Minimally Invasive Sinus Augmentation: A Systematic Review
Funding: No external funding, apart from the support of the author's institution was available for this study.
ABSTRACT
Aim
Technology improvement and a better understanding of sinus anatomy and wound healing in the past decade have allowed the development of minimally invasive surgical techniques. This systematic review focused on identifying and describing these techniques for vertical and lateral sinus augmentation (VSA and LSA).
Materials and Methods
Electronic and hand search were conducted to screen the literature published from January 2003 to May 2024. The selected studies had to include detailed techniques for minimally invasive SA. Data extraction included the study types, sample size, technique/instrument details, and outcome measurements.
Results
A total of 36 articles (27 VSA, 8 LSA with an additional 1 article included both procedures) with 2732 sinus augmentation met the inclusion criteria. Minimally invasive VSA includes the use of modified rotary instruments with stopper, balloon, hydraulic pressure, digital planning, endoscope, and operating microscope. These techniques aim for conservative flap reflection, precise sinus window preparation, and/or controlled sinus membrane elevation. Most of the selected studies (n = 15) did not report the incidence of sinus membrane perforation.
Conclusion
Within the limitations of this review, minimally invasive VSA and LSA achieved sufficient sinus augmentation and implant success with the potential advantages of reduced surgical complications and morbidity. Comparative studies with defined outcomes are encouraged to further validate these useful minimally invasive techniques for SA.
1 Introduction
Sinus augmentation (SA) is indicated to increase the alveolar ridge height in the posterior maxilla with inadequate height for placing standard-length dental implants [1]. After tooth extraction, alveolar bone resorption and sinus pneumatization are inevitable. SA surgery is common, especially at maxillary first molar tooth loss due to terminal periodontitis. With the advanced vertical loss of alveolar bone, up to two-thirds of these sites (67.40%) require SA procedure either with transcrestal/vertical sinus augmentation (VSA) when residual bone height is ≥ 5 mm (23.50%) or lateral sinus augmentation (LSA) (41.20%) when the bone height is < 5 mm [2].
In the traditional LSA approach, the lateral window outline was described to extend the outline to the anatomical limit of the maxillary sinus cavity, which is delineated as 1–2 mm from the sinus floor, 2–3 mm above the planned implant length, 1–2 mm from the anterior wall, and 5 mm distal to the most posterior planned implant site [3]. The window size of approximately 15 × 20 mm allows easy access. This traditional outline requires extensive flap reflection, large lateral window preparation, and a wide area of sinus membrane elevation to the medial wall. This extensive outline could lead to a higher incidence of sinus membrane perforation (SMP) [4] in approximately one-fifth of LSA procedures (21%), increased patient morbidity [5-10], inferior osteogenic potential, and slower bone maturation due to missing bony wall [11]. The prevalence of full edentulism decreased significantly in the US, from 18.9% to 4.9% during the half-century-spanning surveys [12]. The need for multiple implant placements along with large lateral window osteotomy preparation has been reduced. On the contrary, there is a greater need for replacing a single tooth gap with a smaller-sized window preparation.
The conventional osteotome approach for VSA used a blunt end osteotome with a mallet to compact autologous bone and the sinus floor. The compacted bone layer around the osteotomy site lifts the sinus membrane vertically until the desired length is achieved [13]. The main limitations of this technique are that during the surgical steps, the operator is blinded and based primarily on the individual's experience, and the detection of SMP is not feasible through insufficient visualization of the small osteotomy preparation. In addition, uncontrolled use of these instruments could create trauma to the membrane, eventually leading to membrane tears.
The advancement of surgical techniques, instruments, and digital implant planning for VSA and LSA may allow for a minimally invasive approach with better control and higher accuracy of surgical execution that could lead to more favorable treatment outcomes, less postoperative morbidity, enhanced safety and efficacy during surgery. The standard implant length is currently acceptable at 10 mm [14] and even a shorter implant, such as 8 mm can be used to evade possible morbidity or reduce treatment time [2, 15]. A minimally-invasive surgical approach for VSA and LSA using the use of specially designed sinus lift instruments augmented visualization from an operating microscope (OM) or endoscope, and the use of digital implant planning was introduced during the past decade as an alternative to conventional LSA [16]. Understanding the clinical outcome of these modified procedures could potentially result in the development of more simplified procedures with improved surrogate and patient-centered outcomes. Thus, this review aims to critically appraise the current literature on both VSA and LSA surgery by applying the minimally invasive concept using modified instruments, digital implant planning, and/or high magnification loupes/the OM, and/or an endoscope.
2 Material and Methods
This systematic review followed the preferred reporting items for systematic reviews and meta-analyses guidelines (PRISMA) [17, 18]. This systematic review has been registered on.
International prospective register of systematic reviews (PROSPERO) under registration number CRD42024538770.
3 Search Strategy
(1) Focused questions.
(1.1) Based on PICO principle;
(1) Population: Adult patients in need of LSA or VSA for one or more dental implant placements.
(2) Intervention (or exposure): Minimally invasive LSA or VSA involving the OM, loupes, an endoscopic approach, and digital implant planning of LSA or VSA irrespective of technique and technology used.
(3) Control (or comparator): Not applicable.
(4) Outcome of interest and the study design: Description and rationale of the minimally invasive LSA or VSA techniques in controlled clinical trials, case reports/series, and prospective or retrospective clinical studies.
(2) Study selection criteria.
- Studies had to have at least one patient receiving LSA or VSA for implant placement. Surgical techniques used for sinus augmentation had to be clearly described, involving the minimally invasive concept using modified instruments, digital implant planning, and/or high magnification loupes/the OM and/or an endoscope.
- Studies could have more than one group of participants receiving different sinus augmentation techniques.
- Studies had to report the total number of LSA or VSA procedures performed in all participants.
- In vitro studies, animal studies, narrative reviews, repeated reports with similar patients, communications, or expert opinions were excluded from this review.
- Articles not in English.
The primary outcome of this systematic review is the description and rationale of the minimally invasive sinus augmentation techniques. The event of intraoperative SMP was also recorded as a secondary outcome.
(3) Search strategy.
A search was conducted for studies published from January 2003 to May 2024 in MEDLINE (PubMed) using specific key terms (Appendix A Search Strategy). To broaden the scope of the electronic search and ensure inclusivity, four separate searches were performed to identify all articles meeting the inclusion criteria. The key term search is outlined as follows: ([sinus augmentation] AND [microsurgery]) AND ([sinus augmentation] AND [sinus lift]) AND (surgical guides) (((sinus augmentation) AND (sinus lift))) AND (minimally invasive) AND ((sinus augmentation) AND (sinus lift)) AND (lateral window). Furthermore, the reference list was screened to identify any additional articles that might meet the inclusion criteria.
4 Data Extraction and Data Synthesis
The titles and abstracts of all retrieved articles were independently screened by two authors (AR and BS). The full texts of potentially qualifying articles were examined. The third independent examiner (H-L C) was contacted in case of disagreement. If the selected articles had multiple group comparisons, only the group meeting the inclusion criteria was included. Data were independently extracted by the two authors (AR and BS) and compared. The accuracy of the data was confirmed by the third examiner (H-L C).
5 Assessment of Risk of Bias in the Included Studies
Study characteristics, quality, and heterogeneity were assessed by the Cochrane risk-of-bias tool for randomized trials for randomized controlled trials (RCT) [19], and risk of bias in non-randomized studies of interventions tools for non-RCTs [20] by two authors (AR and BS).
6 Results
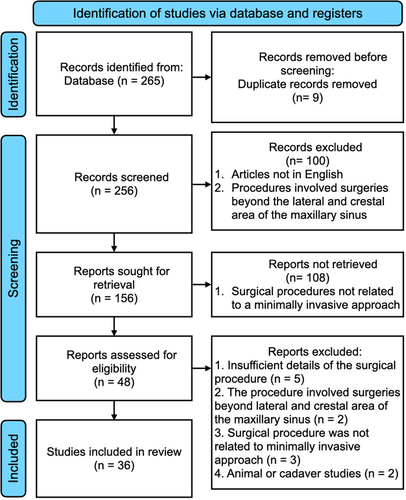
A total of 48 articles were selected for full-text review after screening 256 abstracts and titles (Figure 1); 12 articles were further excluded. The excluded articles and the reason(s) for exclusion are listed in Table 1. Finally, 36 articles with 2732 procedures in 1887 patients were included in this review. The selected studies included two RCTs, 10 prospective cohort studies, five retrospective studies, and 19 case series/reports (Table 2: Treatment strategies in selected articles).
| Reason | Author and year |
|---|---|
| Insufficient details of the surgical procedure | Choudhary et al. 2022, Dhandapani et al. 2016, Soardi et al. 2013, Soltan et al. 2011, Kfir et al. 2011. |
| The procedure involved surgeries beyond lateral and crestal area of the maxillary sinus | Kiyokawa et al. 2016, Kunihiro et al. 2014. |
| Surgical procedure was not related to minimally invasive approach | Balaji et al. 2013, Yamada et al. 2013, Santagata et al. 2010. |
| Animal or cadaver studies | Draenert et al. 2013, Zheng et al. 2014. |
| No. | Study | Study type/design | Follow-up time (months) | No. surgery | No. of participants | VSA | LSA | Guided | Details of the technique | No. of membrane perforation |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Engelke et al. 2003 | Retrospective | 6–60 | 118 | 83 | N | Y | N | Endoscope, 5 × 5 mm window, laterobasal of sinus | 28 |
| 2 | Chen et al. 2005 | Retrospective | 96 | 1557 | 1100 | Y | N | N | Hydraulic pressure from handpiece | N/A |
| 3 | Hu et al. 2009 | Case series | 15.9 +/− 2.94 | 28 | 28 | Y | N | N | Balloon | 2 |
| 4 | Trombelli et al. 2010 | Case report | 12 | 1 | 1 | Y | N | N | Rotating instrument with adjustable stoppers | 0 |
| 5 | Steiner et al. 2010 | Case series | N/A | 30 | 18 | N | Y | N | Hydraulic, microsurgical instruments | 0 |
| 6 | Trombelli et al. 2012 | RCT | 6 | 30 | 30 | Y | N | N | Rotating instrument with adjustable stoppers, compared xenograft and S-HA | 1 |
| 7 | Sisti et al. 2012 | Prospective | 24 | 20 | 17 | Y | N | N | Rotating instrument with adjustable stoppers | 0 |
| 8 | Penarrocha-Diago et al. 2012 | Case series | 12 | 6 | 6 | Y | N | N | Balloon, endoscope | 1 |
| 9 | Petruzzi et al. 2012 | Retrospective | 12 | 56 | 40 | Y | N | N | Balloon | 3 |
| 10 | Trombelli et al. 2014 | RCT | 6 | 38 | 38 | Y | N | N | Rotating instrument with adjustable stoppers, compared xenograft and β-TCP | 5 |
| 11 | Franceschetti et al. 2014 | Prospective | 6 | 45 | 45 | Y | N | N | Rotating instrument with adjustable stoppers | 3 |
| 12 | Better et al. 2014 | Case series | 6.7–13.1 | 23 | 18 | Y | N | N | Hydraulic pressure from implant channel | 0 |
| 13 | Nahlieli 2014 | Case series | 12 | 218 | 63 | Y | N | N | Hydraulic pressure from implant channel | N/A |
| 14 | Pozzi et al. 2014 | Prospective | 36–52 | 136 | 66 | Y | N | Y | Depth stop of the twist drill during osteotomy, VSA with osteotome through the surgical guide | N/A |
| 15 | Parthasaradhi et al. 2015 | Case series | N/A | 10 | 10 | Y | N | N | Disposable hand-torque blade until reaches the sinus membrane | N/A |
| 16 | Trombelli et al. 2015 | Case series | 6–36 | 5 | 3 | Y | N | N | Rotating instrument with adjustable stoppers | N/A |
| 17 | Isidori et al. 2015 | Prospective | 6.5 | 77 | 33 | Y | N | Y | Press-fit bone block at the osteotomy sites | N/A |
| 18 | Lopez et al. 2016 | Case report | N/A | 2 | 2 | Y | N | Y | Flapless, insertion of profiler and dispenser through the surgical guide | N/A |
| 19 | Zhou et al. 2017 | Case series | 6 | 12 | 11 | Y | N | N | Rotating instrument with adjustable stoppers | 0 |
| 20 | Tallarico et al. 2017 | Prospective | 6 | 29 | 18 | Y | N | N | Hydraulic pressure from implant channel | 0 |
| 21 | Gatti et al. 2018 | Prospective | 7 | 49 | 35 | Y | N | N | Hydraulic pressure from a rubber valve | 0 |
| 22 | Lopez-Quiles et al. 2018 | Prospective | 6 | 27 | 27 | Y | N | N | Balloon | 2 |
| 23 | Mudalal et al. 2019 | Case report | 6 | 1 | 1 | Y | N | N | Endoscope | 0 |
| 24 | Chaushu et al. 2020 | Retrospective | 12–36 | 50 | 50 | Y | N | N | Hydraulic pressure from implant channel | 0 |
| 25 | Attanasio et al. 2020 | Case report | 9 | 1 | 1 | Y | N | Y | Bone compactor through the guide | N/A |
| 26 | Stefanelli et al. 2020 | Prospective | 4 | 35 | 35 | Y | N | Y | Navigated antral bone expansion by navigation system and bone expander | N/A |
| 27 | Cho et al. 2020 | Prospective | N/A | 5 | 5 | N | Y | Y | Surgical guide with a slot extension for the conventional sinus window outline | N/A |
| 28 | Pardal-Pelaez et al. 2020 | Case report | N/A | 1 | 1 | N | Y | Y | Surgical guide with a slot extension for the conventional sinus window outline | 0 |
| 29 | Strbac et al. 2020 | Case report | 12 | 1 | 1 | N | Y | Y | Surgical guide with a slot extension for the conventional sinus window outline | 0 |
| 30 | Zadrozny et al. 2021 | Case report | 30 | 1 | 1 | Y | N | N | Hydraulic pressure from a rubber valve | N/A |
| 31 | Cecchetti et al. 2021 | Case report | N/A | 1 | 1 | N | Y | Y | Surgical guide with a slot extension for the conventional sinus window outline | N/A |
| 32 | Zaniol et al. 2021 | Retrospective | N/A | 28 | 22 | N | Y | Y | Surgical guide with a slot extension for the “Low Window” design | 0 |
| 33 | Sirinirund et al. 2021 | Case series | 6 |
20 12 VSA 9 LSA |
16 | Y | Y | N | OM during VSA and LSA surgery to safely elevate the membrane | 1 in VSA |
| 34 | Ntontoulos et al. 2023 | Case series | 6 | 8 | 5 | Y | N | N | Hydraulic pressure from Alb-CGF gel injection | N/A |
| 35 | Meneghetti et al. 2023 | Case series | 5 | 3 | 3 | N | Y | Y | Surgical guide with a slot extension for the conventional sinus window outline | N/A |
| 36 | Albadani et al. 2024 | Prospective | 60 | 12–36 | 60 | Y | N | N | Hand-torque the implant to tent the membrane, compared between immediate and delayed graftless VSA | N/A |
- Abbreviations: LSA, lateral sinus augmentation; N/A, not available; OM, operating microscope; RCT, randomized clinical trial; S-HA, synthetic hydroxyapatite in a collagen matrix; VSA, vertical sinus augmentation; β-TCP, β-tricalcium phosphate-based.
6.1 Quality Assessment and Heterogeneity Evaluation, Quality of Evidence
The two RCT studies showed a “low” overall risk of bias. Among 35 non-RCT, the overall “critical” risk of bias was assessed in 21 studies, with “serious”, “moderate”, and “low” risk of bias in 1, 11, and 1 study, respectively (Table 3).
| Assessment for RCT (ROB2) | |||||||
|---|---|---|---|---|---|---|---|
| Bias assessment | Randomization | Identification and recruitment | Deviations from intended interventions | Missing data | Measurement of the outcome | Selection of the reported result | Overall bias |
| Study | Risk of bias judgment (Low/some concerns/moderate/serious/critical/NI) | ||||||
| Trombelli et al. 2012 | Y | Y | PN | Y | N | Y | Low |
| Trombelli et al. 2014 | Y | Y | PN | PY | N | PY | Low |
| Assessment for non-RCT | |||||||
|---|---|---|---|---|---|---|---|
| Bias assessment | Confounding bias | Selection of participants | Classification of interventions | Deviations from intended interventions | Missing data | Selection of the reported result | Overall bias |
| Study | Risk of bias judgment (Low/moderate/serious/critical/NI) | ||||||
| Engelke et al. 2003 | PY | PY | N | Y | PN | PY | Serious |
| Chen et al. 2005 | PY | PY | PN | PN | PN | PY | Critical |
| Hu et al. 2009 | PY | PY | N | PN | PY | PY | Critical |
| Trombelli et al. 2010 | Y | Y | Y | PN | Y | Y | Critical |
| Steiner et al. 2010 | PY | Y | N | PY | PN | PY | Critical |
| Sisti et al. 2012 | PY | PN | Y | PN | PY | PN | Moderate |
| Penarrocha-Diago et al. 2012 | Y | PY | PN | PN | PN | Y | Critical |
| Petruzzi et al. 2012 | Y | Y | PY | Y | PN | PY | Critical |
| Franceschetti et al. 2014 | PY | PN | PY | PN | PY | PN | Moderate |
| Better et al. 2014 | PY | PN | Y | PN | PN | PY | Critical |
| Nahlieli 2014 | PY | PY | PN | PN | PN | Y | Critical |
| Pozzi et al. 2014 |
PY |
N | N | PN | PN | PN | Moderate |
| Parthasaradhi et al. 2015 | PY | PY | PY | PN | PY | N | Moderate |
| Trombelli et al. 2015 | Y | Y | Y | PN | Y | Y | Critical |
| Isidori et al. 2015 | PY | PY | N | PY | PY | PY | Moderate |
| Lopez et al. 2016 | PY | PY | Y | PN | PY | PY | Critical |
| Zhou et al. 2017 | PY | PY | N | PN | PY | Y | Critical |
| Tallarico et al. 2017 | PN | PN | N | PN | PY | PN | Low |
| Gatti et al. 2018 | PY | PN | Y | PY | PN | PN | Moderate |
| Lopez-Quiles et al. 2018 | PY | Y | N | PN | N | Y | Moderate |
| Mudalal et al. 2019 | Y | Y | N | PN | PN | PY | Critical |
| Chaushu et al. 2020 | PY | Y | PY | PY | PN | PY | Critical |
| Attanasio et al. 2020 | PY | PY | N | PN | PN | PY | Critical |
| Stefanelli et al. 2020 | PY | PY | N | PN | PN | PY | Moderate |
| Cho et al. 2020 | PY | PY | N | PN | PN | PY | Critical |
| Pardal-Pelaez et al. 2020 | PY | PY | N | PN | PN | PY | Critical |
| Strbac et al. 2020 | PY | PY | N | PN | PN | PY | Critical |
| Zadrozny et al. 2021 | PY | PY | N | PN | PN | PY | Critical |
| Cecchetti et al. 2021 | PY | PY | N | PY | PN | Y | Critical |
| Zaniol et al. 2018 | PY | PY | N | PN | PN | PY | Critical |
| Sirinirund et al. 2021 | PY | PY | Y | PN | PY | PY | Moderate |
| Ntontoulos et al. 2023 | Y | Y | N | PY | PY | Y | Critical |
| Meneghetti et al. 2023 | PY | PY | N | N | PY | PY | Moderate |
| Albadani et al. 2024 | PY | PN | Y | PN | PY | PY | Moderate |
- Abbreviations: N, No; NI, No Information; PN, Probably No; PY, Probably Yes; Y, Yes.
7 Minimally Invasive Vertical Sinus Augmentation
Several techniques and arrays of instruments have been implemented to increase success and reduce intraoperative surgical complications. Only two studies were RCT [21, 22], whereas others were prospective, retrospective studies, and case series/reports [23-29].
(1) Rotary instruments with safety features.
Adjustable stop devices have been added to manual and rotating instruments to prevent accidental penetration [21-24, 26]. After the probe drill which was set 1 mm short of the radiographic working length, the probe osteotome is then pushed until cortical bone resistance is felt through tactile sensation. The surgical working length was obtained from the probe and then used as a length for the stop device. Subsequent steps were completed, and a bone core and additional grafting materials were grafted into the sinus with a calibrated osteotome. A few incidences of SMP (ranging from 3.33% to 6.67%) were reported with the additional use of an adjustable stop device in two RCTs and a prospective study [21, 22, 24].
Stoppers were also used in combination with a slow-speed handpiece or special side-cutting rotating instruments to abrade the sinus floor [25, 28]. Both studies showed favorable treatment outcomes with one sinus membrane micro laceration and no evidence of graft extrusion into the sinus cavity.
Another study used a specially designed disposable hand-torque sinus lift system [27]. A special hand-torque blade was advanced into the osteotomy site until reaching the sinus membrane after osteotomy preparation. The membrane was lifted by curets with color markings through the crestal osteotomy site and then filled with biomaterials. Lastly, a recent prospective study proposed a graftless approach in freshly extracted sockets and healed sites [29]. The osteotomy preparation was completed at a 0.5 mm distance from the sinus floor. Then, the implant was placed with a hand wrench to anchor the sinus cortical bone and slowly tent the sinus membrane in an apical direction.
(2) Use of operating microscope.
An OM was used to perform minimally invasive VSA to inspect the integrity of the sinus membrane in twelve patients [30]. The magnification of 15 × to 20 × and illumination of the OM were used after the completion of either the conventional osteotome approach or the reverse drill protocol. One SMP was reported after the initial osteotomy preparation. No other postoperative complication was reported.
(3) Use of endoscope.
A case report used endoscopic evaluation after flapless implant placement with a conventional osteotome VSA in one patient [31]. The real-time observation of the sinus membrane movement and direct inspection of the membrane integrity assisted the clinician after using osteotome and platelet-rich fibrin insertion. No SMP was observed during the VSA procedure.
(4) Hydraulic pressure.
One of the early studies proposed the use of hydraulic pressure from the pressurized water of a round bur handpiece through a pinhole, which can be used to lift the sinus membrane [32]. The study showed a 99.99% implant survival rate with 8 implants failed out of 1577 implants during the 8-year follow-up period. However, the incidence of SMP and bone gain were not reported.
More recent studies implemented the use of saline pressure from a rubber valve connected to a tube syringe [33, 34]. After the complete removal of the sinus floor by a twist drill, approximately 2–3 mL of saline solution was administered to generate hydraulic pressure through the osteotomy site by a hydraulic elevation device and stabilized by finger pressure. During the hydraulic lifting, a gradual increase volume of saline was achieved by multiple cycles of pushing and drawing of a syringe. SMP was inspected by a lack of air bubbles in the syringe and water transition to the nasal cavity. Additional use of bone graft material in the osteotomy site is optional. None of the SMP was observed among 49 cases using this hydraulic system [33].
A case series used albumin concentrated growth factor (Alb-CGF) gel in combination with the use of a piezosurgery device to perform VSA [35]. Initial membrane detachment by a piezosurgical appliance, the sinus membrane was layered first with the CGF membrane. It was further elevated with the hydraulic pressure from the Alb-CGF gel injected from a syringe. Conventional bone grafting and implant placement were subsequently performed.
(5) Hydraulic pressure from an implant internal channel.
Three studies adopted specially designed implants with a 1.5-mm-diameter internal L-shaped channel that allows liquid injection from the lateral aspect of the implant to the apex into the maxillary sinus, causing hydraulic pressure to elevate the sinus membrane [36-38]. The implant length varied from 13, 14, 15.5, and 17 mm for the residual height of 4, 5, 6.5, and 8 mm, respectively [36, 37]. The osteotomy preparation was increased from a pilot drill to either a 3.2- or 4.2-mm final drill (for 4.2- and 5.0-mm implant, respectively) up to 1–2 mm from the sinus floor. The implant was advanced to penetrate the sinus by approximately 1 mm. Saline solution was used to inject into a tubing port of the implant for approximately 2–3 mL [37]. The physiologic bleeding from the retracted saline indicated that the implant tip was successfully placed into the sinus. After initial lifting, the saline was disconnected, and 1–3 cm2 of flowable bone graft was introduced by a syringe. The implant was then advanced until the platform matched the crestal bone level. All three studies with a total number of 99 implant surgeries reported no postoperative complication and no SMP evident in post-operative radiographs and CBCT.
Another variant of the implant with a straight internal channel was developed with multiple outlets at the implant apex (laterally and apically) that allow direct endoscope observation and a drug delivery system through the implant fixture [39]. Saline solution (1 cc) was injected and alternated with a 1-mm increment of implant advancement into the osteotomy preparation until the platform was leveled up with the crestal bone. Fracture of the sinus floor was detected by either physiologic bleeding from the implant channel or the endoscope that was inserted into the implant. The sinus membrane integrity was detected by the respiratory movement of the saline flowing in and out of the implant body. Seven of the 218 implants (3.2%) failed mainly from early infection within 2 weeks. The incidence of SMP was not reported.
(6) Balloon technique.
A balloon technique for VSA was initiated after initial osteotomy preparation and gentle sinus floor elevation by osteotomes [40]. The inflatable balloon was equipped with an inflator syringe and slowly inflated with saline solution until the desired elevation (> 10 mm) was achieved. Bone grafting and implant placement were then performed. One patient suffered from mild nose bleeding and two out of 28 VSA surgeries were aborted due to SMP.
Another retrospective study adopted a microscope to assist the balloon VSA surgery [41]. The author described the use of magnification of the microscope ranging from 4 to 16 × either in direct or indirect vision from incision making, sinus membrane elevation, and integrity evaluation, to suturing at the end of surgery. The balloon was placed between the sinus floor and the membrane, then inflated by saline solution from 2 to 4.5 mL to elevation < 20 mm of the elevation height. A syringe was then used to inject calcium sulfate solution and an implant was placed. Three SMPs were observed from 56 sites (two cases less than 1.5 mm and one case with 5 mm SMP). A similar case series reported the adjunctive use of an endoscope to visualize sinus membrane integrity [42]. The sinus floor was gently tapped by the osteotome, and an endoscope was inserted through the osteotomy site to inspect the integrity of the Schneiderian membrane. A latex balloon was then placed at the subantral space and slowly inflated multiple times with > 4 mL saline solution. One SMP was observed in six patients.
The balloon technique has been used in a staged approach for alveolar ridge height ≤ 4 mm [43]. The balloon was inflated and deflated slowly with a minimum number of five times until the required amount of lift was achieved. After the input valve was closed for a few seconds for membrane distension, the saline was drawn out and the xenograft was compacted. There were two cases of SMP, one with 2 mm in size, and 1 due to the balloon breakage.
(7) Guided minimally invasive vertical sinus augmentation.
Digital surgical guides for implant surgery have been incorporated into the minimally invasive vertical sinus augmentation approach [44-46]. Calibrated osteotomes 0.1 mm smaller than the sleeves of the surgical guide were tapped through the guide to help maintain the working length [46]. Bone compactors also have been used through the surgical guide to compress and expand the osteotomy site, which allows the fracture of the sinus floor and the elevation of the sinus membrane [45]. Another VSA technique incorporated a profiler and dispenser with the assistance of the surgical guide [46]. The profiler, a fixture-like with a smooth convex apex, was first inserted and lifted the sinus membrane 5–6 mm from the sinus floor. Second, a dispenser with a channel in the body to the apex was then introduced into the sinus. The sinus membrane was detached and lifted by the dispenser and the flow from a fluid biomaterial. None of the three studies reported the incidence of SMP.
Digital-guided implant surgery was used in staged cylindrical bone transplants in the VSA approach [47]. The cylindrical allograft or autogenous graft was harvested with a trephine bur 2 mm larger in diameter than the planned implant. The length of the graft is also slightly longer than the planned implant. For the recipient site, the osteotomy was prepared with a depth 2 mm short from the sinus floor and with a diameter 0.5 mm smaller than the block graft with a trephine bur at the implant-planned position. This allows primary stability of the press-fit harvested cylindrical graft. A circular bone window was created by a socket former, and the cylindrical graft was inserted until the level was flush with the crestal bone. The implants were placed at the planned positions after the healing phase with additional osteotome VSA if needed.
Navigated antral bone expansion adopted the use of a navigation system to assist in VSA by medial wall expansion and simultaneous implant placement [48]. The first step was to use a pilot drill in the available alveolar bone until reached 2 mm from the sinus floor with angulation relative to the ideal implant position. A bone expander was then inserted into the osteotomy site and the tip of the expander lifted the sinus wall laterally toward the sinus cavity. Both the pilot drill and the bone expander were navigated by the dynamic navigation system. After the sinus antral wall was lifted, the implant axis was then corrected by the bone expander. The standard protocol of the drilling sequence and the implant was also guided by the navigation system. The incidence of SMP was not reported. There were two palatal alveolar process fractures and three implants that used angled abutments to correct inaccuracy during implant placement surgery from a total of 37 cases.
8 Minimally Invasive Lateral Sinus Augmentation
(1) Hydraulic pressure.
Hydraulic pressure was integrated into a minimally invasive LSA procedure [49] with an adjunctive use of microsurgical instruments. When only a part of the sinus requires augmentation, a single osteotomy is adequate. A small lateral window (3 × 3 mm) was created sinus membrane was initially detached from the wall with a 1-mm round osteoid-shaped instrument. A ball-end instrument that elevated the sinus membrane from the floor to the medial wall. The small window was fitted with a syringe and hydraulic pressure was exerted by biocement injection. No SMP was reported in 29 cases.
(2) Guided minimally invasive lateral sinus augmentation.
Digital-guided LSA has been recently introduced to help surgeons define the outline of lateral window preparation [50-54]. Most of the included studies created a surgical guide with a rectangular or ovoid-shaped slot extension at the vestibular area of the planned implant position, allowing for precise window preparation. One study proposed the “Low Window” design the outline of the lateral window flush with the sinus floor and anterior wall to reduce inadvertent SMP [55]. The apical extent of the outline was determined at 6 mm from the sinus floor to reduce the need for flap reflection. Furthermore, the surgical angle accesses at the sinus floor and anterior wall were planned to have more than a 90° angle from the medial wall to facilitate surgical access and eliminate residual bone that could interfere with the membrane elevation. None of the SMP and postoperative complications were observed in 28 LSA interventions.
(3) Use of operating microscope.
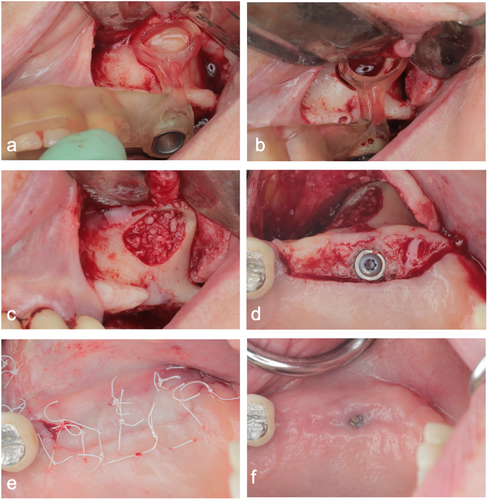
An OM was used to perform minimally invasive LSA and create a small lateral window (6 × 6 mm) [30]. The magnification (range from 8 × to 20 ×) and illumination of the OM were used during the osteotomy preparation of the lateral window and sinus membrane elevation. The integrity of the sinus membrane was also inspected prior to the placement of the bone graft, and the wound was closed with micro sutures. None of the LSA procedures had either postoperative complications or SMP (a total of nine cases).
Endoscope-assisted lateral sinus augmentation.
A retrospective study utilized the video endoscope for minimally invasive LSA [56]. A 5 × 5 mm osteotomy was located at the lateraobasal aspect of the maxillary sinus and the sinus membrane was detached with microsurgical instruments 2- and 4 mm in diameter. The window access was located at the most inferior aspect of the sinus cavity to facilitate the laterobasal tunneling. During the membrane elevation, the integrity of the membrane was inspected with 2.7 mm optic equipment. Twenty-eight of the LSA had SMP, accounting for a 23.73% perforation rate.
9 Discussion
Recently, the advancement of dental implant surfaces/design, bone grafts, and surgical instruments along with the improvement of surgical techniques have made it possible for clinicians to execute more minimally invasive sinus augmentation. Previous reviews showed a high success rate of sinus augmentation surgery [57, 58]. Despite this, the most common intraoperative complication was SMP, which was reported to account for 19.5% (0%–58.3%) [57] and 3.8% (0%–21.4%) [59] for LSA and VSA procedures, respectively. Development of sinus instruments, improved understanding of sinus anatomy and surgical techniques have changed the approaches for accessing the sinus in the past decade [9, 10, 60].
A recent review proposed the term minimally invasive VSA, such surgical intervention should have the following goals: (1) minimize intra- and postoperative morbidity, (2) reduce treatment time, and (3) simplify or eliminate the reconstructive procedures [61]. The review included only prospective controlled trials and most of the selected studies compare osteotome and drilling protocol with a limited number of studies that use hydraulic pressure, piezosurgery, and other alternative techniques. The authors suggested that the use of standardized sequence drills to access the sinus floor could help to reduce morbidity with less chair time and high patient acceptance. In this review, there is evidence that the use of rotary instruments with adjustable stoppers, hydraulic pressure, and balloon technique has been implemented in VSA to minimize the incidence of inadvertent SMP [21-28]. With these adjunctive features, in addition to the sequence drilling protocol from the previous review, an increase in the safety of the VSA procedures is anticipated.
Similarly, hydraulic pressure was also integrated into a minimally invasive LSA procedure [49]. The selected studies mostly were prospective/retrospective studies and case reports/case series. Only two studies were randomized clinical trials [21, 22], three studies reported zero SMP [23, 28, 33], and six studies did not report the incidence of SMP [26, 27, 32, 34, 35, 39]. Most of the studies used the Valsalva maneuver to detect the integrity of the sinus membrane. Alternatively, either the leak of saline from the hydraulic pressure technique into the nose or the presence of air bubbles in the retracted saline solution were used as an indicator for SMP.
Various SMP detection techniques among studies should be taken into consideration as the incidence of such adverse events as SMP during VSA is not always detected. A high incidence of SMP after 36 VSA procedures has been shown in an ex vivo study [62]. The perforation rate obtained by endoscopic evaluation was higher in the conventional osteotome method (66.7%) compared to the rotary instrument with adjustable stoppers (50%). One study used the endoscope to assist in the balloon approach and reported one incidence of SMP from six VSA procedures (16.67%) [42]. The high detection rate in this study may result from the direct observation of the sinus membrane from the endoscopic view. Hence, the method of sinus membrane inspection should be taken into consideration as it may affect the incidence of SMP and most of the selected studies did not report the incidence of the adverse event.
The need to inject liquid from the side of the L-shaped implant channel to elicit hydraulic pressure to the apex has made the length of the implant longer than the 10-mm standard length implant (range from 13 to 17 mm) [36-38]. The longer the implant implies the need for unnecessary greater elevation height and may pose a risk of SMP during implant placement. The implant that extrudes into the sinus during placement may exert extra pressure on the bone graft, potentially causing the breakage of the membrane and the dispersion of graft materials into the sinus cavity. All three studies reported zero SMP. However, it may not be feasible to evaluate the integrity of the sinus membrane when the implant was placed before sinus lifting and the authors did not provide any description of how the incidence of SMP was assessed. A maximum safety elevation threshold of 5 mm of VSA without bone graft and implant placement has been proposed in a cadaver model [62]. Further investigation may be needed to validate and prove the safety of the approach. Additionally, one study used specially designed implants with a straight implant channel that allows hydraulic pressure and endoscopic evaluation at the implant apex [39]. Nonetheless, the incidence of SMP was not reported.
Guided VSA surgery mainly uses the surgical guided as an adjunctive tool for osteotome, a dispenser, and a cylindrical graft to be inserted in the osteotomy site to maintain working length [44-46]. This approach had a similar rationale to a rotating drill with adjustable stoppers that prevents inadvertent SMP from uncontrolled osteotomy preparation. Another way for guided VSA is to use the dynamic navigation system that allows medial antral wall expansion [48]. Despite the advantages of real-time observation of the osteotomy preparation, adjacent vital structure, and verification of ideal implant position, care must be taken when using the bone expander to avoid palatal process fractures and adjusting the osteotomy drilling path to the accurate implant position.
Digitally guided LSA was used primarily to define the outline for conventional lateral window design [50-54]. Despite this, the term “minimally invasive” for guided LSA in this review implies that the surgical guide enhances the accuracy of the window preparation. The use of the guide does not entail a smaller window size or reduce the flap extension. Only one retrospective study suggested a small 6-mm height lateral window with the outline flush with the sinus anterior wall and the sinus floor or the “Low Window” technique [55]. The surgical angle of the osteotomy at the anterior and floor was recommended to be more than 90° to eliminate any undercut at the osteotomy margin that could block the surgical access for membrane detachment. The location of a small window when placed at the most mesial recess of the maxillary sinus could help clinicians to lower the SMP. The elimination of any residual bone wall increases access and facilitates membrane detachment. On the contrary, when the window is located more distally, this creates a “blind” condition to elevate the membrane. The advantage of a small window includes less flap reflection, facilitates surgical access, and less membrane elevation, which may lead to less incidence of SMP. This minimally invasive window preparation is similar to the microscope-assisted LSA procedure as the size of the window was about 6 mm in height [30].
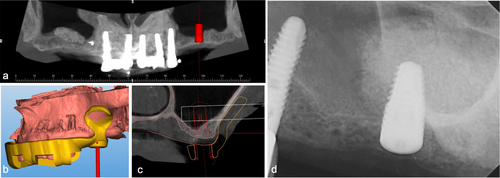
Adjunctive use of an OM during VSA and LSA has recently been advocated in the literature [30]. With superior visual magnification and enhanced illumination, an unparalleled visual advantage of osteotomy preparation, sinus membrane elevation, and assessment of the membrane integrity by direct observation are advantageous, compared to traditional VSA and LSA surgery (Figure 2, Video S1). The approach could potentially minimize intraoperative surgical complications due to undetected SMP, accelerate bone maturation, enhance early wound healing, and reduce postoperative morbidity [8, 11]. Compared to a larger conventional window outline that extends to anatomical limits, this may result in opposite less favorable outcomes in terms of inferior healing potential and more postoperative morbidity. Moreover, extensive membrane elevation may pose a risk for SMP, increase intraoperative bleeding, increase the use of biomaterials, and unstable containment of the grafted bone at the implant's planned location. Despite several benefits of using the OM, there is a higher learning curve with the use of the OM along with microsurgical instruments for LSA procedures.

Minimally invasive LSA compared to the traditional approach is more challenging. Limited visibility and access to lift the sinus membrane may need a higher level of manual dexterity, a specific microsurgical armamentarium for membrane detachment, and assistance from co-axial illumination from dental loupes or an OM. Hence, some exposure to conventional LSA and specific microsurgical training from experienced microsurgical clinicians may be required for training a minimally invasive LSA. Additionally, the difficulty assessment of the maxillary sinus is also necessary before planning the LSA surgery. The use of difficulty score systems has been implemented in other fields than implant dentistry [63, 64]. The LSA difficulty assessment could assist in surgical planning, foresee any anatomical obstacles, and predict the risk of intraoperative complications as well as an adjunctive tool for clinician–patient communication [65].
A paradigm shift of sinus augmentation surgery from the conventional to a more minimally invasive approach is that the membrane elevation needs to fulfill two purposes: (1) to maintain membrane integrity and (2) to increase the bone-to-implant contact [16]. Depending on the residual bone height, the sinus membrane is manipulated differently. With digital guided implant planning, the precision of the location of the window is improved. The extent of the sinus membrane elevation could be limited to the area where the implant will be placed (Figures 3 and 4). The elasticity of the sinus membrane allows detachment and distension of the membrane from the pressure of the bone replacement graft. Thus, the need to gain an elevation height of the membrane to the implant apex and 5 mm distal to the most posterior planned implant site may not be mandatory. Regardless of the benefit of using guided LSA, extensive flap reflection for the lateral window guide positioning may result in inferior healing outcomes (Figure 4f). Furthermore, short implants have gained popularity over the past decade as an alternative treatment option for atrophic maxilla with acceptable clinical and patient-reported outcomes [66, 67]. Therefore, the need for extensive sinus augmentation may be gradually diminished.
Limitations of this current systematic review included substantial heterogeneity with the study design, which carries a moderate to critical risk of bias and inconsistent complication reporting (15 studies with no report on the incidence of SMP). Only two randomized clinical trials with a low risk of bias that met the inclusion criteria were selected. Consequently, the benefits of the minimally invasive surgical approaches and the adjunctive use of OM, endoscope, and guided sinus augmentation still need to be explored. Future randomized clinical trials are required to ideally assess and compare the benefits of minimally invasive VSA and LSA in terms of bone maturation, accuracy of bone graft placement at the planned implant position, incidence of intraoperative complications, cost-effectiveness, and patients' reported outcomes. Lastly, the implementation of microsurgical instruments along with the magnification and illumination of the OM and endoscope may enhance sinus complication management.
10 Conclusion
Modified instruments, digital planning, endoscopes, and OM have been identified in the literature to execute minimally invasive VSA and LSA procedures. Although the methods to detect adverse events among these studies are inconsistent, these minimally invasive techniques aiming for conservative flap reflection, precise sinus window preparation, and controlled membrane elevation may result in accelerated healing, fewer complications, and less patient morbidity. Comparative studies with defined outcomes are encouraged to validate these minimally invasive sinus augmentation techniques.
Author Contributions
Drs. Benyapha Sirinirund and Hsun-Liang Chan contributed to the conception of the study, provided the design of the study, and performed critical revisions of the manuscript. Drs. Benyapha Sirinirund and Amanda B. Rodriguez Betancourt performed an article review and collected data. Drs. Benyapha Sirinirund, Amanda B. Rodriguez Betancourt, and Hsun-Liang Chan provided data analysis and interpretation. Drs. Yu-Chang Wu and Riccardo Scaini assisted in data management and manuscript writing. All authors helped prepare the manuscript, gave their final approval, and agreed to be accountable for all aspects of the work.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A: Search Strategy
(“paranasal sinuses”[MeSH Terms] OR (“paranasal”[All Fields] AND “sinuses”[All Fields]) OR “paranasal sinuses”[All Fields] OR “sinus”[All Fields] OR “sinus s”[All Fields]) AND (“augment”[All Fields] OR “augmentation”[All Fields] OR “augmentations”[All Fields] OR “augmented”[All Fields] OR “augmenting”[All Fields] OR “augments”[All Fields]) AND ((“paranasal sinuses”[MeSH Terms] OR (“paranasal”[All Fields] AND “sinuses”[All Fields]) OR “paranasal sinuses”[All Fields] OR “sinus”[All Fields] OR “sinus s”[All Fields]) AND (“lifting”[MeSH Terms] OR “lifting”[All Fields] OR “lift”[All Fields])) AND ((“surgical procedures, operative”[MeSH Terms] OR (“surgical”[All Fields] AND “procedures”[All Fields] AND “operative”[All Fields]) OR “operative surgical procedures”[All Fields] OR “surgical”[All Fields] OR “surgically”[All Fields] OR “surgicals”[All Fields]) AND (“guide”[All Fields] OR “guided”[All Fields] OR “guides”[All Fields] OR “guiding”[All Fields])). In addition the second search was: (“paranasal sinuses”[MeSH Terms] OR (“paranasal”[All Fields] AND “sinuses”[All Fields]) OR “paranasal sinuses”[All Fields] OR “sinus”[All Fields] OR “sinus s”[All Fields]) AND (“augment”[All Fields] OR “augmentation”[All Fields] OR “augmentations”[All Fields] OR “augmented”[All Fields] OR “augmenting”[All Fields] OR “augments”[All Fields]) AND (“microsurgery”[MeSH Terms] OR “microsurgery”[All Fields] OR “microsurgeries”[All Fields]). Third search terms were: (“paranasal sinuses”[MeSH Terms] OR (“paranasal”[All Fields] AND “sinuses”[All Fields]) OR “paranasal sinuses”[All Fields] OR “sinus”[All Fields] OR “sinus s”[All Fields]) AND (“augment”[All Fields] OR “augmentation”[All Fields] OR “augmentations”[All Fields] OR “augmented”[All Fields] OR “augmenting”[All Fields] OR “augments”[All Fields]) AND ((“paranasal sinuses”[MeSH Terms] OR (“paranasal”[All Fields] AND “sinuses”[All Fields]) OR “paranasal sinuses”[All Fields] OR “sinus”[All Fields] OR “sinus s”[All Fields]) AND (“lifting”[MeSH Terms] OR “lifting”[All Fields] OR “lift”[All Fields])) AND (“minimally”[All Fields] AND (“invasibility”[All Fields] OR “invasible”[All Fields] OR “invasion”[All Fields] OR “invasions”[All Fields] OR “invasive”[All Fields] OR “invasively”[All Fields] OR “invasiveness”[All Fields] OR “invasives”[All Fields] OR “invasivity”[All Fields])).
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.