Implant abutment material and surface modifications effect on human gingival fibroblast behavior
16324 Poster Display Clinical Research – Peri-Implant Biology
Background
Soft tissue around implant abutment serves as a barrier that protects underlaying bone from various hazardous agents. In case of a two-piece bone level dental implant, soft tissue sealing is formed around implant-abutment connection. Different materials and their surface modifications have shown to bear different biocompatibility properties. At present there is a growing amount of prosthetic materials on a market including new generation polymers and 3D printed materials.
Aim/Hypothesis
The aim of this study was to compare the effect of various ceramic and polymeric materials surfaces on the proliferation and adhesion of human gingival fibroblasts (HGF) using titanium as a positive control. The null hypothesis- there is no significant difference between prosthetic materials.
Material and Methods
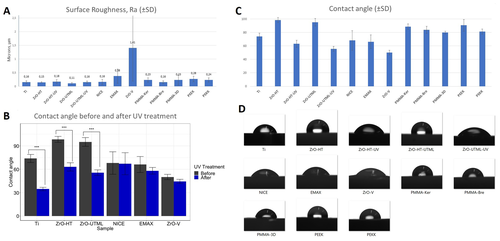
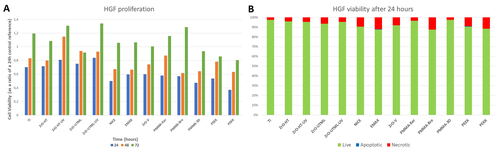
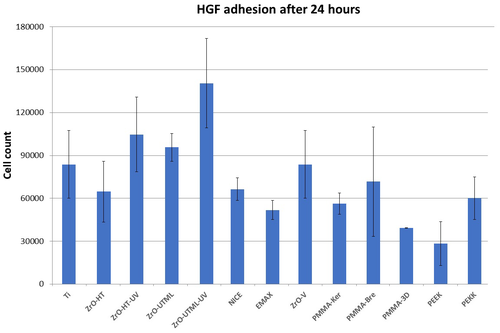
Materials tested- titanium (Ti), zirconium oxide ceramics high translucency (ZrO-HT) and multilayer (ZrO-UTML), lithium disilicate glass-ceramics (NICE, EMAX), ZrO veneered with feldspar ceramics and glazed (ZrO-V), two types of milled (PMMA-Bre, PMMA-Ker) and 3D printed polymethylmethacrylate (PMMA-3D), polyetheretherketone (PEEK), and polyetherketoneketone (PEKK). Specimens were cylinder shaped (5 mm width, 2 mm height) and polished according to manufacturer's recommendations. Surface roughness (Ra) was assessed using an optical imaging profiler. Photofunctionalization used UV-C light for 48 hours. Contact angle measurements were performed using Krüss EasyDrop system. For material toxicity and cellular adhesion evaluation, primary human gingival fibroblast cells were used. To evaluate the strength of cellular adhesion, gingival fibroblasts were cultured on the tested materials and subjected to lateral shear forces by applying 500 rpm shaking intensity.
Results
Ceramics and Ti surface roughness (Ra) values were in the range of 0.1–0.2 μm, except for EMAX (0.38 μm) and ZrO-V (1.4 μm) + polymeric materials’ Ra values were in the range of 0.15–0.3 μm (Fig. 1 A). Contact angles for Ti, ZrO-HT and ZrO-UTML groups reduced significantly (P < 0.05) after 48 hours treatment with UV (Fig. 1 B). Mean contact angles were decreasing in the following order ZrO-HT, ZrO-UTML, PEEK, PMMA-Ker, PMMA-Bre, PEKK, PMMA-3D, Ti, NICE, EMAX, ZrO-HT-UV, ZrO-UTML-UV, ZrO-V (Fig. 1 C, D). Each group showed increasing HGF viability over time (Fig. 2 A). No significant differences were observed comparing HGF viability between groups at any time period of proliferation. UV treated groups showed a tendency at 48 and 72 hours for increased HGF proliferation. Majority of non-vital cells after 24 hours were due to necrosis, apoptosis was uncommon (Fig. 2 B). HGF adhesion had a tendency to be higher for ZrO and Ti groups (Fig 3).
Conclusion and Clinical Implications
Majority of the tested materials had roughness values approaching recommended 0.2 μm threshold for fibroblast bacterial adhesion. Photofunctionalization of titanium and ZrO ceramics has a significant effect towards reducing the contact angle. UV treatment also has a tendency to favor HGF proliferation. The results of this study could help a clinician to select the most favorable prosthetic materials in certain situations in order to enhance soft tissue seal around dental implants and abutments.