3 months 33, and intra-operative factors such as peritoneal contamination, blood loss and operative time 34. Nevertheless, we were able to adjust for other important factors that have previously been shown to be associated with postoperative complications such as comorbidity score, smoking status and emergency surgery 15. If the results of our study had demonstrated an increased risk of postoperative complications with preoperative anti-TNF therapy, the need to adjust for disease severity and use of other medications would be obvious.
It was interesting that laparoscopic surgery was not associated with a reduction in postoperative complications compared to open surgery and, in the sub-analysis, was actually associated with increased gastrointestinal complications. Laparoscopic compared to open subtotal colectomy is a longer operative procedure and our findings are consistent with others who have been unable to demonstrate any differences in 30-day postoperative complications between the two approaches 35.
The strength of our study is the population-based approach encompassing all NHS hospital admissions for subtotal colectomy in England. HES data perform relatively well for primary diagnoses with an accuracy of > 90% and the accuracy of recorded surgical procedures in recent years is also high 36. There is concern about how well HES captures postoperative complications, although capture improves with complication severity 15, 36. The complication rate in our study of 12–13% suggests effective capture and is consistent with complication rates reported in other studies 8.
In conclusion, our study has failed to demonstrate an association between postoperative complications and use of anti-TNF in the preoperative period. This is despite studying the use of anti-TNF within both 12- and 4-week preoperative time frames and adjusting for confounding variables in a multivariate model.
Conflicts of interest
All authors confirm that they have no conflicts of interest to declare.