Increasing normality–persisting barriers: Current socio-demographic characteristics of 350 individuals diagnosed with gender dysphoria
Funding information
This research did not receive any specific grant from any funding agency in the public, commercial or nonprofit sector.
Abstract
Introduction
The number of individuals requesting medical treatment for gender dysphoria has increased significantly within the past years. Our purpose was to examine current biographic and socio-demographic characteristics and aspects of legal gender reassignment.
Design
Medical files from n = 350 individuals of a German Endocrine outpatient clinic were collected from 2009 to 2017 and analysed retrospectively.
Results
Ratio of transwomen to transmen equates to 1:1.89 with a remarkable increase of transmen by the year 2013, showing a reversal of gender distribution compared with previous studies for the first time. Use of illegal substances or self-initiated hormone therapy was rare (4.6 and 2.1%). Satisfaction with gender-affirming hormone therapy was significantly higher in transmen than in transwomen (100% vs 96.2%, P = .005). Use of antidepressants declined significantly after onset of hormone treatment in transmen (13% vs 7%; P = .007). The number of individuals with a graduation diploma was only about half as high as in the general population (14.3% vs 27.3%), whereas unemployment rate was more than twice as high (14% vs 6.9%). Median latency between application for legal gender reassignment and definitive court decision was 9 months.
Conclusions
Our data provide possible indications for a decline of psychosocial burden in individuals diagnosed with gender dysphoria over the last years. However, affected individuals are still limited in their occupational and financial opportunities as well as by a complex and expensive procedure of legal gender reassignment in Germany.
1 INTRODUCTION
Gender dysphoria, formerly most commonly termed as transsexualism, is defined as the affliction resulting from discrepancy between somatic sex and subjectively perceived gender. The number of individuals affected, respectively, the number of individuals who ask for medical treatment has markedly increased over the past years.1
However, former biographic and socio-demographic data about individuals diagnosed with gender dysphoria were mostly gathered in rather small patient populations. Most of the earlier studies show a ratio between transwomen (individuals who self-identify as female but were assignated as male at birth) and transmen (individuals who self-identify as male but were assignated as female at birth) of 2:1,1-4 whereas in later studies, the proportion of transmen seems to adjust.5 The average age at the first medical consultation for gender-affirming treatment is reported to be lower in transmen than in transwomen.2, 3, 6-8 Some studies show higher unemployment rates in individuals diagnosed with gender dysphoria, especially in transwomen.2, 8 Individuals affected seem to live less frequently in a permanent partner relationship, transwomen even less frequent than transmen.2, 3, 7 Among people diagnosed with gender dysphoria, a proportion of 50% cigarette smokers has been described which is higher compared with 28% cigarette smokers in the general population of the European Union.2, 6 Furthermore, an above-average consumption of illegal substances of up to 43% has been described.3 Nearly, all studies point out a high satisfaction level with the gender-affirming therapy, a decline of depressive symptoms9, 10 and very low rates of misdeterminations.1, 4
Standards of care for gender dysphoria were first defined in 1979 by the World Professional Association for Transgender Health (WPATH)11 and are updated regularly since then. In 2017, the evidence-based clinical practice guideline of the Endocrine Society for endocrine treatment of individuals diagnosed with gender dysphoria was published.12 According to this clinical practice guideline, our outpatient clinic, as most other centres in Germany, requires a written confirmation of gender dysphoria and an indication for treatment from a qualified mental health professional to initiate a gender-affirming hormone therapy (GAHT). The majority of German healthcare providers cover the costs of GAHT, if these requirements are met.
In contrast to this well-defined, internationally developed recommendations for the diagnosis of gender dysphoria and gender-affirming medical treatment, there are still considerable differences regarding admission requirements and legal aspects of gender reassignment between different countries even within the European Union. While in Germany, the decision for legal gender reassignment is under the jurisdiction of the responsible district court and requires two independent expert opinions which confirm the diagnosis of transsexualism and the stability and continuity of gender incongruence for at least 3 years, in other European countries (e.g. Denmark, Ireland, Norway and Belgium) an application to a competent administrative authority is enough. So far, there are few data about chronological correlation of medical and legal aspects of gender reassingment. The heterogeneity of legislations and the sociocultural differences between countries make it difficult to compare the available data.
The aim of this study was to examine biographic and socio-demographic characteristics, treatment satisfaction and aspects of legal gender reassignment in a reliable German population.
2 SUBJECTS AND METHODS
Since its foundation in January 2009 until March 2017, n = 533 individuals presented in our Endocrine outpatient clinic for gender dysphoria with the desire for GAHT. Thereof, n = 88 had already started GAHT and asked for endocrinological follow-up, and in n = 95, the written indication for treatment from a qualified mental health professional that is required before initiating GAHT was still outstanding at the time of data analysis. These individuals were therefore excluded from our analysis. Consequently, data from n = 350 individuals who started and continued GAHT under our medical attendance were analysed. Thereof, n = 310 had a time of follow-up after onset of GAHT of at least 10-14 months. All data were collected retrospectively from medical files.
Treatment of individuals diagnosed with gender dysphoria in our outpatient clinic is performed by a small team of trained physicians under supervision of one senior staff member and following a defined process according to the clinical practice guideline.12 In order to provide an efficient and safe GAHT, a thorough medical history, which involves pre-existing medical conditions and medications as well as legal and illegal drug use, is a central aspect of the first clinical interview. Further questions about sexual orientation, desire to have children and partnership are necessary for advices on contraception, possible changes in sexual life and fertility and therefore elementary in our first anamnesis. For a better understanding of the individual´s distress and wishes and to determine a possible need for support, the anamnesis is complemented by a social anamnesis that includes questions about their age of onset of feelings of gender incongruence, the status of social gender role transition, educational qualification and work life. After onset of GAHT, a regular follow-up is performed every 3-6 months during the first year and every 6-12 months afterwards. Besides clinical and laboratory examinations, questions about subjective effects of GAHT, possible side effects, new medical conditions, changes in co-medication as well as status of legal gender assignment are ask in every visit. To estimate treatment satisfaction, individuals are regularly interviewed if GAHT leads to a subjective improvement of their overall situation and whether they feel any doubts about their decision to start treatment. Data are documented in an individual IT-based medical file.
The study was approved by the local ethical committee (permit no.185/16).
Significances were calculated using chi-square contingency tables and corrected using the Bonferroni-Holm method or by the Wilcoxon-Mann-Whitney U test to compare categories. To compare the use of antidepressants before and 10-14 months after start of GAHT, McNemar's test was performed. Statistical analysis was performed using the statistical software BiAS 11.05. Significance was accepted for values of P < .05.
3 RESULTS
Results are summarized in Table 1.
| Total (n = 350) | Transwomen (n = 121) | Transmen (n = 229) | P | |
|---|---|---|---|---|
| Age at first presentation, Median (range) years | 22 (14-60) | 25 (14-60) | 21 (14-52) | <.001 |
| Manifestation prepubertal, % | 60.6 | 50.4 | 65.94 | .005 |
| Manifestation postadolescent, % | 1.14 | 3.31 | 0 | .006 |
| Graduation diploma, % | 14.29 | 18.18 | 12.23 | .13 |
| Unemployed, % | 14 | 19.01 | 11.35 | .154 |
| Employed, % | 41.7 | 39.7 | 42.6 | |
| Pupils/students, % | 36.9 | 32.2 | 39.3 | |
| Permanent relationship, % | 28.57 | 23.14 | 31.44 | .186 |
| Genetical-related parenthood, % | 6.29 | 14.05 | 2.18 | <.001 |
| Cigarette smoking, % | 36.57 | 21.49 | 44.54 | <.001 |
| Former smokers, % | 8 | 11.57 | 6.11 | .074 |
| Current or former use of illegal drugs, % | 4.57 | 4.96 | 4.37 | >0.2 |
| Contact to a trained mental health professional in advance, % | 93.43 | 93.39 | 93.45 | >.2 |
| First documented professional contact in our clinic, % | 5.43 | 5.79 | 5.24 | >.2 |
| Latency between onset of psychotherapeutic attendance and onset of GAHT, Median (range) month | 9 (2-178) | 10 (2-178) | 9 (2-158) | .083 |
| Social gender role transition in advance, % | 70.57 | 65.29 | 73.36 | >.2 |
| latency between onset of GAHT and legal gender reassignment, Median (range) month | 12 (−28-61) | 13 (2-60) | 12 (−28-61) | >.2 |
| Self-initiated GAHT, % | 2.06 | 5.17 | 0.45 | <.001 |
| Subjective improvement of overall situation after onset of GAHT, % | 98.71 | 96.15 | 100 | .005 |
| Doubts about decision to start treatment with GAHT, % | 0.96 | 2.88 | 0 | .037 |
- Significant differences between transwomen and transmen are indicated in bold.
In our cohort of 350 individuals, n = 121 were transwomen and n = 229 transmen resulting in a ratio of transwomen to transmen of 1:1.89. Since its foundation in 2009, we treat more transmen than transwomen in our Endocrine outpatient clinic for gender dysphoria. By the year 2013, we can observe a remarkable, though not significant, increase of this ratio (P = .076; Table 2).
| Transwomen (n) | Transmen (n) | Sex ratio | P | ||
|---|---|---|---|---|---|
| 2009-2010 | 10 | 13 | 1:1.30 | 1:1.37 | .076 |
| 2011-2012 | 28 | 39 | 1:1.39 | ||
| 2013-2014 | 39 | 87 | 1:2.23 | 1:2.13 | |
| 2015-3/2017 | 44 | 90 | 1:2.05 | ||
GAHT was implemented according to current clinical guidelines in all individuals.13, 14 In transmen, testosterone undecanoate intramuscularly was used in 76.4% (dosage: 1000 mg every 10-17 weeks, median of 12 weeks), transdermal testosterone gel in 23.6% (dosage: 25-75 mg/d, median of 50 mg/d). In about ¼ of transmen, a preceding or concomitant therapy with progestins or GnRH agonists was performed to assist menstrual cessation. Transdermal formulations of oestradiol in transwomen were applied in 52.9%, thereof transdermal gels in 89% (dosage: 1.5-6 mg/d, median of 2.25 mg/d) and transdermal patches in 11% (dosage: 0.1 mg/d). Oral formulations of oestradiol valerate, respectively, hemihydrate (dosage: 3-10 mg/d, median of 6 mg/d) were used by 47.1% of transwomen. Antiandrogenic medication was established with cyproteronacetate in 71.5% (dosage: 10-50 mg/d, median of 25 mg/d). Spironolactone was used in 5.6% (dosage 50-100 mg/d, median of 100 mg/d), and combinations of both in 5.6%. 17.4% of transwomen refused to use antiandrogens. Antiandrogen medication was discontinued at the time of gonadectomy.
Median age at first presentation in our outpatient clinic was 22 years. Transmen presented at a significantly lower age. An initial manifestation of gender dysphoria before the onset of puberty was reported by the majority of individuals, but was significantly more frequent in transmen than transwomen. Manifestation after adolescence was rare in transmen and did not occur in transwomen of our study cohort.
About 14.29% of the individuals achieved graduation diploma. There were no significant differences between transmen and transwomen. The percentage of unemployed in our cohort was 14%, also with no significant difference between both genders.
Less than a third stated a permanent partnership at the time of their first presentation. Genetical-related parenthood was recorded in 6.29% of all individuals and was significantly more frequent in transwomen compared with transmen.
The proportion of cigarette smokers was about one third. Nicotine consumption was recorded more than twice as often in transmen compared with transwomen (P < .001) and more transwomen than transmen stopped smoking in advance, albeit not significant. A current or former consumption of illegal drugs was less than 5% in both groups without significant gender differences.
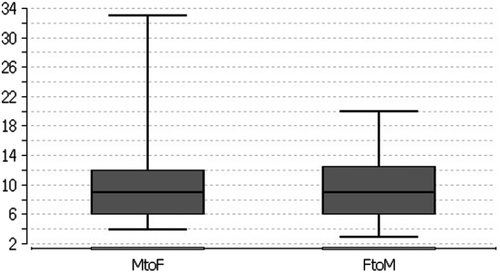
A broad majority of individuals that came to our outpatient clinic contacted a trained mental health professional in advance. Our clinic was the first documented professional contact regarding gender dysphoria in 5% of the cases. These individuals were referred to a mental health professional before starting hormonal treatment. Median latency between onset of psychotherapeutic attendance and GAHT was 9 months without differences between transwomen and transmen. Social gender role transition took place in about 70% before the first contact with our clinic, more frequently, however, not significant, in transmen. Legal gender reassignment was already realized in a very small proportion of individuals at the first presentation at our clinic. During evaluation period, legal gender reassignment was implemented in more than half of the individuals. Median latency between onset of GAHT and legal gender reassignment was 12 months without significant differences between transmen and transwomen. The median time between application for legal gender reassignment and definitive court decision was 9 months with a range from 3 to 33 months (Figure 1).
GAHT was initiated by a medical specialist in most individuals. The proportion of self-initiated hormone therapies was significantly higher in transwomen (5.2% in transwomen vs 0.45% in transmen, P < .001).
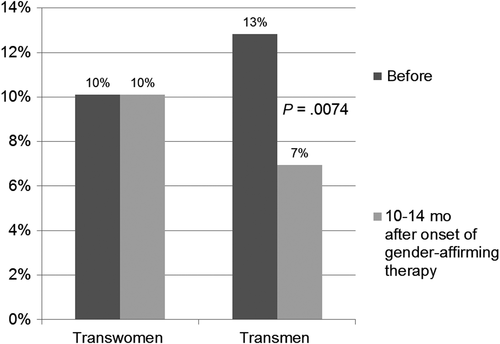
Retrospectively, a broad majority of 98.7% reported an improvement of their overall situation after onset of GAHT. Improvement through GAHT was significantly more often reported by transmen than by transwomen (100% vs 96.2%, P = .005). Doubts about their decision to start treatment were raised by few transwomen but no transmen. None of the individuals rated their decision for GAHT as false. In transmen, the use of antidepressants declined significantly 10-14 months after onset of hormone treatment (n = 24, 13% vs n = 13, 7%; P = .007). This association could not be observed in the group of transwomen (Figure 2).
4 DISCUSSION
Our outpatient clinic was founded in 2009 and is part of a regional network of mental health professionals, gynaecologist and surgeons specialized for diagnosis and medical treatment of gender dysphoria. The established system is working in accordance with the standards of care11 and current evidence-based clinical practice guideline,12 leading to a high proportion of more than 90% of individuals that went to a trained mental health professional before the request for gender-reassignment treatment. In our cohort, we recorded a very small percentage of <2.5% with self-initiated GAHT compared with previous studies with up to more than 50%.3, 8 In line with these former evaluations from other European countries,2, 3, 8 a significantly higher proportion of self-initiated hormone therapies in transwomen compared with transmen was still observed. One possible reason could be an easier availability of oestradiol derivates, for example contraceptive pills. Furthermore, the therapeutic need is possibly higher in transwomen, whereas transmen are more likely to receive social acceptance, even before GAHT is initiated. However, notably, we observe an earlier manifestation of gender dysphoria in transmen who are in average 4 years younger than transwomen at the time of their first consultation for gender-reassignment medical treatment. This effect was also shown in several previous studies.2, 3, 6-8
In the 8 years analysed, nearly twice as many transmen than transwomen came to our outpatient clinic. We recorded a higher proportion of transmen than transwomen in our Endocrine outpatient clinic for gender dysphoria since its foundation in 2009. By the year 2013, we could observe a remarkable increase of this ratio. Since previous studies predominantly show a distinct preponderance of transwomen,1-4 more recent analyses indicate an adjustment of gender ratio over time.5 Our study is, to our knowledge, the first showing a reverse ratio. One possible reason could be the increasing pretherapeutic communication between affected individuals via social media where recommendations for certain centres are given. However, since specialized treatment centres for gender dysphoria are still rare, it does not solely explain sufficiently this remarkable result and the reasons need to be further analysed.
Our data verify–as described before9, 10–that a broad majority appraise GAHT as a subjective improvement of their overall situation. Doubts about decision to start treatment were raised in only a very few number of transwomen, though none of the individuals evaluated its decision as false retrospectively. The use of antidepressants as a surrogate marker for concomitant depressive symptoms was almost reduced by half 10-14 months after onset of GAHT in transmen. In addition to that, we could observe a significantly higher proportion of transmen than transwoman who appraised GAHT as an improvement of their overall situation, a result which had also been shown before.15 Possible explanations for this remarkable difference between transmen and transwoman are a faster and more convincing change of physical features, a therefore easier reversion of gender role and maybe also in general less self-critical perception of gender role in transmen. A further potential reason for the significant decline of antidepressant co-medication in transmen but not in transwomen could be the fact that depressive symptoms are a possible side effect of cyproteronacetate, used as antiandrogenic drug in about 70% of our transwoman cohort, though further studies regarding this concern are needed.
Self-concept of assumable gender role could also be an explanation for the different proportion of smokers in transmen and transwomen. Remarkably, the proportion of smokers in our cohort of transmen was higher compared with young male Germans (44.54% vs 34.7%), whereas the proportion of transwomen smokers was lower compared with young female Germans (21.49% vs 31.3%).16 The higher rate of persons who stopped smoking in transwomen possibly also reflects certain awareness for cardiovascular and thromboembolic risks under feminizing hormone treatment. Our data provide good reasons to systematically advise individuals seeking for GAHT about potential risks of tobacco use and to offer support for smoking cessation. Use of illegal substances was recorded much less frequent than in a former study (<5% vs more than 40%).3
A minority of less than a third of our cohort stated that they are living in a permanent partnership, which is comparable to previous studies.2, 3, 7 Genetical-related parenthood was rare, and predominantly in transwomen. The very low share of parenthood in only about 2% of transmen probably relates to the denial of carry out a pregnancy, perceived as an epitome of feminity, since egg donation and surrogacy are illegal in Germany. This assumption is further supported by a recent analysis in another cohort of German individuals diagnosed with gender dysphoria showing also a significantly higher rate of genetical-related children in transwoman compared with transmen (31.5% vs 10.9%).17 Notably, the proportion of individuals with genetical-related children in this study is two to five times higher compared with our cohort. We explain these differences with the higher median age of the study cohort (median age transwomen 41 years vs 25 years in our cohort, median age transmen 33 years vs 21 years in our cohort).
By evaluating data for academic and occupational success, we could also find a remarkable difference between individuals diagnosed with gender dysphoria and the general population. In comparison to the German population above 15 years of age, proportion of those achieving graduation diploma was almost reduced by half (14.3% vs 27.3%),18 albeit these results are limited by a relatively high amount of missing data. Unemployment rate was more than twice as high as in the general population of Germany (14% vs 6.9%).19 It appears that individuals diagnosed with gender dysphoria are still limited in their opportunities and cannot realize their full potential, either by internal factors such as depressive comorbidity, external constraints or–most probably–a combination of both. Therefore, our data emphasize the need for support and encouragement of individuals diagnosed with gender dysphoria by mental health professionals.
A retrospective analysis from data of a single centre study is certainly not free of limitations. Treatment in our outpatient clinic is performed by a small team of trained physicians under supervision of one senior staff member and following a defined structure according to the clinical practice guideline. Nevertheless, the evaluability of some data is aggravated by the lack of specified, precise definitions and differing rates of missing informations in medical files. Ascertainments of data about drug use or preceding self-medication, if retrospective or prospective, are limited by a tendency to under-report potentially disqualifying informations. We cannot completely exclude that this leads to false low rates of illegal drug use in our cohort. Nevertheless, the differences to former results are apparent. Recent or ongoing self-medication with gender-affirming hormones can be easily detected by an examination of hormone levels which we perform regularly at the first visit in our outpatient clinic. We therefore assess our data about that topic as valid. Despite these possible limitations, evaluating a large, well-established German Endocrine outpatient clinic for gender dysphoria, covering an area with a radius of about 200 km and more than 500 individuals, we assess our data about this increasingly important topic as informative.
The overall very high level of individuals who appraised GAHT as an improvement of their overall situation as well as the absence of misdetermination in our cohort point out that individuals diagnosed with gender dysphoria benefit from a procedure according to the established standards of care and best-practice guideline. The declining use of illegal substances, the diminishing proportion of self-medication with gender-affirming hormones as well as the remarkable reduction of antidepressant co-medication observed at least in transmen could be interpreted as possible signs for a decline of psychosocial burden in individuals diagnosed with gender dysphoria over the last years.
An important result of our study, which to our knowledge has never been addressed before, concerns latency between application for legal gender reassignment and court decision. The median time for this process was nine months. In contrast to the well-defined, international developed recommendations for diagnosis and gender-affirming medical treatment, there are still considerable differences regarding admission requirements and legal aspects of gender reassignment between different countries even within the European Union. In Germany, legal gender assignment is regulated by the 1981 ‘German Transsexual Act (TSG)’. The decision is up to the jurisdiction of the responsible district court, and two mutually independent and fee-based expert opinions are required. The justifying reasons for the comparably complex and expensive procedure are incomprehensible, especially taking into account the high grade of satisfaction with gender reassignment, the marginal share of misdeterminations as well as the abated occupational and financial capacities of persons concerned, which we have validated with this study.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
ETHICAL APPROVAL
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethical committee of Goethe-University Hospital Frankfurt, Germany (permit no.185/16). For this type of retrospective analysis, formal consent is not required.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.